Whiplash neck injury, cervico-cranial syndrome
- Understanding Whiplash Neck Injury and Cervico-Cranial Syndrome
- Classification of Subaxial Cervical Spine Injuries
- Diagnosis of Whiplash Injury and Cervico-Cranial Syndrome
- Treatment of Whiplash Injury and Cervico-Cranial Syndrome
- Differential Diagnosis of Neck Pain and Associated Symptoms Post-Trauma
- Prognosis and Potential Complications
- Prevention and When to Seek Specialist Care
- References
Understanding Whiplash Neck Injury and Cervico-Cranial Syndrome
Whiplash neck injury, often leading to a constellation of symptoms termed cervico-cranial syndrome (or sometimes post-whiplash syndrome, whiplash-associated disorders - WAD), is a common consequence of sudden acceleration-deceleration forces acting on the head and neck. This typically occurs in motor vehicle accidents (especially rear-end collisions) but can also result from sports injuries, falls, or direct blows to the head or neck.
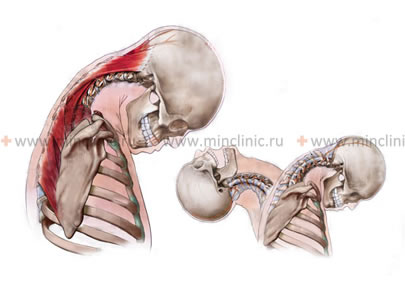
Definition and Mechanism of Injury
Cervico-cranial syndrome describes a painful condition affecting the cervico-occipital junction (where the base of the skull meets the upper cervical spine) and the broader cervical spine. It results from acute injury or, less commonly, chronic overload of this region. The injury mechanism involves irritation and damage to pain receptors located in the ligamentous apparatus, the capsules of the intervertebral (facet) joints, the muscles of the cervical spine, and the aponeurosis (fascia) in the occipital part of the skull.
The source of pain in the neck and back of the head is an injury or chronic overload of the supporting structures of this area. Injuries to the cervical spine can be acute or chronic:
- Acute Injury: Occurs due to a sudden traumatic event such as car accidents (whiplash), falls (bruised neck and back of the head), direct blows to the head, or collisions during activities like skiing, snowboarding, skating, or rollerblading. The whiplash mechanism involves a sharp, rapid movement of the head relative to the torso, typically in an anteroposterior (flexion-extension) or lateral direction, causing hyperextension followed by hyperflexion, or vice versa.
- Chronic Overload/Trauma: Can develop from sustained static loads due to monotonous efforts over a long period (e.g., prolonged sedentary work with poor posture, repetitive occupational movements, or activities like extended breastfeeding or carrying a child in the arms).
The whiplash mechanism involves injury to the ligaments and muscles of the neck, and potentially a mild traumatic brain injury (concussion), during sudden forceful movements of the head, such as in a car accident, collisions during sports (skating, rollerblading, skiing, snowboarding), or a fall causing a bruised neck and back of the head.
Pathophysiology and Affected Structures
During an acute whiplash injury of the cervical spine, the rapid and forceful movement at the cervico-occipital junction and intervertebral joints can exceed the physiological range of motion. This results in stretching, spraining, or tearing of various soft tissue structures:
- Ligaments of the cervical spine (e.g., anterior longitudinal ligament, posterior longitudinal ligament, interspinous ligaments, facet joint capsules).
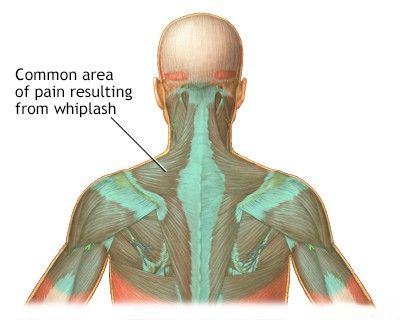
- Muscles of the neck (posterior, anterior, and lateral groups, including sternocleidomastoid, scalenes, trapezius, levator scapulae, and deep neck flexors/extensors) and their tendinous attachments.
- Intervertebral discs (annular tears or, less commonly, acute herniations).
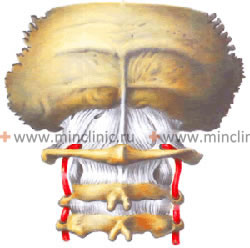
- Facet joints (zygapophyseal joints), which can be sprained or develop synovitis.
In more severe cases, the movement can be greater than the physiological norm for the cervical spine, potentially leading to subluxation or dislocation of intervertebral joints, fractures of vertebral bodies or processes, or injury to the odontoid process of the C2 vertebra (axis). Damage to nerve roots or the spinal cord itself can also occur in severe trauma.
Chronic trauma or overload, often due to poor posture or repetitive strain, leads to microtrauma, muscle imbalances, chronic inflammation, and eventually degenerative changes in the cervical spine (cervical osteochondrosis, spondylosis).
Associated Symptoms: Beyond Neck Pain
Depending on the intensity of pain in the back of the head and neck following an injury or contusion of the cervical spine, the patient may have difficulty finding a comfortable sleeping position. Chronic static load from monotonous efforts over a long period (e.g., sedentary work) often leads to discomfort in the neck and back of the head that may be present for some time before an acute exacerbation. Such exacerbations of pain in the cervical spine can be triggered by hypothermia, a sudden head movement (turning the head to the side or back), or maintaining an uncomfortable neck position during sleep.
Against the background of whiplash and pain in the cervical spine, irritation of the vertebral arteries can occur. These arteries pass through foramina in the transverse processes of the cervical vertebrae and are susceptible to compression or spasm due to muscle tension, inflammation, or instability.
It should be noted that in addition to pain in the neck and head (occiput, temples, crown, forehead), patients with cervico-cranial syndrome may also experience **vestibular disorders**. These are often attributed to irritation or compromised blood flow in the vertebral arteries (vertebrobasilar insufficiency) and can manifest as:
- Dizziness (vertigo or lightheadedness)
- Unsteadiness when walking (ataxia or dysequilibrium)
- Nausea and vomiting
Sometimes, the clinical manifestations of cervico-cranial syndrome, particularly the headache, dizziness, and cognitive symptoms, can lead to an erroneous diagnosis of a concussion (mild traumatic brain injury), especially if a direct head impact also occurred. While concussion can coexist, many symptoms may be primarily cervicogenic.
Other associated symptoms of cervico-cranial syndrome can include:
- Tinnitus (noise or ringing in the ears) and other cochlear manifestations.
- Numbness or paresthesia (tingling) of the skin of the face, back of the head, or in the ear region.
- Numbness or altered sensation on the mucous membrane of the tongue.
- Rapid fatigability.
- Non-restorative sleep (waking up feeling unrefreshed).
- Insomnia (difficulty sleeping).
- Decreased general performance and attention.
- Irritability and mood changes.
Classification of Subaxial Cervical Spine Injuries
Subaxial cervical spine injuries refer to injuries occurring from the C3 to C7 vertebrae. Various classification systems exist to categorize these injuries based on the mechanism of injury and radiographic findings, which helps guide treatment decisions. One common clinical classification includes:
- Compression Fracture: Typically involves failure of the anterior column of the vertebra due to axial loading in flexion.
- Explosive (Burst) Fracture: Results from high-energy axial loading, causing comminution of the vertebral body with potential retropulsion of fragments into the spinal canal.
- Flexion-Distraction Injury (Chance-type injury of the neck): Involves failure of all three spinal columns (anterior, middle, posterior) under tension, often due to sudden deceleration with a fulcrum (e.g., seatbelt).
- Dislocation of Articular Processes (Facet Joints): Can be unilateral or bilateral, resulting from flexion-rotation or severe flexion forces. This leads to significant instability.
- Fracture of the Articular Processes (Facet Fracture): Can occur in isolation or with dislocations.
The Allen and Ferguson classification is another system used in specialized literature, based on X-ray data and the predominant mechanism of injury for subaxial (C3-C7) cervical spine injuries:
- Flexion-Compression: Different stages describe increasing severity of anterior vertebral body compression and posterior ligamentous injury.
- Vertical Compression: Leads to burst fractures.
- Flexion-Distraction: Includes various degrees of injury:
- Subluxation of the articular process (facet joint).
- Unilateral dislocation of the articular processes.
- Bilateral dislocation of the articular processes with 50% anterior displacement of the superior vertebra.
- Complete dislocation (100% displacement).
- Extension-Compression: Can cause fractures of posterior elements.
- Extension-Distraction: Can lead to anterior ligamentous injury or hyperextension dislocations.
- Lateral Flexion: Can cause wedge compression fractures or ligamentous injury on one side.
These classifications help surgeons understand the pattern of injury, assess stability, and plan appropriate management, which may range from conservative (e.g., bracing) to surgical stabilization.
Diagnosis of Whiplash Neck Injury and Cervico-Cranial Syndrome
Diagnosing an injury or contusion of the neck (cervical spine) and the associated cervico-cranial syndrome requires a comprehensive evaluation, starting with a consultation with a physician (e.g., neurologist, neurosurgeon, orthopedic specialist, or physiatrist) for a thorough neurological and musculoskeletal examination. This assessment should evaluate the biomechanics of the cervical spine, including range of motion, muscle tone and strength, and the presence of myofascial trigger points or fibromyalgia-like tenderness in the muscles of the neck and surrounding areas.
Clinical Examination and Neurological Assessment
A neurological examination of a patient with a neck injury may reveal:
- Symptoms of Monoradiculopathy: If a single nerve root is compressed or irritated. For example:
- Unilateral dislocation of the articular processes at the C5-C6 vertebral level usually manifests as C6 radiculopathy. In this case, the patient may complain of muscle weakness when extending the wrist (wrist extensors) or flexing the elbow (biceps, brachioradialis), along with numbness and tingling in the thumb, index finger, and lateral forearm.
- Unilateral dislocation of the articular processes at the C6-C7 vertebral level typically manifests as C7 radiculopathy. Symptoms include muscle weakness when extending the arm at the elbow (triceps), flexing the wrist, or extending the fingers, as well as numbness and tingling in the index, middle, and sometimes ring fingers.
- Symptoms of Spinal Cord Compression (Myelopathy): Neurological symptoms of spinal cord compression can occur with bilateral dislocations of the cervical vertebrae, severe fractures, or large disc herniations. These symptoms can worsen with increasing subluxation or instability. Myelopathy signs include upper motor neuron findings like spasticity, hyperreflexia, Babinski's sign below the level of injury, gait disturbance, and potentially bowel/bladder dysfunction.
The pattern of segmental innervation on the surface of the human body (dermatomes for sensation, myotomes for muscle function) helps clinicians in clarifying the localization and level of radiculopathy (nerve root injury) or spinal cord compression.
Video demonstrating a neurological examination, which is a key component in diagnosing neck injuries and cervico-cranial syndrome.
Imaging and Other Diagnostic Procedures
Based on the results of the clinical examination, if the diagnosis remains unspecified or if serious injury is suspected, additional diagnostic procedures may be ordered:
- Vascular Studies (REG, Doppler Ultrasound): Rheoencephalography (REG) or Doppler ultrasound of the neck (carotid and vertebral arteries) and brain vessels may be performed to assess blood flow, especially if symptoms like dizziness, tinnitus, or unsteadiness suggest vertebral artery involvement or vertebrobasilar insufficiency.
- X-ray of the Cervical Spine: Standard views (anteroposterior, lateral, odontoid) are often the initial imaging study. Functional X-rays (flexion and extension views) can help assess for ligamentous instability or abnormal movement between vertebrae.
- Computed Tomography (CT) of the Cervical Spine: Provides excellent detail of bony structures and is superior to X-rays for detecting fractures, especially complex ones involving posterior elements or facet joints. CT angiography (CTA) can visualize the vertebral arteries.
- Magnetic Resonance Imaging (MRI) of the Cervical Spine: The best imaging modality for visualizing soft tissues, including intervertebral discs (herniations, tears), ligaments, muscles, the spinal cord (for contusion, edema, or compression), and nerve roots. It is crucial for diagnosing conditions like disc herniation causing radiculopathy or myelopathy.
- Electromyography (EMG) and Nerve Conduction Studies (NCS): May be used to confirm nerve root damage (radiculopathy) or peripheral nerve injury if suspected.
Magnetic Resonance Imaging (MRI) of the cervical spine (lateral or sagittal view shown) is invaluable in diagnosing damage to intervertebral discs, ligaments, and the spinal cord, as well as determining the precise position and alignment of cervical vertebrae, especially when they are displaced due to injury.
Treatment of Whiplash Neck Injury and Cervico-Cranial Syndrome
The management of whiplash injuries and cervico-cranial syndrome is typically conservative initially, focusing on pain relief, reducing inflammation, restoring range of motion, and facilitating recovery. A multimodal approach is often most effective.
Conservative Management
- Rest and Activity Modification: Relative rest for a short period (1-2 days) may be helpful for acute, severe pain, but prolonged immobilization is generally discouraged. A gradual return to normal activities as tolerated is encouraged.
- Ice and Heat Therapy: Ice application during the first 24-48 hours can help reduce acute inflammation and swelling. Heat therapy (e.g., warm packs, heating pad) can be used later to relax tense muscles and alleviate stiffness.
Pharmacological Therapy
- Analgesics: Over-the-counter pain relievers like acetaminophen or NSAIDs (e.g., ibuprofen, naproxen) are often sufficient for mild to moderate pain.
- NSAIDs (Nonsteroidal Anti-Inflammatory Drugs): Help to reduce pain and inflammation. Prescription-strength NSAIDs may be used for more severe pain.
- Muscle Relaxants: May be prescribed for short-term use to alleviate muscle spasms, particularly if they contribute significantly to pain and stiffness.
- Neuropathic Pain Medications: If radicular pain or persistent neuropathic symptoms develop, medications like gabapentin, pregabalin, or tricyclic antidepressants may be considered.
- Hormones (Corticosteroids - Rarely Used Systemically): Oral corticosteroids are generally not indicated for uncomplicated whiplash but might be considered in very specific, severe inflammatory situations by a specialist. Local steroid injections are more common (see below).
Therapeutic Injections
If pain is severe or persistent despite conservative measures, targeted injections may be considered, often performed under imaging guidance:
- Trigger Point Injections: Injection of local anesthetic (e.g., Novocaine/procaine, Lidocaine) with or without a corticosteroid (e.g., Cortisone, Diprospan/betamethasone, Kenalog/triamcinolone) into painful myofascial trigger points in the neck and shoulder muscles.
- Cervical Epidural Steroid Injections: For radicular pain due to nerve root inflammation.
- Cervical Facet Joint Injections or Medial Branch Blocks: If facet joint pain is suspected. Sufficiently low doses of anesthetic and corticosteroid are injected into the lumen or soft tissues near the affected joint.
- Occipital Nerve Blocks: For cervicogenic headaches originating from the greater or lesser occipital nerves.
When combined with a properly selected physiotherapy regimen, these injections can have a good and long-term effect on headaches and neck pain following a cervical spine injury.
The application of physiotherapy plays a crucial role in treating cervical spine injuries by helping to eliminate swelling (puffiness) and inflammation, alleviate soreness, and restore the normal range of motion in the joints and muscles of the neck.
Manual Therapy and Physiotherapy
- Physiotherapy (Physical Therapy): A cornerstone of whiplash recovery. Includes:
- Gentle range-of-motion exercises for the neck.
- Stretching and strengthening exercises for neck and shoulder muscles.
- Postural education and correction.
- Modalities like TENS, ultrasound, heat/cold therapy.
- Manual therapy techniques (see below).
- Manual Therapy: Techniques such as joint mobilization, soft tissue mobilization, myofascial release, or specific osteopathic/chiropractic adjustments may be used by qualified practitioners to address joint restrictions and muscle dysfunction.
Acupuncture
Acupuncture may be helpful for some individuals in managing pain and muscle tension associated with whiplash injuries.
Cervical Collars and Braces
Wearing a special cervical brace (e.g., a soft Philadelphia collar) or a simpler cervical collar (Shantz splint) can limit the range of motion in stretched ligaments and injured joints of the neck in cases of cervico-cranial syndrome or acute whiplash injury. At the same time, a cervical corset or brace creates additional unloading of tense and protectively spasmodic neck muscles. With limited movement due to the collar, the pain symptom in the neck and back of the head often resolves much faster, leading to a quicker restoration of the previous range of motion. The duration of collar use depends on the severity of pain and is determined by the physician, typically ranging from a few days to a few weeks. It's generally recommended for short-term use to avoid muscle atrophy and dependence.
Wearing a neck brace, such as a Philadelphia collar, is part of the treatment for sprained ligaments and injured neck joints following an injury to the cervical spine, providing support and limiting motion.
A Philadelphia collar offers significant support and immobilization, aiding in the treatment of sprained ligaments and injured joints of the neck after cervical spine trauma.
Surgical Treatment (Rarely Indicated for Uncomplicated Whiplash)
Surgery is rarely needed for uncomplicated whiplash-associated disorders. It is reserved for cases with evidence of significant structural damage such as unstable fractures, dislocations, progressive neurological deficits due to spinal cord or nerve root compression from a large disc herniation or severe stenosis that has not responded to comprehensive conservative management.
Differential Diagnosis of Neck Pain and Associated Symptoms Post-Trauma
It is crucial to differentiate whiplash-associated disorders from more serious traumatic injuries or other conditions that can cause similar symptoms:
| Condition | Key Differentiating Features |
|---|---|
| Whiplash-Associated Disorder (WAD) / Cervico-Cranial Syndrome | History of acceleration-deceleration injury; neck pain, stiffness, headache, dizziness, muscle tenderness. Neurological exam often normal in mild cases. Imaging may be normal or show soft tissue injury. |
| Cervical Spine Fracture / Dislocation | Significant trauma; severe pain, deformity, point tenderness over bone, potential neurological deficits (radiculopathy, myelopathy). Requires X-ray/CT/MRI for diagnosis. |
| Cervical Disc Herniation (Traumatic or Pre-existing) | Neck pain with radiating arm pain, numbness, tingling, weakness in a dermatomal pattern. Provoked by certain neck movements. MRI confirms. |
| Mild Traumatic Brain Injury (Concussion) | Often coexists with whiplash if head impact occurred. Headache, dizziness, confusion, memory/concentration issues, sensitivity to light/noise, fatigue. Neurological exam often normal. |
| Vertebral Artery Dissection | Can occur after neck trauma/manipulation. Neck pain, occipital headache, vertigo, ataxia, visual changes, signs of stroke/TIA in posterior circulation. Requires urgent imaging (CTA/MRA). |
| Temporomandibular Joint (TMJ) Dysfunction | Can be exacerbated by whiplash. Jaw pain, clicking, limited opening, headache. |
| Post-Traumatic Headache (Non-Cervicogenic) | Headache as a primary symptom after head injury, may have features of migraine or tension-type headache. |
Prognosis and Potential Complications
The majority of individuals with mild to moderate whiplash injuries recover within a few weeks to months with conservative treatment. However, a subset of patients may develop chronic pain, stiffness, headaches, and other symptoms (chronic WAD or persistent post-whiplash syndrome). Factors that may predict a poorer prognosis include high initial pain intensity, significant psychological distress, pre-existing neck problems, and severe neurological symptoms at onset.
Potential complications, though mostly associated with more severe injuries initially misdiagnosed as simple whiplash, can include:
- Chronic neck pain and headaches.
- Persistent dizziness or balance problems.
- Cervical radiculopathy or myelopathy (if disc herniation or instability is present).
- Temporomandibular joint (TMJ) disorders.
- Psychological sequelae (anxiety, depression, post-traumatic stress disorder).
Prevention and When to Seek Specialist Care
Prevention of whiplash injuries often involves safe driving practices, proper use of headrests in vehicles, and appropriate protective gear in sports.
It is important to seek medical attention after any significant neck injury, especially if:
- There was a high-impact trauma (e.g., motor vehicle accident, significant fall).
- Pain is severe or rapidly worsening.
- There are any neurological symptoms such as radiating arm pain, numbness, tingling, weakness, or bowel/bladder dysfunction.
- Symptoms like severe headache, persistent dizziness, visual disturbances, or difficulty speaking/swallowing occur.
- Symptoms do not improve or worsen despite initial self-care measures.
- There is significant limitation of neck movement.
A specialist (e.g., neurologist, neurosurgeon, orthopedic spine specialist, physiatrist, or pain management physician) can perform a thorough evaluation, order appropriate imaging if necessary, and recommend a tailored treatment plan to ensure optimal recovery and rule out more serious injuries.
References
- Spitzer WO, Skovron ML, Salmi LR, et al. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining "whiplash" and its management. Spine (Phila Pa 1976). 1995 Apr 15;20(8 Suppl):1S-73S.
- Sterling M. Physiotherapy management of whiplash-associated disorders (WAD). J Physiother. 2014 Mar;60(1):5-12.
- Bogduk N, McGuirk B. Management of Acute and Chronic Neck Pain: An Evidence-Based Approach. Elsevier Health Sciences; 2006.
- Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc. 2015 Feb;90(2):284-99.
- Schofferman J, Bogduk N, Slosar P. Chronic whiplash and whiplash-associated disorders: an evidence-based approach. J Am Acad Orthop Surg. 2007 Oct;15(10):596-606.
- Barnsley L, Lord SM, Wallis BJ, Bogduk N. The prevalence of chronic cervical zygapophysial joint pain after whiplash. Spine (Phila Pa 1976). 1995 Jan 1;20(1):20-5.
- International Headache Society. The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018 Jan;38(1):1-211. (For cervicogenic headache criteria)
- Ferrara LA. The Biomechanics of Whiplash. Europa Medicophysica. 2002;38(3):129-135.
See also
- Anatomy of the spine
- Spine abnormalities
- Osteoarthritis of the sacroiliac joint
- Spondyloarthrosis (facet joint osteoarthritis)
- Spinal cord diseases:
- Ankylosing spondylitis (Bechterew's disease)
- Scheuermann-Mau disease (juvenile osteochondrosis)
- Low back pain (spinal pain)
- Symptom of pain in the neck, head, and arm
- Back pain during pregnancy
- Dislocation and subluxation of the vertebrae
- Vertebral hemangiomas (spinal angiomas)
- Herniated and bulging intervertebral disc
- Coccygodynia (tailbone pain)
- Lumbago (low back pain) and sciatica
- Osteoporosis of the spine
- Pain in the thoracic spine, intercostal neuralgia
- Osteocondritis of the spine
- Compression fracture of the spine
- Guidelines for Caregiving for Individuals with Paraplegia and Tetraplegia
- Sacrodinia (pain in the sacrum)
- Sacroiliitis (inflammation of the sacroiliac joint)
- Scoliosis, poor posture
- Spinal spondylosis
- Spondylitis (osteomyelitic, tuberculous)
- Spondylolisthesis (displacement and instability of the spine)
- Spinal stenosis
- Whiplash neck injury, cervico-cranial syndrome
- Spinal bacterial (purulent) epiduritis