Dislocation and subluxation of the vertebrae
- Understanding Vertebral Dislocation and Subluxation
- Diagnosis of Vertebral Dislocation and Subluxation
- Treatment of Vertebral Dislocation and Subluxation
- Differential Diagnosis of Acute Neck/Back Pain with Potential Instability
- Potential Complications
- Prevention and Prognosis
- When to Seek Urgent Medical Care
- References
Understanding Vertebral Dislocation and Subluxation
Definitions and Prevalence
Vertebral dislocation refers to a complete displacement of one vertebra relative to an adjacent vertebra, resulting in a loss of normal alignment and contact between their articular (facet) surfaces. Vertebral subluxation is a partial or incomplete dislocation, where there is still some contact between the articular surfaces but the alignment is abnormal. "Pure" dislocations (without associated fractures) are relatively rare phenomena in the spine. More commonly, vertebral dislocations are associated with concomitant vertebral fractures (fracture-dislocations).
In its pure form, without significant fracture, dislocations occur almost exclusively in the cervical spine due to its greater mobility and less inherent bony stability compared to the thoracic and lumbar regions. When a dislocation occurs, the upper vertebra is conventionally considered the dislocated one relative to the vertebra below it.
Mechanisms and Types of Cervical Dislocations
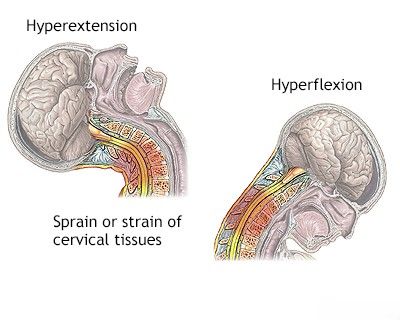
Cervical spine dislocations are typically caused by significant trauma involving excessive forces applied to the neck. Two main types are described based on the mechanism of injury:
Flexion Dislocations (Bilateral Facet Dislocation)
Excessive extension (bending backward) of the neck meets a natural obstacle as the vertebral arches (posterior bony elements) approach each other, which helps prevent posterior dislocation. However, excessive flexion (bending the head forward towards the chest) can lead to anterior displacement of the articular processes of the upper vertebra relative to those of the lower vertebra. Initially, this may result in an incomplete dislocation or subluxation. With subsequent straightening or further movement of the spine, the articular surfaces of the upper vertebra can slide further forward, "jumping" over and locking in front of the articular processes of the lower vertebra, resulting in a complete, bilateral facet dislocation. In this scenario, the head acts as a lever, with the fulcrum being on the anterior edges of the articular surfaces of the underlying vertebra. Therefore, flexion dislocations of the cervical vertebrae are almost always bilateral, involving complete rupture of the capsules of both intervertebral facet joints, as well as significant ligamentous injury (e.g., posterior longitudinal ligament, interspinous ligaments).
Excessive extension or flexion forces resulting from a neck injury (whiplash or direct trauma) can cause displacement (dislocation or subluxation) of the cervical vertebrae.
Rotational Dislocations (Unilateral Facet Dislocation)
Rotational dislocation occurs with excessive lateral flexion (side bending) combined with rotation. During this movement, the articular process of the upper vertebra on the side of lateral flexion may rest on the arch of the lower vertebra, acting as a fulcrum. With further movement, the articular processes on one side (the side of rotation and contralateral to the lateral flexion) can diverge and dislocate, similar to a flexion mechanism, resulting in an incomplete or complete unilateral facet dislocation. This typically involves rupture of the capsule of the intervertebral joint on the side of rotation. On the opposite side (the side of lateral flexion), during rotation, the upper articular process may move posteriorly relative to the lower vertebra due to stretching of the articular capsule. Thus, in rotational dislocation, the vertebrae are displaced on both sides but in opposite directions relative to each other. Because the "locking" or "engagement" of the articular processes occurs primarily on one side, rotational dislocation is often referred to as unilateral facet dislocation.
Both flexion and rotational dislocations are primarily observed in the cervical spine due to its horizontally oriented facet joints and greater mobility, typically resulting from a sharp or forceful bend of the neck.
When performing an X-ray of the cervical spine in the lateral projection, visualization of the lower cervical vertebrae (e.g., C6-C7) can be challenging as they may be obscured by the patient's shoulders, potentially hindering the assessment of vertebral body displacement after an injury. This image shows the upper 5 cervical vertebrae with an increased retropharyngeal space (6.1mm, normal up to 7mm in adults, up to 2/3 vertebral body width in children), which can indicate prevertebral soft tissue swelling.
Dislocations in Specific Cervical Regions (C1-C2)
Dislocations in the upper cervical spine, particularly at the C1-C2 level (atlantoaxial joint), are unique due to the absence of intervertebral discs and the specialized anatomy of these vertebrae. The joints here are wide and primarily stabilized by a powerful ligamentous apparatus.
- Atlanto-Occipital Dislocation (C0-C1): Dislocation of the skull (occiput) relative to the atlas (C1 vertebra) is an extremely severe and often fatal injury, usually resulting from high-energy trauma causing a sharp bend or rotation of the head.
- Atlantoaxial Dislocation (C1-C2): Dislocation of the atlas (C1) relative to the axis (C2 or epistropheus) is also a serious injury. The C2 vertebra has an odontoid process (dens) that articulates with the anterior arch of the atlas. This joint is stabilized by the transverse ligament, alar ligaments (pterygoid ligaments), and apical ligament (cruciate ligaments connecting to the anterior edge of the foramen magnum).
- If these ligaments rupture (e.g., during extreme neck flexion with traction, as in hanging), the C1 vertebra can displace anteriorly on C2. This can cause the odontoid process of C2 to compress or crush the spinal cord within the spinal canal, often leading to instant death or severe neurological deficit.
- If the odontoid process itself fractures and displaces anteriorly from the C1 arch, the spinal cord may not be as severely compressed if the C1 arch remains intact posteriorly.
- Hyperflexion injuries in this region can also lead to fractures of the vertebral bodies or articular processes.
Thoracic and Lumbar Spine Dislocations
Pure dislocations without fracture are very rare in the thoracic and lumbar spine due to their greater intrinsic stability:
- Thoracic Spine: The rib cage and vertically oriented facet joints provide significant stability, making it inactive relative to pure dislocations. Dislocations usually occur only in the context of severe trauma with associated fractures of adjacent (articulated) vertebrae.
- Lumbar Spine: More mobile than the thoracic spine but reinforced by powerful long and short ligaments. The range of motion during flexion is more pronounced than rotation or tilting. In the lumbar vertebrae, the articular processes (facets) are primarily oriented in the sagittal plane (though they have some coronal orientation), which resists anterior displacement. This anatomical feature, along with strong ligaments, generally prevents pure dislocation of lumbar vertebrae during flexion without an associated fracture (e.g., of the facet joints or pars interarticularis).
Spondylolisthesis (Chronic Sliding)
Chronic anterior slippage of the L5 vertebral body on the sacrum (S1) was first described by Killian as spondylolysis (a defect in the pars interarticularis) and spondylolisthesis (the actual slippage), and by Lambl as "spinal dislocation." Spondylolisthesis is often an inevitable consequence of a congenital defect (spondylolysis) in the development of the vertebral arches, most commonly found in the arch of the L5 vertebra. Clinical manifestations of this defect in the form of spondylolisthesis are often precipitated by sudden physical exertion, heavy lifting, or trauma. In women, repeated pregnancies can contribute to the gradual development or worsening of spondylolisthesis, as hormonal changes during pregnancy cause ligamentous softening, which increases the mobility of pelvic joints for childbirth but can also affect spinal ligamentous stability.
Diagnosis of Vertebral Dislocation and Subluxation
Clinical Symptoms and Signs
The clinical presentation depends on the level and severity of the dislocation and any associated neurological injury.
- Flexion Dislocation of the Cervical Spine:
- The patient's head is often tilted forward, with the chin almost touching the sternum (fixed flexion deformity).
- Significant pain and limited mobility in the neck, shoulders, and back of the head are common. Patients often support their head with their hands while walking or moving.
- On palpation of the spinous processes of the cervical spine, a "step-off" deformity may be felt: the spinous process of the underlying vertebra may protrude, while an impression or gap is felt above it where the overlying dislocated vertebra should be.
- The anteriorly displaced body of the overlying vertebra can sometimes make swallowing difficult (dysphagia) and may be palpable through the pharynx or visualized during laryngoscopy.
- Rotational Unilateral Dislocation of a Cervical Vertebra:
- The position of the patient's neck and head can vary depending on the degree of dislocation.
- In incomplete dislocation, the neck may be extended, with the head tilted and turned towards the healthy (non-dislocated) side.
- In complete dislocation, the head is often tilted towards the chest (flexed) and also dislocated and rotated towards the healthy side.
- The spinous processes of the upper vertebrae will be deflected towards the side of dislocation.
- Neurological Symptoms (Common with Cervical Dislocations):
- Changes in sensation of a radicular nature (affecting specific nerve roots): hypesthesia (reduced sensation), paresthesia (tingling/pins and needles), or analgesia (loss of pain sensation).
- Paresis (weakness) or paralysis of the muscles of the upper extremities (mono- or paraparesis, paraplegia) as a result of compression or damage to cervical nerve roots.
- Paralysis of all four limbs (quadriplegia or tetraplegia) indicates damage to the substance of the spinal cord itself. The severity of these neurological symptoms is critical for prognosis. A fatal outcome due to respiratory paralysis (from high cervical cord injury) is not uncommon with severe dislocations.
Computed tomography (CT) of the cervical spine demonstrates anterior displacement (anterolisthesis) of the C5 vertebral body relative to C6 following an injury (displacement indicated by an arrow). The image also shows a widened retropharyngeal space (6mm), suggesting prevertebral soft tissue swelling.
This CT scan of the cervical spine reveals a complex injury involving a fracture with associated dislocation of the C7 vertebra, demonstrating the "locking" or engagement of the facet joints, which prevents spontaneous reduction.
Radiological Evaluation
Imaging is essential to confirm the diagnosis, determine the type and severity of dislocation, identify associated fractures, and assess for spinal cord or nerve root compression.
- Plain X-rays: Standard views (anteroposterior, lateral, and odontoid view for upper cervical spine) are often the initial imaging. They can show vertebral misalignment, facet joint displacement, and associated fractures. Lateral views are particularly important for assessing anteroposterior displacement. However, as noted, in lateral cervical spine X-rays, the lower cervical vertebrae can be obscured by the shoulders, necessitating special views (e.g., swimmer's view) or alternative imaging.
- Computed Tomography (CT) Scan: CT provides excellent detail of bony injuries, including subtle fractures, facet joint relationships, and the degree of spinal canal compromise. It is often the imaging modality of choice after initial X-rays, especially if a fracture-dislocation is suspected or if X-rays are inconclusive. 3D reconstructions can be very helpful.
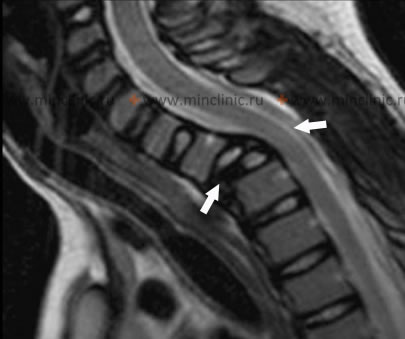
- Magnetic Resonance Imaging (MRI): MRI is crucial for evaluating soft tissue injuries, including ligamentous damage (which is always present in significant dislocations), intervertebral disc herniations, spinal cord compression or injury (edema, hemorrhage, transection), and epidural hematomas. It is particularly important if neurological deficits are present.
- Flexion-Extension X-rays (Dynamic Views): May be performed cautiously in stable patients with suspected ligamentous instability or subluxation, but are generally contraindicated in acute, unstable dislocations until stability is achieved.
This lateral MRI of the cervical spine demonstrates anterior displacement of the C7 vertebral body and a fracture of the Th1 vertebral body (indicated by arrows). These injuries have resulted in significant compression of the spinal cord at this level following trauma.
Treatment of Dislocation and Subluxation of the Vertebrae
The management of vertebral dislocations and subluxations is a complex task, often requiring emergency intervention, and aims to reduce the dislocation (restore normal alignment), stabilize the spine, decompress neural elements if compromised, and facilitate neurological recovery.
Principles of Reduction
Reduction (realignment) of a dislocated vertebra can be challenging, even under anesthesia, due to muscle spasm and locked facets.
- Incomplete Unilateral Cervical Dislocations: These are generally easier to reduce. Techniques may involve cervical traction (e.g., using a Glisson loop or skeletal traction with Gardner-Wells tongs) along the length of the body, combined with careful manipulation such as turning the head in the opposite direction of the rotation.
- Complete Bilateral "Locked" Cervical Dislocations: These are more difficult. Reduction requires disengaging the "locked" or "jumped" facets. This often involves initial traction, followed by controlled flexion of the head towards the side of dislocation to unlock the facets, then rotation towards the healthy side, all while maintaining constant axial traction. After disengagement and while continuing traction, a reverse maneuver (abducting the head to the healthy side, followed by rotation towards the dislocation side) may be performed to achieve final alignment. It has also been recommended to convert a flexion dislocation of a cervical vertebra into a rotational, unilateral one, and then reposition it.
All reduction maneuvers, especially closed ones, must be performed by experienced physicians with extreme caution, often with neurophysiological monitoring and imaging guidance, to avoid worsening neurological injury.
The Gardner-Wells tongs or brace is a form of skeletal traction used in emergency care for cervical spine injuries, including dislocations. It allows for controlled axial traction along the length of the neck, often applied using an adjustable weight and pulley system attached to an X-ray transparent table to facilitate imaging during reduction.
Conservative Treatment (Immobilization)
Following successful closed reduction of certain stable dislocations or subluxations, or for injuries deemed stable without significant neurological compromise, conservative treatment with temporary immobilization of the neck may be an option. This is typically for a period of 6 to 12 weeks to allow damaged ligaments, tendons, and muscles of the neck to heal. Compliance with immobilization is crucial, especially for ligamentous healing, as metabolic processes in ligaments are much slower than in muscles (which have a richer vascular network). Immobilization methods include:
- Cervical Orthoses (Braces): Such as a rigid cervical corset (e.g., Philadelphia collar, Miami J collar) for subaxial (C3-C7) injuries.
- Halo Vest Immobilization: Provides more rigid immobilization for unstable cervical spine injuries, including some upper cervical (C1-C2) injuries or highly unstable subaxial injuries.
Wearing a rigid neck brace, such as a Philadelphia collar, is a common method for immobilizing the cervical spine during the treatment of sprained ligaments and injured neck joints, including after reduction of dislocations or subluxations.
Immobilization with a neck brace, like the Philadelphia collar shown, is an important component in the conservative treatment of dislocation or subluxation of the articular processes (facet joints) of the cervical vertebrae, promoting healing and stability.
Surgical Treatment Options and Techniques
Most significant vertebral dislocations, especially those with neurological compromise, instability, or irreducible "locked" facets, require surgical stabilization. Surgical treatment for dislocation of the articular processes of the cervical vertebrae may be performed in one or two stages, depending on the clinical status and type of injury:
The sequence of these steps depends only on the clinical status of the patient and the type of damage present.
The treatment approaches can be broadly categorized:
| Technique | Description of Dislocation Reduction and Stabilization |
|---|---|
| Option 1: Closed Reduction followed by Surgical Stabilization | Applicable for unilateral or bilateral dislocation of cervical facet joints with neurological symptoms in conscious, cooperative patients.
|
| Option 2: Immediate MRI followed by Open Reduction and Surgical Stabilization | Applicable for patients with impaired consciousness, uncooperative behavior, or when closed reduction fails or is contraindicated.
|
| Anterior Open Reduction and Fixation with Discectomy (ACDF) | Indicated for:
|
| Posterior Reduction and Transpedicular or Lateral Mass Stabilization | Indicated for:
|
| Combined Anterior Decompression and Posterior Reduction/Stabilization (360° Fusion) | Indicated for severe injuries with anterior disc herniation requiring decompression in patients with a dislocation that was not reducible by closed or solely anterior open methods.
Features of one technique:
|
After reduction, a stabilizing operation is often performed to fix the vertebrae (e.g., discectomy with anterior and/or posterior fusion). Various fixation devices are used, including plates, implants (cages), and transpedicular or lateral mass screws and rods.
Most often, cervical spine dislocations occur at the C3-C5 or C5-C6 vertebral levels, i.e., in the mid-cervical spine where overall anterior mobility is greatest.
An example of posterior occipitocervical fusion surgery, involving fixation of the upper cervical vertebrae (axial vertebrae C1-C2) to the occipital bone, performed for severe injuries or instability at the cervico-occipital junction or upper cervical spine.
Anterior cervical discectomy and fusion (ACDF) is a common surgical procedure for stabilizing injuries or degenerative conditions of the subaxial cervical spine, such as at the C4-C5-C6 levels. It involves removing the damaged disc(s) and fusing the vertebrae with a bone graft and often a plate.
Differential Diagnosis of Acute Neck/Back Pain with Potential Instability
When a patient presents with acute spinal pain after trauma, a vertebral dislocation/subluxation needs to be differentiated from other injuries:
| Condition | Key Differentiating Features |
|---|---|
| Vertebral Dislocation/Subluxation | Obvious vertebral misalignment on imaging (X-ray, CT). Often severe pain, fixed deformity (especially cervical), potential neurological deficits. Significant ligamentous injury. |
| Vertebral Fracture (without significant dislocation) | Localized pain, tenderness, possible deformity. Fracture line visible on imaging. Neurological deficits depend on fracture stability and canal compromise. |
| Acute Intervertebral Disc Herniation | Often sudden onset of radicular pain, numbness, weakness. Positive nerve tension signs. MRI confirms disc herniation. May occur with or without major trauma. |
| Severe Ligamentous Sprain/Strain (Whiplash) | Neck pain, stiffness, muscle spasm after trauma. No bony injury or dislocation on imaging, but MRI may show ligamentous edema/tear. Diagnosis of exclusion for more severe injuries. |
| Muscle Spasm/Contusion | Localized muscle pain and tenderness. No bony or significant ligamentous injury. |
Potential Complications
Vertebral dislocations and subluxations can lead to severe and permanent complications:
- Spinal Cord Injury (SCI): Leading to paralysis (quadriplegia, paraplegia), sensory loss, and autonomic dysfunction (bowel, bladder, sexual dysfunction). This is the most devastating complication.
- Nerve Root Injury (Radiculopathy): Causing pain, weakness, and sensory loss in the distribution of the affected nerve root(s).
- Chronic Pain: Persistent neck or back pain.
- Spinal Instability: Leading to recurrent subluxations, progressive deformity, or delayed neurological injury.
- Post-Traumatic Deformity (Kyphosis, Scoliosis).
- Vascular Injury: E.g., vertebral artery injury with cervical dislocations, potentially leading to stroke.
- Nonunion or Malunion: If associated fractures do not heal properly.
- Complications of Treatment: Including those related to surgery (infection, hardware failure, pseudarthrosis) or prolonged immobilization (pressure sores, DVT).
Prevention and Prognosis
Prevention involves measures to avoid high-impact trauma:
- Using seatbelts and appropriate car seats.
- Following safety guidelines in sports (e.g., proper tackling techniques, avoiding diving into shallow water).
- Fall prevention measures, especially for the elderly.
- Workplace safety.
The prognosis after a vertebral dislocation depends heavily on the severity of the initial injury, particularly the presence and extent of neurological damage. Patients with complete spinal cord injuries have a poor prognosis for neurological recovery below the level of injury. Those with incomplete injuries or nerve root damage without cord injury may have a better potential for recovery with timely and appropriate treatment. Early reduction and stabilization are crucial for optimizing outcomes.
When to Seek Urgent Medical Care
Any significant trauma to the neck or back, especially if associated with the following, requires immediate emergency medical evaluation:
- Severe neck or back pain.
- Inability to move limbs, or new onset of weakness or paralysis.
- Numbness, tingling, or loss of sensation in any part of the body.
- Loss of bowel or bladder control.
- Visible deformity of the spine or abnormal head/neck position.
- Difficulty breathing after trauma.
Vertebral dislocations are serious injuries that require prompt assessment and management by specialists in spinal trauma (orthopedic spine surgeons or neurosurgeons).
References
- Vaccaro AR, Baron EM. Spine and Spinal Cord Trauma: Evidence-Based Management. Thieme; 2017.
- Fehlings MG, Cadotte DW, Fehlings LN. A series of systematic reviews on the diagnosis and treatment of acute spinal cord injury: a foundation for a North American Clinical Practice Guideline. J Neurosurg Spine. 2011 Mar;14(3):289-90.
- Allen BL Jr, Ferguson RL, Lehmann TR, O'Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982 Mar-Apr;7(2):121-30.
- Hadley MN, Walters BC, Aarabi B, et al. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery. 2013 Mar;60 Suppl 1:82-91.
- Marcon RM, Cristante AF, Teixeira WJ, et al. Fractures of the cervical spine. Clinics (Sao Paulo). 2013;68(11):1455-61.
- Dvorak MF, Fisher CG, Fehlings MG, et al. The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976). 2007 Oct 15;32(22):2421-9.
- Anderson PA, Montesano PX. Morphology and treatment of occipital condyle fractures. Spine (Phila Pa 1976). 1988 Jul;13(7):731-6. (Context for upper cervical injuries)
- White AA, Panjabi MM. Clinical Biomechanics of the Spine. 2nd ed. Lippincott Williams & Wilkins; 1990. (Classic text on spinal biomechanics and stability)
See also
- Anatomy of the spine
- Ankylosing spondylitis (Bechterew's disease)
- Back pain by the region of the spine:
- Back pain during pregnancy
- Coccygodynia (tailbone pain)
- Compression fracture of the spine
- Dislocation and subluxation of the vertebrae
- Herniated and bulging intervertebral disc
- Lumbago (low back pain) and sciatica
- Osteoarthritis of the sacroiliac joint
- Osteocondritis of the spine
- Osteoporosis of the spine
- Guidelines for Caregiving for Individuals with Paraplegia and Tetraplegia
- Sacrodinia (pain in the sacrum)
- Sacroiliitis (inflammation of the sacroiliac joint)
- Scheuermann-Mau disease (juvenile osteochondrosis)
- Scoliosis, poor posture
- Spinal bacterial (purulent) epiduritis
- Spinal cord diseases:
- Spinal spondylosis
- Spinal stenosis
- Spine abnormalities
- Spondylitis (osteomyelitic, tuberculous)
- Spondyloarthrosis (facet joint osteoarthritis)
- Spondylolisthesis (displacement and instability of the spine)
- Symptom of pain in the neck, head, and arm
- Pain in the thoracic spine, intercostal neuralgia
- Vertebral hemangiomas (spinal angiomas)
- Whiplash neck injury, cervico-cranial syndrome