Sacroiliitis (inflammation of the sacroiliac joint)
Anatomy of the Sacrum and Sacroiliac Joint
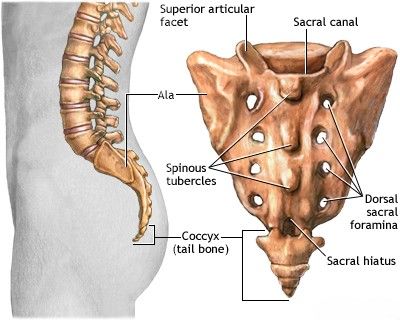
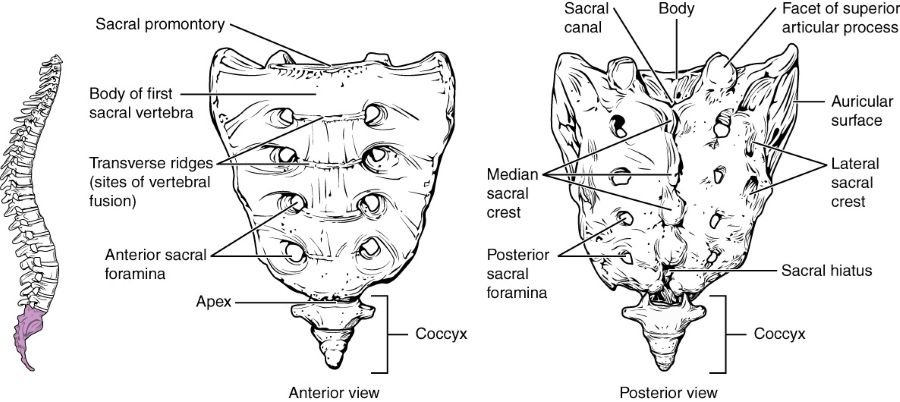
The sacrum is a large, triangular composite bone located at the base of the spine, forming the posterior part of the pelvis. It articulates superiorly with the fifth lumbar vertebra and inferiorly with the coccyx (tailbone).
Development and Characteristics of the Sacrum
In adults, the sacrum is formed by the fusion of five sacral vertebrae (S1-S5). This fusion process, however, is not complete at birth; the sacral vertebrae are initially separate. The fusion begins relatively late in development, typically after the age of 15 years, starting with the three lower vertebrae (S3-S5). By the age of 25, the two upper sacral vertebrae (S1-S2) also fuse with each other and with the lower segments to form a single, solid sacral bone. Anatomically, the sacrum in males tends to be longer, narrower, and more significantly curved than in females, a difference attributed to adaptations for childbirth in the female pelvis.
Incomplete fusion of the sacral vertebrae or associated congenital developmental anomalies can lead to conditions such as spina bifida occulta (a defect in the vertebral arch without protrusion of spinal contents), transitional vertebrae like sacralization of the L5 vertebra (fusion of the last lumbar vertebra to the sacrum) or lumbarization of the S1 vertebra (separation of the first sacral vertebra, giving it characteristics of a lumbar vertebra). More severe forms of spina bifida, such as meningocele or meningomyelocele, involve protrusion of the spinal membranes or neural tissue through the vertebral arch defect.
This image displays the anatomical structure of the sacrum bone and the auricular (ear-shaped) articular surfaces that form the sacroiliac joint with the iliac bones of the pelvis.
The Sacroiliac Joint (SIJ)
The lateral surfaces of the sacrum possess prominent, irregular auricular (ear-shaped) articular surfaces. These articulate with corresponding auricular surfaces on the iliac bones of the pelvis on each side, forming the bilateral sacroiliac (SI) joints. The SI joint is a complex joint that is partly synovial (allowing limited movement) and partly syndesmotic (fibrous, allowing very little movement). It is characterized by its inherent stability, reinforced by a dense network of strong intrinsic and extrinsic ligaments (e.g., anterior and posterior sacroiliac ligaments, interosseous sacroiliac ligament, sacrotuberous, and sacrospinous ligaments). Due to its robust ligamentous support and irregular, interlocking articular surfaces, the SI joint is a very rigid formation, designed primarily for weight transmission and stability rather than extensive motion. It is often referred to as the sacroiliac junction to emphasize its limited mobility.
Understanding Sacroiliitis and its Causes
Definition of Sacroiliitis
Sacroiliitis is defined as inflammation of one or both sacroiliac joints (SIJs), which are the junctions between the sacrum (the triangular bone at the base of the spine) and the iliac bones of the pelvis. This inflammation can cause pain in the lower back, buttocks, and sometimes radiating down the legs.
Etiological Factors
The causes of sacroiliac joint inflammation leading to sacroiliitis are diverse and can include:
- Mechanical Stress or Overload: Prolonged positional overload of the lower limb girdle and lumbopelvic region can contribute to SIJ pain and inflammation. This can occur due to:
- Sedentary work with prolonged sitting.
- Repetitive heavy lifting or carrying heavy objects.
- Pregnancy (due to hormonal ligamentous laxity, weight gain, and altered biomechanics).
- Leg length discrepancy or gait abnormalities.
- Trauma: Direct trauma to the pelvis or sacrum, such as from a fall, motor vehicle accident, or sports injury, can lead to acute sacroiliitis or chronic SIJ dysfunction.
- Infection (Infectious Sacroiliitis): Bacterial infection of the SIJ (pyogenic sacroiliitis) is uncommon but can occur, often via hematogenous spread from another site of infection or direct inoculation. *Staphylococcus aureus* is a common pathogen. Tuberculosis can also affect the SIJ.
- Autoimmune Processes (Inflammatory Spondyloarthropathies): Sacroiliitis is a hallmark feature of several inflammatory rheumatic diseases, collectively known as spondyloarthropathies. These include:
- Ankylosing Spondylitis (AS): Bilateral sacroiliitis is a defining characteristic.
- Psoriatic Arthritis.
- Reactive Arthritis (formerly Reiter's syndrome).
- Enteropathic Arthritis (associated with inflammatory bowel disease like Crohn's disease or ulcerative colitis).
- Undifferentiated Spondyloarthritis.
- Degenerative Changes (Osteoarthritis of the Sacroiliac Joint): Wear and tear of the SIJ cartilage can lead to osteoarthritis and associated pain and inflammation, particularly in older individuals or those with previous trauma.
- Crystal Arthropathies: Gout or pseudogout can rarely affect the SIJ.
Common Symptoms
The primary complaint of a patient with sacroiliitis is pain localized to the sacral region (sacrodynia), often felt unilaterally or bilaterally over the affected sacroiliac joint(s) or buttocks. The characteristics of the pain can vary:
- Nature of Pain: It may be described as aching, dull, sharp, or similar to a "bruise."
- Intensity: Can range from mild discomfort to severe, debilitating pain.
- Triggers/Aggravating Factors: Pain is often worsened by activities that stress the SIJ, such as:
- Prolonged standing or walking.
- Prolonged sitting, especially on hard surfaces.
- Climbing stairs.
- Rising from a seated position.
- Lying on the affected side.
- Certain movements like twisting, bending, or impact activities.
- Radiation of Pain: Pain may radiate to the buttock, lower back, groin, posterior thigh, and occasionally down the leg (pseudo-sciatica), but typically does not extend below the knee in a true dermatomal pattern.
- Stiffness: Morning stiffness or stiffness after periods of inactivity, particularly if inflammatory in origin (e.g., spondyloarthritis).
- Heaviness or Discomfort: A feeling of constant heaviness or discomfort in the lumbopelvic region, especially after exertion such as walking, sitting for long periods, or activities like dancing.
Diagnosis and Symptoms of Sacroiliitis
The diagnosis of sacroiliitis involves a comprehensive evaluation that includes a detailed patient history, a thorough physical examination focusing on lumbopelvic biomechanics, and often confirmatory imaging and laboratory studies.
Clinical Examination
- Patient History (Anamnesis): The physician will inquire about the onset, duration, location, character, radiation, intensity, and aggravating/relieving factors of the pain. A history of trauma, recent infections, systemic inflammatory diseases, pregnancy, or occupational/lifestyle factors is important.
- Physical Examination:
- Inspection: Observation of gait, posture, and any visible asymmetry or swelling in the lumbopelvic region.
- Palpation: Tenderness is often elicited by direct palpation over the sacroiliac joints (located just medial to the posterior superior iliac spines - PSIS). This can dramatically increase the patient's reported pain (sacrodynia) if sacroiliitis is present. Tenderness in surrounding muscles (gluteal, piriformis) may also be noted.
- Range of Motion: Assessment of lumbar spine and hip joint mobility.
- Provocative Tests for SIJ Pain: Several specific clinical maneuvers are used to stress the SIJ and reproduce the patient's pain. Common tests include:
- FABER (Patrick's) Test: Flexion, Abduction, External Rotation of the hip.
- Gaenslen's Test.
- Thigh Thrust Test (Posterior Pelvic Pain Provocation Test).
- Sacral Thrust Test.
- Compression Test and Distraction Test.
- Neurological Examination: To rule out lumbar radiculopathy or other neurological causes of pain.
Gynecological diseases affecting the pelvic organs in women can cause referred pain symptoms (sacrodynia) that are perceived in the sacrum, sometimes imitating the pain of sacroiliitis. (Image illustrative of pelvic anatomy).
Laboratory and Imaging Studies
- Laboratory Tests:
- Blood tests may reveal signs of inflammation, such as an increase in the erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP), particularly in inflammatory or infectious sacroiliitis.
- HLA-B27 testing may be performed if a spondyloarthropathy like ankylosing spondylitis is suspected.
- Other tests may be done to rule out infection or other systemic diseases based on clinical suspicion.
- Imaging Studies:
- X-ray of the Pelvic Bones and Sacroiliac Joints: Can show signs of sacroiliitis such as erosions, sclerosis (increased bone density), joint space narrowing, or ankylosis (fusion) in chronic inflammatory conditions. It also helps to exclude traumatic causes of SIJ damage or significant osteomyelitis.
- Computed Tomography (CT) Scan: CT has made a great contribution to the modern diagnosis of diseases affecting the pelvic bones and their joints in sacroiliitis. CT of the sacral spine and pelvic bones provides more detailed bony anatomy than X-rays and can better delineate arthrosis of the sacroiliac joint, subtle erosions, or fractures. CT also helps to exclude oncological causes of lesions affecting the pelvic bones or vertebral bodies in patients presenting with sacral pain.
- Magnetic Resonance Imaging (MRI): MRI is the most sensitive imaging modality for detecting early inflammation in and around the SIJs (active sacroiliitis), such as bone marrow edema, synovitis, and enthesitis, even before structural changes are visible on X-rays or CT. It is particularly useful in diagnosing early spondyloarthropathies. MRI can also evaluate surrounding soft tissues and rule out other pathologies.
- Bone Scan (Scintigraphy): Can show increased uptake in areas of inflammation or increased bone turnover in the SIJs but is non-specific.
- Diagnostic SIJ Injection: Injection of local anesthetic into the SIJ under imaging guidance (fluoroscopy or ultrasound) can be both diagnostic and therapeutic. Significant pain relief after the injection strongly suggests the SIJ as the source of pain.
Computed tomography (CT) of the pelvic bones, including the sacrum and ilium, allows for detailed assessment and can help exclude oncological lesions of the sacrum or adjacent vertebrae in a patient presenting with symptoms suggestive of sacroiliitis.
Treatment of Sacroiliitis
The treatment of sacroiliitis is aimed at reducing inflammation, relieving pain, improving function, and addressing the underlying cause if identified.
Conservative Management
- Activity Modification: Avoiding activities that exacerbate pain (e.g., prolonged sitting/standing, high-impact activities). If possible, complete or partial limitation of excessive physical exertion on the sacroiliac joint is recommended.
- Supportive Measures for Pregnant Women: For unloading the lumbosacral region in pregnant women with sacroiliac pain, a special maternity support belt or pelvic brace can be used.
- Physical Therapy (Physiotherapy): A cornerstone of treatment. Includes:
- Exercises to improve flexibility, strength, and stability of the lumbopelvic region (core muscles, gluteal muscles, hip abductors).
- Stretching exercises for tight muscles (e.g., hamstrings, hip flexors, piriformis).
- Manual therapy techniques (mobilization or manipulation of the SIJ and lumbar spine by a qualified therapist).
- Postural education and correction of biomechanical faults.
- Modalities like heat, cold, TENS, or ultrasound for symptomatic relief.
In the treatment of sacroiliitis, physiotherapy plays a vital role. It helps to eliminate inflammation and pain symptoms (sacrodynia), and restore range of motion in the sacrum and surrounding muscles of the lower back and buttocks, thereby accelerating recovery.
Pharmacological Therapy
Medical treatment for sacroiliitis is prescribed depending on the severity of the specific symptoms in a patient and the underlying cause:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): First-line medications for reducing pain and inflammation (e.g., ibuprofen, naproxen, diclofenac, celecoxib). Can be used topically (gels/creams) or orally.
- Analgesics: Acetaminophen for pain relief if NSAIDs are contraindicated or insufficient. Stronger analgesics (e.g., opioids) are reserved for severe acute pain and used for short durations.
- Muscle Relaxants: May be prescribed for associated muscle spasms.
- Disease-Modifying Antirheumatic Drugs (DMARDs): If sacroiliitis is part of an inflammatory spondyloarthropathy (e.g., ankylosing spondylitis), DMARDs such as sulfasalazine, methotrexate, or biologic agents (e.g., TNF inhibitors, IL-17 inhibitors) are used to control the underlying systemic inflammation under the guidance of a rheumatologist.
- Antibiotics: For infectious sacroiliitis, appropriate intravenous and/or oral antibiotics are essential, guided by culture results.
- Glucocorticoids (Systemic): Oral corticosteroids are generally not used for mechanical SIJ pain but may be considered for short periods in severe inflammatory sacroiliitis or acute flares of spondyloarthropathy.
Interventional Pain Management (Injections)
If pain (sacrodynia) is severe in a patient with sacroiliitis and unresponsive to conservative measures, therapeutic injections (blockades) into or around the SIJ can be performed under imaging guidance (fluoroscopy or ultrasound):
- Sacroiliac Joint Injections: Injection of a local anesthetic and a corticosteroid (e.g., lidocaine with hydrocortisone, diprospan/betamethasone, Kenalog/triamcinolone) directly into the SIJ. This can provide significant pain relief and reduce inflammation.
- Periarticular Injections: Injections into ligaments or trigger points around the SIJ.
- Radiofrequency Ablation (RFA) / Neurotomy: For chronic SIJ pain, RFA can be used to denervate the sensory nerves supplying the joint, providing longer-lasting pain relief.
Physical and Manual Therapies
In addition to prescribed exercises, other therapies include:
- Manual Therapy: Techniques performed by qualified physical therapists, chiropractors, or osteopaths, such as SIJ mobilization or manipulation, muscle energy techniques, and soft tissue mobilization.
- Physiotherapy Modalities: In addition to exercise, modalities like heat, cold, TENS, ultrasound, or UHF therapy may be used on the affected side of the sacroiliac joint.
- Acupuncture: May help alleviate pain in some individuals.
Supportive Measures (Bracing)
Wearing a semi-rigid lumbosacral brace or, more specifically, a sacroiliac belt or brace can help to limit painful motion in the sacroiliac joint. This support can reduce the symptoms of pain in the area of SIJ inflammation in sacroiliitis and relieve excessive protective tension and spasm of the muscles of the lower back and buttock area. With such a brace, the patient can often move more independently at home and outdoors, and manage sitting in a car or at their workplace. The need for a corset or SI belt typically diminishes as the pain in the sacrum passes. Various types of lumbosacral semi-rigid braces and SI belts are available; they are selected according to size and can be used repeatedly in case of recurrent pain in the sacrum region.
Wearing a sacroiliac brace helps in the treatment of sacroiliac pain (sacrodynia) and arthrosis of the sacroiliac joint by providing compression and stability to the articulation.
A variant of a semi-rigid lumbosacral brace, which can provide support and help in the treatment of pain localized to the sacrum (sacrodynia).
Surgical Treatment (Rare)
Surgical treatment for sacroiliitis (e.g., SI joint fusion) is rarely necessary and is reserved for cases of severe, debilitating chronic pain that has not responded to comprehensive conservative and interventional management, and where the SIJ is definitively identified as the primary pain generator.
Differential Diagnosis of Sacroiliac Region Pain
Pain in the SIJ region can be mimicked by or associated with several other conditions:
| Condition | Key Differentiating Features |
|---|---|
| Sacroiliitis | Pain over SIJ, buttock, posterior thigh; positive SIJ provocative tests; imaging (X-ray, MRI, CT) shows inflammation/degeneration of SIJ. |
| Lumbar Disc Herniation with Radiculopathy (e.g., L5/S1) | Radiating leg pain (sciatica) in dermatomal pattern, numbness, weakness, altered reflexes. Positive SLR. MRI shows disc herniation impinging on nerve root. |
| Lumbar Facet Joint Syndrome | Low back pain, may refer to buttock/thigh (rarely below knee). Worse with extension/twisting. Tenderness over lumbar facets. |
| Piriformis Syndrome / Gluteal Myofascial Pain | Buttock pain, may mimic sciatica. Tenderness over piriformis or gluteal trigger points. Pain with specific muscle stretch/contraction. |
| Hip Joint Pathology (e.g., Osteoarthritis, Bursitis) | Groin pain, lateral hip pain, pain with hip movements (e.g., internal/external rotation). Can refer to buttock/thigh. |
| Pelvic Organ Disease (Gynecological, Urological) | Pain often deep, aching, may be cyclical. Associated symptoms related to the involved organ system. |
| Sacral Stress Fracture or Tumor | Localized sacral pain, may have history of trauma or risk factors (osteoporosis, cancer). Imaging (MRI, CT, bone scan) diagnostic. |
Complications and Prevention
Untreated or chronic sacroiliitis can lead to:
- Chronic pain and disability.
- Difficulty with daily activities like walking, sitting, and standing.
- Altered gait and posture.
- Reduced quality of life.
- In inflammatory spondyloarthropathies, progressive ankylosis (fusion) of the SIJs and spine can occur if the underlying disease is not controlled.
Prevention strategies may include:
- Maintaining good posture and body mechanics.
- Regular exercise to strengthen core and pelvic stabilizing muscles.
- Avoiding prolonged static positions or repetitive stress on the SIJs.
- Early diagnosis and management of underlying inflammatory conditions.
When to Consult a Specialist
Consultation with a physician (e.g., general practitioner, rheumatologist, orthopedic specialist, physiatrist, or pain management specialist) is recommended if:
- Pain in the lower back, buttock, or sacral region is persistent, severe, or worsening.
- Pain is associated with morning stiffness that improves with activity (suggestive of inflammatory cause).
- There are symptoms of systemic illness (fever, weight loss) or "red flag" signs.
- Pain significantly impacts daily functioning or sleep.
- Conservative self-care measures fail to provide relief.
- There is a family history of spondyloarthritis or other inflammatory rheumatic diseases.
An accurate diagnosis is key to developing an effective treatment plan for sacroiliitis and related sacral pain.
References
- Cohen SP, Chen Y, Neff N. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2013 Mar;116(3):695-710.
- Forst SL, Wheeler MT, Fortin JD, Vilensky JA. The sacroiliac joint: anatomy, physiology and clinical significance. Pain Physician. 2006 Jan;9(1):61-7.
- Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012 Dec;221(6):537-67.
- Sieper J, Rudwaleit M, Baraliakos X, et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis. 2009 Jun;68 Suppl 2:ii1-44. (Context for inflammatory sacroiliitis)
- van der Heijde D, Ramiro S, Landewé R, et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis. 2017 Jun;76(6):978-991.
- Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976). 1995 Jan 1;20(1):31-7.
- Hansen HC, McKenzie-Brown AM, Cohen SP, et al. Sacroiliac joint interventions: a systematic review. Pain Physician. 2007 Jan;10(1):165-84.
- Sembrano JN, Polly DW Jr. Sacroiliac joint dysfunction. Mayo Clin Proc. 2009 Jan;84(1):93-4.
See also
- Anatomy of the spine
- Ankylosing spondylitis (Bechterew's disease)
- Back pain by the region of the spine:
- Back pain during pregnancy
- Coccygodynia (tailbone pain)
- Compression fracture of the spine
- Dislocation and subluxation of the vertebrae
- Herniated and bulging intervertebral disc
- Lumbago (low back pain) and sciatica
- Osteoarthritis of the sacroiliac joint
- Osteocondritis of the spine
- Osteoporosis of the spine
- Guidelines for Caregiving for Individuals with Paraplegia and Tetraplegia
- Sacrodinia (pain in the sacrum)
- Sacroiliitis (inflammation of the sacroiliac joint)
- Scheuermann-Mau disease (juvenile osteochondrosis)
- Scoliosis, poor posture
- Spinal bacterial (purulent) epiduritis
- Spinal cord diseases:
- Spinal spondylosis
- Spinal stenosis
- Spine abnormalities
- Spondylitis (osteomyelitic, tuberculous)
- Spondyloarthrosis (facet joint osteoarthritis)
- Spondylolisthesis (displacement and instability of the spine)
- Symptom of pain in the neck, head, and arm
- Pain in the thoracic spine, intercostal neuralgia
- Vertebral hemangiomas (spinal angiomas)
- Whiplash neck injury, cervico-cranial syndrome