Sacrodinia (pain in the sacrum)
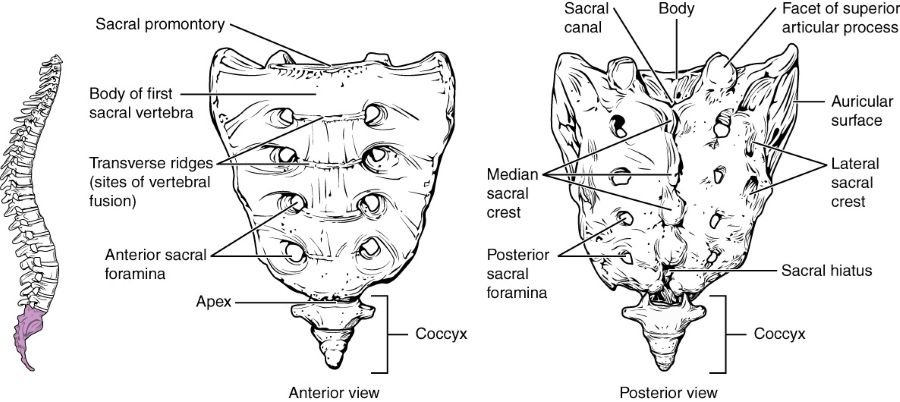
Anatomy of the Sacral Bone (Sacrum)
The sacrum is a large, triangular bone located at the base of the spine, situated between the two hip bones (ilia) of the pelvis. It is formed by the fusion of typically five sacral vertebrae (S1-S5). This fusion process is not complete at birth but occurs progressively throughout childhood and adolescence.
Development and Gender Differences
The fusion of the sacral vertebrae into a single sacral bone occurs relatively late in development, generally between the ages of 18 and 25 years. The process typically begins after 15 years of age with the fusion of the three lower sacral vertebrae (S3-S5), and by approximately age 25, the two upper sacral vertebrae (S1-S2) also fuse with the lower segments and with each other. There are some anatomical differences in the sacrum between sexes: the sacrum in males is generally longer, narrower, and more curved than in females, reflecting adaptations for childbirth in the female pelvis.
In cases of incomplete fusion of the sacral vertebrae or associated congenital developmental anomalies, conditions such as spina bifida occulta (non-closure of the vertebral arches), transitional vertebrae like sacralization of the L5 vertebra (fusion of L5 to S1) or lumbarization of the S1 vertebra (separation of S1 from the sacrum), or even more severe neural tube defects like meningocele or meningomyelocele (protrusion of spinal membranes with or without spinal cord tissue through a defect in the vertebral arch) can be detected.
Sacroiliac Joint
The lateral surfaces of the sacrum feature auricular (ear-shaped) articular surfaces. These surfaces articulate with corresponding auricular surfaces on the iliac bones of the pelvis, forming the sacroiliac (SI) joints. The sacroiliac joint is a strong, relatively immobile synovial joint (though it has some characteristics of an amphiarthrosis) that is critical for transferring weight from the upper body to the lower limbs. It is heavily reinforced by strong ligaments, making it a very rigid formation, often referred to as the sacroiliac junction rather than a highly mobile joint.
Inflammation of the sacroiliac joint (sacroiliitis), particularly in its acute stage, is a common cause of pain localized to the sacrum, a condition known as sacrodynia.
Understanding Sacrodynia (Pain in the Sacrum)
Sacrodynia is a medical term referring to pain localized in the sacral region (the area of the sacrum bone at the base of the spine and between the buttocks). This pain can arise from a variety of underlying conditions affecting the lumbosacral spine, sacroiliac joints, or adjacent pelvic structures.
Common Causes of Sacral Pain
Pain in the sacrum (sacrodynia) can occur with several conditions:
- Lumbosacral Spine Pathologies:
- Osteochondrosis of the lumbosacral spine (degenerative disc disease affecting the lower lumbar and L5-S1 discs).
- Spondylolisthesis (instability of the spine with displacement of vertebral bodies, often L5 on S1).
- Herniated discs at L4-L5 or L5-S1 impinging on sacral nerve roots.
- Congenital anomalies in the development of the lumbosacral spine, such as sacralization (fusion of L5 to S1), lumbarization (S1 behaving as an L6 vertebra), or non-closure of the vertebral arches (spina bifida occulta), which can alter biomechanics and lead to pain.
- Sacroiliac Joint Disorders:
- Sacroiliitis (inflammation of the sacroiliac joint), which can be due to spondyloarthropathies like ankylosing spondylitis, psoriatic arthritis, reactive arthritis, or enteropathic arthritis.
- Osteoarthritis of the sacroiliac joint (degenerative changes).
- Sacroiliac joint sprain or instability (e.g., postpartum or post-traumatic).
- Pelvic Organ Pathologies (Referred Pain):
- Inflammation of the peri-uterine tissue (parametritis).
- Compaction or inflammation of the sacro-uterine ligaments.
- Other pathological processes in adjacent areas of the pelvic organs, such as endometriosis, pelvic inflammatory disease, prostatitis, or tumors.
- Pain in the sacrum is also frequently reported after gynecological manipulations and operations.
- Trauma: Direct contusions, fractures of the sacrum or coccyx (coccygodynia can sometimes refer pain superiorly).
- Infections: Osteomyelitis of the sacrum (rare).
- Tumors: Primary bone tumors of the sacrum (e.g., chordoma, giant cell tumor) or metastatic disease to the sacrum.
- Myofascial Pain: Trigger points in gluteal muscles, piriformis muscle (piriformis syndrome can refer pain to sacral area).
Characteristics of Sacral Pain
The pain associated with sacrodynia often increases with certain activities or postures:
- When sitting for prolonged periods.
- When getting up quickly from a seated position.
- When bending the body forward.
- When lifting weights.
Pain can also radiate from the sacrum to the lower back, buttocks, groin, or down the legs, sometimes mimicking sciatica. The character of the pain can be dull, aching, sharp, or burning, depending on the cause.
Diagnosis of Pain in the Sacrum (Sacrodynia)
The diagnosis of sacrodynia is based on a thorough evaluation aimed at excluding or confirming the various potential sources of pain in the sacrum. This involves differentiating pathology of the lumbosacral spine and sacroiliac joints from diseases of the pelvic organs and other conditions.
Key diagnostic steps include:
- Detailed Medical History: Onset, duration, location, character, radiation, aggravating and relieving factors of the pain. History of trauma, systemic diseases, previous surgeries, and (in women) gynecological history.
-
Physical Examination:
- Inspection for deformity, swelling, or skin changes over the sacrum and lower back.
- Palpation for tenderness over the sacrum, sacroiliac joints, lumbosacral spine, and surrounding muscles (e.g., gluteal, piriformis).
- Assessment of lumbar spine range of motion.
- Specific provocative tests for sacroiliac joint pain (e.g., FABER test, Gaenslen's test, thigh thrust, sacral thrust, compression/distraction tests).
- Neurological examination of the lower extremities to assess for nerve root involvement (strength, sensation, reflexes, straight leg raise).
- Rectal examination may be indicated to assess for coccygeal tenderness or pelvic masses.
- Pelvic examination in women if gynecological causes are suspected.
-
Imaging Studies:
- X-rays of the Lumbosacral Spine and Pelvis: Can reveal fractures, degenerative changes (osteochondrosis, spondyloarthrosis), spondylolisthesis, congenital anomalies (spina bifida, transitional vertebrae), signs of sacroiliitis (erosions, sclerosis), or bone tumors.
- Computed Tomography (CT) Scan of the Lumbosacral Spine and Pelvic Bones: Provides more detailed bony anatomy than X-rays. It helps to exclude sacroiliitis or arthrosis of the sacroiliac joints. CT also makes it possible to rule out an oncological nature of lesions affecting the pelvic bones or vertebral bodies in the patient.
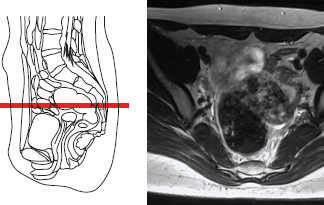
- Magnetic Resonance Imaging (MRI) of the Lumbosacral Spine and/or Pelvis: Excellent for visualizing soft tissues, including intervertebral discs (herniations), nerve roots, ligaments, muscles, bone marrow (for edema indicating inflammation like sacroiliitis or osteomyelitis), and pelvic organs. MRI of the pelvic organs in a woman is often prescribed to exclude sources of pain in the sacrum (sacrodynia) such as inflammation of the peri-uterine tissue (parametritis), hardening or inflammation of the sacro-uterine ligaments, endometriosis, or ovarian pathology.
- Bone Scan (Scintigraphy): Can detect areas of increased bone turnover, helpful in identifying stress fractures, infections, tumors, or inflammatory arthritis.
- Laboratory Tests: Blood tests for inflammatory markers (ESR, CRP), HLA-B27 (if spondyloarthropathy is suspected), infection markers, or tumor markers if indicated.
- Diagnostic Injections: Fluoroscopically or ultrasound-guided injections of local anesthetic into the sacroiliac joint or around suspected nerve roots can help confirm the source of pain if significant relief is achieved.
Sacrodynia in a patient should be distinguished from traumatic injuries of the sacrum, primary inflammatory sacroiliitis, osteomyelitis, and primary or metastatic tumors affecting this localization.
Computed tomography (CT) of the pelvic bones (including the sacrum and ilium) performed for sacral pain (sacrodynia) enables physicians to exclude oncological lesions or occult fractures affecting these bones or adjacent vertebral bodies in the patient.
Magnetic Resonance Imaging (MRI) of the pelvic organs in a female patient is often prescribed to exclude gynecological sources of pain in the sacrum (sacrodynia), such as inflammation of peri-uterine tissue (parametritis), pathology or hardening of the sacro-uterine ligaments, endometriosis, or other conditions.
Treatment of Pain in the Sacrum (Sacrodynia)
The treatment of sacrodynia is directed at the underlying cause identified during the diagnostic workup. If the pain is determined to be related to osteochondrosis of the lumbosacral spine or sacroiliac joint dysfunction, and after excluding gynecological or other significant pelvic organ pathology, the treatment approach is often similar to that for other forms of mechanical or inflammatory low back pain.
Depending on the severity of manifestations and the specific causes of pain in the sacrum with sacrodynia, the following therapeutic actions are possible:
Conservative Management
- Pharmacological Therapy:
- NSAIDs (Nonsteroidal Anti-Inflammatory Drugs): To reduce pain and inflammation (e.g., ibuprofen, naproxen, diclofenac).
- Analgesics: Acetaminophen or, for more severe pain, other pain relievers as prescribed.
- Muscle Relaxants: If significant muscle spasm in the gluteal or paraspinal region is contributing to pain.
- Hormones (Corticosteroids): Oral corticosteroids are generally not used for uncomplicated sacrodynia but may be considered for severe inflammatory conditions like acute sacroiliitis. More commonly, corticosteroids are administered via targeted injections.
- Physical Therapy (Physiotherapy):
- Exercises to improve flexibility, strength, and stability of the lumbopelvic region (core strengthening, gluteal strengthening, stretching).
- Postural correction and education on body mechanics.
- Modalities such as heat, cold, ultrasound, TENS (Transcutaneous Electrical Nerve Stimulation), or UHF (Ultra-High Frequency) therapy to alleviate pain and muscle spasm.
- Manual Therapy: Techniques such as mobilization or manipulation of the sacroiliac joints or lumbar spine, soft tissue mobilization (massage), and specific muscle energy or radicular techniques (if nerve irritation is present) may be employed by qualified practitioners.
- Acupuncture (Reflexotherapy): Can be beneficial for pain relief in some individuals with sacrodynia.
In the treatment of sacral pain (sacrodynia), physiotherapy focused on the lower back and buttocks can accelerate the elimination of inflammation and soreness, and help restore the normal range of motion in the muscles and joints of this region.
Interventional Pain Management
- Therapeutic Injections (Blockades):
- Sacroiliac Joint Injections: Injection of local anesthetic and a corticosteroid directly into the sacroiliac joint under imaging guidance (fluoroscopy or ultrasound) can be both diagnostic and therapeutic for sacroiliitis or SI joint arthrosis.
- Epidural Steroid Injections: If pain is referred from lumbar disc pathology or spinal stenosis affecting sacral nerve roots.
- Trigger Point Injections: For myofascial pain originating from gluteal or piriformis muscles.
- Radiofrequency Ablation (RFA): For chronic SI joint pain unresponsive to injections, RFA of the sensory nerves supplying the SI joint may be considered.
Supportive Measures (Bracing)
Wearing a semi-rigid lumbosacral brace or a specific sacroiliac belt can help to limit painful motion in the lumbar spine and sacroiliac joints. This can reduce pain in the area of sacral inflammation during sacrodynia and relieve excessive protective tension and spasm of the muscles of the lower back and buttocks. In such a brace, the patient can often move more comfortably at home and outdoors, and manage sitting in a car or at their workplace. The need for a corset or SI belt typically diminishes as the pain in the sacrum associated with sacrodynia subsides. There are several types of semi-rigid lumbosacral braces and SI belts; all are selected by size and can be used repeatedly in case of recurrent pain in the sacrum region.
Wearing a specialized sacroiliac brace can be beneficial in the treatment of sacroiliac pain (sacrodynia) and arthrosis of the sacroiliac joint by providing compression and support to the joint.
This is a variant of a semi-rigid lumbosacral brace, which can help in the treatment of pain in the sacrum (sacrodynia) when related to issues in the lower lumbar spine or sacroiliac region.
Surgical Treatment (Rarely for isolated sacrodynia)
Surgical intervention for isolated sacrodynia (pain primarily from the sacrum or SI joints without significant lumbar pathology) is rare. It might be considered in cases of:
- Severe, debilitating sacroiliac joint pain unresponsive to all conservative and interventional measures (SI joint fusion may be an option).
- Symptomatic sacral tumors requiring excision.
- Unstable sacral fractures.
- Severe spondylolisthesis directly impacting the sacrum and causing intractable pain or neurological deficits.
If sacrodynia is secondary to significant lumbar spine pathology (e.g., large disc herniation compressing sacral nerves), then surgical treatment would address the primary lumbar issue.
Differential Diagnosis of Sacral Pain
Pain in the sacral region can originate from various sources. A thorough differential diagnosis is crucial:
| Condition | Key Differentiating Features |
|---|---|
| Sacroiliitis (Inflammatory or Degenerative) | Pain localized to SI joint, buttock, may refer to posterior thigh. Positive SI joint provocative tests. Imaging shows SI joint inflammation or degeneration (arthrosis). |
| Lumbar Spine Pathology (e.g., Disc Herniation, Stenosis, Spondylolisthesis) | May have low back pain with radiation into sacrum and/or legs (sciatica). Neurological signs may be present. MRI/CT of lumbar spine diagnostic. |
| Coccygodynia (Tailbone Pain) | Pain localized to the coccyx, worse with sitting or direct pressure. Can sometimes refer to sacral area. |
| Myofascial Pain (Gluteal, Piriformis) | Pain from trigger points in gluteal or piriformis muscles can refer to the sacrum. Tenderness over specific muscles. |
| Sacral Stress Fracture or Acute Fracture | History of trauma or repetitive stress (e.g., athletes, osteoporosis). Localized sacral tenderness. Imaging (X-ray, CT, MRI, bone scan) confirms. |
| Pelvic Organ Disease (Gynecological, Urological, Gastrointestinal) | Pain often deep, aching, may be cyclical (e.g., endometriosis). Associated symptoms related to the involved organ system. Pelvic examination and imaging (ultrasound, MRI) important. |
| Sacral Tumors (Primary or Metastatic) | Persistent, often progressive pain, may be worse at night. Neurological symptoms if nerve roots involved. History of cancer. Imaging (CT/MRI, bone scan) and biopsy for diagnosis. |
| Sacral Osteomyelitis / Infection | Localized pain, tenderness, fever, elevated inflammatory markers. Risk factors (IV drug use, diabetes, recent surgery). MRI diagnostic. |
Prevention and When to Consult a Specialist
While not all causes of sacrodynia are preventable, maintaining good spinal health through regular exercise, proper posture, and avoiding activities that excessively strain the lower back and pelvis can be beneficial.
Consultation with a physician (e.g., general practitioner, neurologist, neurosurgeon, orthopedic spine specialist, gynecologist, or rheumatologist, depending on suspected cause) is recommended if:
- Sacral pain is severe, persistent, or progressively worsening.
- Pain is associated with trauma.
- There are "red flag" symptoms such as unexplained weight loss, fever, night sweats, or new neurological deficits (weakness, numbness, bowel/bladder changes).
- Pain significantly impacts daily activities or sleep.
- Conservative self-care measures fail to provide relief.
- There is a history of cancer or systemic inflammatory disease.
An accurate diagnosis by a specialist is key to developing an effective treatment plan for sacrodynia.
References
- Cohen SP, Chen Y, Neff N. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2013 Mar;116(3):695-710.
- Forst SL, Wheeler MT, Fortin JD, Vilensky JA. The sacroiliac joint: anatomy, physiology and clinical significance. Pain Physician. 2006 Jan;9(1):61-7.
- Slipman CW, Jackson HB, Lipetz JS, et al. Sacroiliac joint pain referral zones. Arch Phys Med Rehabil. 2000 Mar;81(3):334-8.
- Bernard TN, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop Relat Res. 1987 Mar;(217):266-80. (Context for lumbosacral pain origins)
- Sembrano JN, Polly DW Jr. Sacroiliac joint syndrome. Mayo Clin Proc. 2009 Jan;84(1):93-4.
- Hansen HC, McKenzie-Brown AM, Cohen SP, et al. Sacroiliac joint interventions: a systematic review. Pain Physician. 2007 Jan;10(1):165-84.
- Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012 Dec;221(6):537-67.
See also
- Anatomy of the spine
- Ankylosing spondylitis (Bechterew's disease)
- Back pain by the region of the spine:
- Back pain during pregnancy
- Coccygodynia (tailbone pain)
- Compression fracture of the spine
- Dislocation and subluxation of the vertebrae
- Herniated and bulging intervertebral disc
- Lumbago (low back pain) and sciatica
- Osteoarthritis of the sacroiliac joint
- Osteocondritis of the spine
- Osteoporosis of the spine
- Guidelines for Caregiving for Individuals with Paraplegia and Tetraplegia
- Sacrodinia (pain in the sacrum)
- Sacroiliitis (inflammation of the sacroiliac joint)
- Scheuermann-Mau disease (juvenile osteochondrosis)
- Scoliosis, poor posture
- Spinal bacterial (purulent) epiduritis
- Spinal cord diseases:
- Spinal spondylosis
- Spinal stenosis
- Spine abnormalities
- Spondylitis (osteomyelitic, tuberculous)
- Spondyloarthrosis (facet joint osteoarthritis)
- Spondylolisthesis (displacement and instability of the spine)
- Symptom of pain in the neck, head, and arm
- Pain in the thoracic spine, intercostal neuralgia
- Vertebral hemangiomas (spinal angiomas)
- Whiplash neck injury, cervico-cranial syndrome