Compression of the spinal cord
- Understanding Spinal Cord Compression and Related Myelopathies
- Extradural Spinal Cord Tumors (Primarily Metastatic)
- Intradural Extramedullary Spinal Cord Tumors
- Epidural Abscess of the Spinal Cord
- Spinal Epidural Hemorrhage and Hematomyelia
- Acute Herniated (Extruded) Disc Causing Cord Compression
- Other Atypical Compressive Lesions of the Spinal Cord
- Differential Diagnosis of Spinal Cord Compression Syndromes
- General Principles of Management and Prognosis
- When to Seek Urgent Medical Attention
- References
Understanding Spinal Cord Compression and Related Myelopathies
Spinal cord compression occurs when any pathological process narrows the spinal canal and impinges upon the spinal cord or its nerve roots, leading to neurological dysfunction (myelopathy or radiculopathy). Tumors within the spinal canal are a significant cause of such compression and are broadly classified based on their origin and relationship to the dura mater (the outermost covering of the spinal cord).
Classification of Spinal Canal Tumors
Spinal canal tumors are divided into:
- Primary Tumors: Originating from tissues within or surrounding the spinal cord (e.g., meninges, nerve roots, glial cells, blood vessels, bone).
- Secondary (Metastatic) Tumors: Cancer cells that have spread (metastasized) to the spine or epidural space from a primary cancer elsewhere in the body.
Based on their location relative to the dura mater and spinal cord parenchyma, these tumors can be further classified:
- Extradural (or Epidural) Tumors: Located outside the dura mater, in the epidural space. These are the most common type of spinal tumors, with metastases being a frequent cause.
- Intradural Tumors: Located beneath (within) the dura mater. These are further subdivided into:
- Extramedullary Tumors: Located within the dura but outside the spinal cord parenchyma itself (e.g., arising from nerve roots like schwannomas/neurofibromas, or from the meninges like meningiomas).
- Intramedullary Tumors: Located within the substance (parenchyma) of the spinal cord (e.g., astrocytomas, ependymomas, intramedullary metastases).
While myelopathies in cancer patients most often result from compressive lesions, if imaging studies like MRI or CT myelography do not detect a cerebrospinal fluid (CSF) block or obvious external compression, it can be challenging to differentiate between intramedullary metastases, paraneoplastic myelopathy, and radiation myelopathy based solely on these initial findings without contrast or specialized sequences.
Extradural Spinal Cord Tumors (Primarily Metastatic)
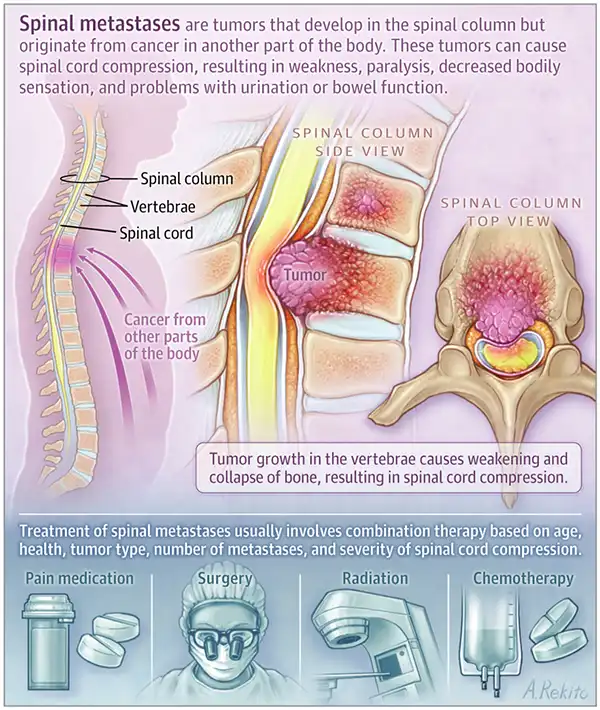
In clinical practice, neurologists and neurosurgeons most frequently encounter extradural spinal cord tumors. The vast majority of these are metastases from primary cancers located elsewhere in the body, often organs near the spine or those with a propensity for bony spread. Common primary sites for spinal metastases include the prostate, breast, and lungs. Lymphomas and plasma cell dyscrasias (like multiple myeloma) also frequently involve the spine and epidural space. Indeed, the development of metastatic epidural spinal cord compression (MESCC) is a described complication in almost all forms of human malignant tumors.
Clinical Presentation and Symptoms
The first symptom of epidural (extradural) spinal cord compression due to a tumor is usually a patient's complaint of local back pain at the level of the lesion. This pain can be insidious or acute, often worsening in the supine (lying down) position and frequently forcing the patient to wake up at night. Back pain is often accompanied by radiating radicular pain (pain shooting along a nerve root distribution), which intensifies with activities that increase intraspinal pressure, such as coughing, sneezing, or straining. Frequently, back pain and localized tenderness on palpation may precede other neurological symptoms of epidural compression by many weeks.
Neurological symptoms in a patient with epidural spinal cord compression typically develop progressively over a few days or weeks. The first manifestation of the spinal cord compression syndrome is usually progressive weakness in the extremities (legs if thoracic/lumbar, arms and legs if cervical). This weakness can eventually progress to encompass all the signs of a transverse myelopathy, including paraparesis or tetraparesis (weakness of two or four limbs, respectively), and a distinct level of sensory loss.
Diagnostic Evaluation
Conventional radiography (X-rays) of the spine may reveal destruction or a compression fracture of a vertebral body at the level corresponding to the spinal cord injury syndrome. Bone scintigraphy (bone scan) is even more informative for detecting multiple bony metastases. However, MRI with contrast is the gold standard for diagnosing spinal cord compression. CT scans and myelography (with contrast injected into the subarachnoid space) can also be significant. These studies can show a horizontal symmetrical expansion and compression of the spinal cord by an extramedullary pathological formation, often noticeable by the boundaries of a blockade of the subarachnoid space (CSF block). With a complete CSF block, changes in the adjacent vertebrae (e.g., erosion, collapse) may also be evident.
Treatment Strategies
Therapeutic tactics for extramedullary compression of the spinal cord by a tumor can be conservative or operative, often involving a multidisciplinary approach.
- Corticosteroids: If spinal cord compression is suspected, high-dose corticosteroids (e.g., dexamethasone) are often administered immediately to reduce edema around the tumor and spinal cord, which can provide rapid but temporary neurological improvement.
- Radiation Therapy: For radiosensitive tumors (e.g., lymphoma, myeloma, some carcinomas), radiation therapy to the affected spinal segment is a primary treatment modality. It can effectively shrink the tumor and relieve compression.
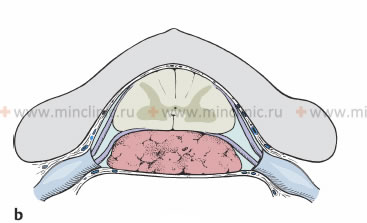
- Surgical Decompression: In a neurosurgical hospital, a patient with extramedullary compression of the spinal cord by a tumor may undergo surgical decompression, often via laminectomy. The essence of a laminectomy operation is to remove the posterior bony arch of the vertebra to create more space (a "bone window") in the area of spinal cord compression by tumor masses, allowing for tumor removal or debulking.
- Chemotherapy: Systemic chemotherapy targeted at the primary cancer type may be used, especially if the tumor is chemosensitive.
- Stabilization: If the tumor has caused significant bony destruction leading to spinal instability, surgical stabilization with instrumentation may be necessary.
The choice between conservative treatment (e.g., radiation and corticosteroids) and surgical intervention for MESCC depends on several factors. After the introduction of corticosteroids for one or two days, the severity of leg muscle weakness (paraparesis) in patients often decreases. For some incomplete or early syndromes of transverse spinal cord injury, neurosurgical treatment may be appropriate if there is a single site of compression, the tumor is relatively radioresistant, there is spinal instability, or the diagnosis is uncertain. In any case, individual analysis of treatment tactics is required, considering the radiosensitivity of the tumor, the localization of other metastases, and the general condition of the patient. Regardless of the chosen treatment tactic (surgical treatment, radiation therapy, or both), it should be applied to the patient quickly to maximize the chance of neurological recovery.
As a general principle, when cancer spreads to the spine and presses on the spinal cord, surgery can help restore nerve function. However, if the surgery is performed late (after significant neurological deficits have developed) or involves the thoracic part of the spine (where spinal cord blood supply can be more tenuous), the chances of nerve recovery are lower. Also, patients who have more severe nerve damage before surgery are less likely to regain ambulation after surgery. To improve nerve function, quality of life, and survival, it is crucial to detect and treat spinal cord compression early.
When cancer spreads to the spine and causes metastatic epidural spinal cord compression, surgery can help restore nerve function. However, if surgery is delayed or involves the thoracic spine, chances of nerve recovery are lower. Patients with more pre-operative nerve damage are less likely to walk again. Early detection (on MRI) and treatment are vital to improve nerve function, quality of life, and survival.
Intradural Extramedullary Spinal Cord Tumors
Intradural extramedullary spinal cord tumors are located within the dural sac but outside the substance of the spinal cord itself. They typically grow at a slower rate compared to extradural tumors (especially metastases) and are therefore less likely to cause acute spinal cord compression, though progressive compression is common.
Common Types and Clinical Features
Among intradural extramedullary spinal cord tumors, **meningiomas** (arising from the arachnoid cap cells of the meninges) and **neurofibromas/schwannomas** (arising from nerve roots) are the most common. Other tumor types, such as hemangiopericytoma or other tumors of the spinal coverings (shells), are rare in clinical practice.
At the beginning of spinal cord involvement by an intradural extramedullary tumor, patients often develop radicular sensory disturbances (pain, paresthesias in a dermatomal distribution) and an asymmetric pattern of neurological disorders. Computed tomography (CT) of the spinal cord and myelography (or MRI, which is now preferred) typically reveal a characteristic pattern of displacement (dislocation) of the spinal cord away from the tumor, which is located within the subarachnoid space.
Cerebrospinal Fluid (CSF) Findings
A slight increase in the protein content in the cerebrospinal fluid (CSF) is detected in patients with oncological compressive myelopathies of all types. In the case of a complete CSF block of the subarachnoid space of the spinal cord by a tumor, the protein concentration in the CSF collected below the block can increase significantly, sometimes to 1000-10000 mg/dL (10-100 g/L). This phenomenon (Froin's syndrome: high protein, xanthochromia, few cells) is due to the stagnation of CSF dynamics from the caudal sac upwards towards the cranial subarachnoid space, where its physiological reabsorption occurs.
In normal adult CSF, there are practically no or very few cellular elements (typically <5 white blood cells/mm³). The cell count in the CSF of patients with intradural extramedullary spinal cord tumors will usually be small or zero, unless there is associated inflammation or bleeding. Cytological examination of CSF typically does not reveal tumor cells for benign extramedullary tumors like meningiomas or schwannomas, unless it's a malignant primary (e.g., leptomeningeal spread of a CNS tumor) or metastatic tumor involving the leptomeninges. The glucose content in the patient's CSF may also be within the normal range if the tumor is not accompanied by widespread carcinomatous meningitis of the spinal cord membranes (which can cause low CSF glucose).
Epidural Abscess of the Spinal Cord
Etiology and Clinical Course
Treatment of a spinal epidural abscess in patients generally does not cause diagnostic difficulties if considered. It is important to diagnose an epidural abscess in a timely manner at the beginning of the disease, without confusing it with a non-infectious tumor lesion of the spinal cord. Several conditions predispose to the occurrence of a spinal epidural abscess:
- Furunculosis (boils) of the occipital region of the scalp or other skin infections.
- Bacteremia (bacteria in the bloodstream) or sepsis from any source.
- Minor back injuries or trauma.
- Intravenous drug use.
- Diabetes mellitus or other immunocompromising conditions.
A spinal epidural abscess can also develop as a complication after surgery on the structures of the spine (e.g., for herniated discs, vertebroplasty) or after procedures like lumbar puncture or epidural anesthesia. A common cause of an epidural abscess, which compresses the spinal cord as it increases in size, is vertebral osteomyelitis (infection of the vertebral bone). The focus of osteomyelitis may be small initially and not be detected on conventional radiographs. For an accurate diagnosis of osteomyelitis in a patient, it is necessary to conduct multi-spiral computed tomography (MSCT) of the spine or, preferably, MRI.
With an epidural abscess of the spinal cord, a patient typically experiences the following over several days or weeks:
- Elevated temperature (fever) of unclear nature.
- Mild to severe back pain, often localized and progressive.
- Local pain on palpation or percussion over the affected spinal level.
- Radicular pain (shooting pain along nerve roots) often appears later.
- Progressive neurological deficits as the abscess enlarges and compresses the spinal cord (weakness, sensory loss, bowel/bladder dysfunction).
Diagnosis and Treatment
Increasing in size, the epidural abscess compresses the spinal cord. This escalating extramedullary compression leads to a neurological syndrome of transverse spinal cord lesion, sometimes progressing to a complete functional break (complete paralysis and sensory loss). In the case of increasing clinical signs of spinal cord compression from an epidural abscess, urgent surgical decompression is necessary. This typically involves a laminectomy to expose the epidural space and drainage of the abscess cavity. In the postoperative period, a patient with an epidural abscess should be prescribed high-dose intravenous antibiotics, ideally selected based on the sensitivity of the bacterial culture obtained from the abscess. As with any infectious process, incomplete drainage of the abscess cavity often leads to the development of a chronic granulomatous and fibrous process (chronic epiduritis). The use of antibiotics alone in this scenario will not eliminate the compressive effect on the spinal cord if a significant collection or granulation tissue persists. Compressive "cold" abscesses (leaky abscesses) due to tuberculosis affecting the spine (Pott's disease) are currently rare in developed countries but remain a consideration.
Spinal Epidural Hemorrhage and Hematomyelia
In cases of hemorrhage affecting the spinal cord, either within its substance (hematomyelia) or in the surrounding spaces (subarachnoid hemorrhage, epidural hemorrhage), the patient may develop a clinical picture of acute transverse myelopathy within a few minutes or hours. Hemorrhages involving the spinal cord are typically accompanied by severe back pain.
Causes and Clinical Manifestations
The source of hemorrhage in **hematomyelia** (bleeding into the spinal cord) can be:
- Rupture of a spinal arteriovenous malformation (AVM, angioma, hemangioma).
- Hemorrhage within a spinal cord tumor.
- Complication of anticoagulant therapy (e.g., with warfarin for conditions like thrombosis of cerebral venous sinuses).
- Spontaneous hemorrhage (sometimes idiopathic or related to underlying, undiagnosed vascular anomalies or coagulopathies).
- Trauma.
Spinal epidural hemorrhages (hematomas) can develop as a result of:
- Minor or major spinal injuries.
- Complications of lumbar puncture or epidural anesthesia.
- Anticoagulant therapy with warfarin or other agents.
- Secondarily against the background of blood diseases (e.g., hemophilia, thrombocytopenia).
- Spontaneous rupture of an epidural vascular malformation (e.g., small epidural hemangioma).
Patients' complaints of back pain and radicular pain in spinal cord hemorrhages (whether hematomyelia or epidural hematoma) often precede the onset of weakness by several minutes or hours. Weakness and pain can be significantly pronounced, forcing patients to assume antalgic (pain-avoiding) positions when moving. An epidural hematoma at the level of the lumbar spinal cord segments is often accompanied by the loss of knee and Achilles reflexes, whereas retroperitoneal hematomas (which can also cause back pain and neurological symptoms) typically cause loss of knee reflexes only (due to femoral nerve involvement) without affecting Achilles reflexes unless there is lumbosacral plexus involvement.
This MRI of the thoracic spine shows an extradural hematoma that arose as a postoperative complication in a patient following an operation to remove a hemangioma.
Diagnostic Considerations
When diagnosing a spinal hemorrhage in a patient, a space-occupying (volumetric) process is often determined on myelography (historically). Computed tomography (CT) of the spine without contrast sometimes does not clearly detect an acute hematoma, because the dense blood clot cannot always be easily distinguished from adjacent bone tissue. MRI is far superior for detecting and characterizing hematomas.
Spinal cord hematomas can form as a result of spontaneous bleeding. Blood clots can be caused by the same factors as epidural hemorrhages and can produce a particularly pronounced pain syndrome if located in the subdural or subarachnoid spaces. In an epidural hemorrhage, the cerebrospinal fluid (CSF) obtained by lumbar puncture is usually clear or may contain a small number of red blood cells if there has been minor dural irritation or puncture. In contrast, with a spinal subarachnoid hemorrhage, the CSF is initially bloody, and later (after several hours) acquires a pronounced yellow-brown hue (xanthochromia) due to the presence of blood breakdown pigments. Additionally, with subarachnoid hemorrhage, pleocytosis (increased white blood cells) and a decrease in glucose concentration can be detected in the CSF due to meningeal irritation, which can sometimes create a false clinical picture similar to bacterial meningitis.
An intraspinal (intramedullary) hematoma can be caused by spontaneous rupture of an internal vascular malformation, such as telangiectasia in the gray matter. More often, it is the result of an injury. If bleeding begins in the central area of the cord, it usually spreads up and down along the axis of the spinal cord, involving several segments, and is referred to as hematomyelia. Clinically, an acute syndrome develops, which can very much resemble the chronic syndrome characteristic of syringomyelia (e.g., dissociated sensory loss, weakness).
Spinal epidural bleeding (hematoma) is relatively rare. It is usually caused not by direct trauma to epidural vessels, but by a rupture of a vascular malformation, most often a small-vascular hemangioma (AVM, angioma, or cavernoma) located in the epidural space or originating from nearby bones of the spine. Radiography may reveal vertical trabeculae in the spongy substance of a vertebral body, characteristic of a vertebral hemangioma, which can sometimes be the source of an epidural bleed. Blood is not always collected directly in the area of the angioma itself. A hematoma typically develops over the dorsal (posterior) part of the mid-thoracic spinal cord. It can cause acute radicular pain at the level of bleeding. Subsequently, a syndrome of transverse myelopathy develops with paresthesias, followed by progressive sensory loss. Motor paresis often begins in the fingers and feet and ascends to the level of spinal cord compression. In such cases of acute neurological deterioration due to suspected epidural hematoma, immediate consultation with a neurosurgeon is indicated for potential surgical evacuation.
Acute Herniated (Extruded) Disc Causing Cord Compression
Herniation (extrusion) of intervertebral discs in the lumbar and cervical spine is a fairly common pathology in modern humans, often leading to nerve root compression (radiculopathy). Extrusion of intervertebral discs in the thoracic spine is less likely to cause symptomatic compression of the spinal cord due to the relatively larger canal-to-cord ratio and the stabilizing effect of the rib cage. Usually, thoracic disc herniations that cause spinal cord compression and myelopathy develop at this level after a significant spinal injury or in the context of severe degenerative disc disease.
Degeneration of cervical intervertebral discs (extrusion, herniation) with concomitant osteoarthritis of the intervertebral (facet) joints and hypertrophy of the posterior longitudinal ligament and ligamentum flavum (a condition known as cervical spondylosis with spinal stenosis) is a common cause of chronic myelopathy at the cervical level of the spinal cord in elderly patients. Acute, large central disc herniations at any level can also cause acute spinal cord compression.
This MRI of the cervical spine demonstrates a C5-C6 disc herniation that is compressing the spinal cord at the cervical level, leading to the development of compression myelopathy.
Other Atypical Compressive Lesions of the Spinal Cord
Glucocorticoid-Induced Epidural Lipomatosis
In patients undergoing long-term treatment of various diseases with high doses of adrenal cortex hormones (glucocorticoids), or those with primary Cushing's syndrome, there is a tendency for increased growth and deposition of epidural adipose tissue (epidural lipomatosis). Such an increase in the volume of epidural fat can, in some cases, compress the patient's thoracic or lumbar spinal cord, leading to myelopathy or cauda equina syndrome.
Rare Causes
In certain blood diseases (e.g., myeloproliferative disorders, severe anemias), compression of the spinal cord can be caused by foci of extramedullary hematopoiesis (formation of blood cells outside the bone marrow) occurring within the epidural space.
Rare diseases that can lead to compression of the spinal cord in patients include:
- Eroding aortic aneurysms (causing vertebral body erosion and potential compression).
- Echinococcal (hydatid) cysts and other parasitic cysts involving the spine or epidural space.
- Tuberculous gummas (granulomas) or Pott's disease with abscess formation.
- Lymphomatous-granulomatous processes.
- Mucopolysaccharidoses (lysosomal storage diseases causing skeletal dysplasia and potential spinal canal narrowing).
Inflammatory Joint Diseases Affecting the Spine
Inflammatory diseases of the intervertebral joints (facet joints) and discovertebral articulations can manifest in two primary clinical forms leading to potential spinal cord or nerve root compression:
- Compression of the lumbar spinal cord (conus medullaris) or cauda equina as a result of advanced ankylosing spondylitis, leading to ossification, spinal stenosis, or atlantoaxial instability.
- Compression of the cervical segments of the spinal cord due to destruction and instability of the cervical apophyseal (facet) joints or the atlantoaxial joint (between C1 and C2 vertebrae) in severe rheumatoid arthritis.
This MRI of the cervical spine reveals arthropathy of the atlantoaxial joint (between C1 and C2) and erosive changes in the odontoid process (dens) of the C2 vertebra. These changes are causing compression myelopathy in a patient with rheumatoid arthritis.
Complications from joint damage in rheumatoid arthritis that cause effects on the spinal cord are often overlooked by physicians if not specifically considered. Anterior subluxation of the bodies of the cervical vertebrae, or specifically of the atlas (C1) relative to the second cervical vertebra (axis, C2) due to ligamentous laxity and erosions, can lead to significant damage to the spinal cord, potentially up to a fatal outcome in the case of acute compression after a minor injury (whiplash injury of the neck, cervico-occipital syndrome). In milder cases, the patient may develop chronic compression myelopathy, similar in presentation to that seen with cervical spondylosis. The separation (os odontoideum) or fracture of the odontoid process from C2 can also cause narrowing (stenosis) of the upper part of the spinal canal with compression at the junction of the medulla oblongata and spinal cord, especially in positions involving flexion of the neck with the head tilted forward.
Differential Diagnosis of Spinal Cord Compression Syndromes
Differentiating the cause of spinal cord compression is critical for appropriate management. A comprehensive approach is needed.
| Cause of Compression | Key Differentiating Features |
|---|---|
| Extradural Tumors (e.g., Metastases, Lymphoma) | Back pain often prominent, precedes neurological deficits. Rapid progression possible. History of primary cancer. MRI shows extradural mass, often with vertebral involvement. |
| Intradural Extramedullary Tumors (e.g., Meningioma, Schwannoma) | Slower progression. Radicular pain common early. Asymmetric neurological deficits. MRI shows well-defined intradural mass displacing cord. CSF protein often high. |
| Intramedullary Tumors (e.g., Ependymoma, Astrocytoma, Metastasis) | Poorly localized pain or dysesthesia. Central cord syndrome features (dissociated sensory loss, sacral sparing). MRI shows intrinsic cord expansion and enhancement. |
| Spinal Epidural Abscess | Fever, severe localized back pain, rapidly progressive neurological deficits. Elevated inflammatory markers. MRI shows epidural collection with rim enhancement, often associated discitis/osteomyelitis. |
| Spinal Epidural Hematoma | Sudden onset severe back pain and neurological deficits. Often history of trauma, anticoagulation, or spinal procedure. MRI shows epidural blood collection. |
| Acute Disc Herniation | Often acute onset of radicular pain, may progress to myelopathy if large central herniation. MRI confirms disc herniation compressing neural structures. |
| Cervical Spondylotic Myelopathy | Older age, chronic progressive course. Gait disturbance, clumsiness, UMN signs. MRI shows multilevel degenerative changes, cord compression from discs/osteophytes. |
| Traumatic Fracture/Dislocation | Clear history of significant trauma. Immediate or delayed onset of neurological deficits. Imaging shows fracture/dislocation with canal compromise. |
General Principles of Management and Prognosis
The management of spinal cord compression is a medical emergency, especially if neurological deficits are acute or progressive. Key principles include:
- Stabilization: Medical and spinal stabilization as needed.
- Corticosteroids: High-dose corticosteroids (e.g., dexamethasone) are often given immediately if neoplastic cord compression is suspected, to reduce edema and temporarily relieve symptoms. Their role in other compressive etiologies is more varied.
- Definitive Treatment of the Cause:
- Surgical Decompression: For most compressive lesions causing neurological deficits (e.g., tumors, abscesses, hematomas, severe disc herniations, fractures). The goal is to remove the compressing agent and relieve pressure on the spinal cord.
- Radiation Therapy: For radiosensitive tumors (e.g., metastases, lymphoma), often used adjunctively or as primary treatment if surgery is not feasible.
- Antibiotics: For infectious causes like epidural abscess.
- Chemotherapy: For chemosensitive systemic malignancies with spinal involvement.
- Supportive Care and Rehabilitation: Including pain management, bladder/bowel care, prevention of complications (DVT, pressure sores), and intensive neurological rehabilitation.
The prognosis after spinal cord compression depends on the underlying cause, the severity and duration of compression, the rapidity of onset of neurological deficits, and the timeliness and effectiveness of treatment. Early intervention generally leads to better neurological outcomes.
When to Seek Urgent Medical Attention
Immediate medical evaluation (often in an emergency department) is crucial if an individual develops:
- New or worsening weakness or paralysis in the limbs.
- New or worsening numbness or sensory loss, especially if there is a clear sensory level.
- Sudden onset or worsening of bowel or bladder dysfunction (incontinence or retention).
- Severe, unrelenting back or neck pain, particularly if associated with fever or neurological symptoms.
- Symptoms suggestive of spinal cord compression after trauma.
- Rapidly progressive neurological decline.
Timely diagnosis and intervention are critical to minimize permanent neurological damage from spinal cord compression.
References
- Byrne TN, Waxman SG. Spinal Cord Compression: Diagnosis and Principles of Management. F.A. Davis Company; 1990.
- Loblaw DA, Perry J, Chambers A, Laperriere NJ. Systematic review of the diagnosis and management of malignant extradural spinal cord compression: the Cancer Care Ontario Practice Guidelines Initiative's Neuro-Oncology Disease Site Group. J Clin Oncol. 2005 Mar 20;23(9):2028-37.
- Cole JS, Patchell RA. Metastatic epidural spinal cord compression. Lancet Neurol. 2008 May;7(5):459-66.
- Abram S. Spinal Cord Tumors. Am Fam Physician. 2000 Feb 15;61(4):1057-1064.
- Darouiche RO. Spinal epidural abscess. N Engl J Med. 2006 Nov 9;355(19):2012-20.
- Babu R, Hiterrows M, Guyot AM, et al. Spinal emergencies: a review. World J Emerg Surg. 2013;8(1):9.
- McCormick PC, Post KD, Stein BM. Intradural extramedullary tumors in adults. Neurosurg Clin N Am. 1990 Jul;1(3):591-608.
- Jansson KA, Bauer HC. Spinal tumors: A review. Orthopedics. 2006 Apr;29(4):311-7.
See also
- Anatomy of the spine
- Ankylosing spondylitis (Bechterew's disease)
- Back pain by the region of the spine:
- Back pain during pregnancy
- Coccygodynia (tailbone pain)
- Compression fracture of the spine
- Dislocation and subluxation of the vertebrae
- Herniated and bulging intervertebral disc
- Lumbago (low back pain) and sciatica
- Osteoarthritis of the sacroiliac joint
- Osteocondritis of the spine
- Osteoporosis of the spine
- Guidelines for Caregiving for Individuals with Paraplegia and Tetraplegia
- Sacrodinia (pain in the sacrum)
- Sacroiliitis (inflammation of the sacroiliac joint)
- Scheuermann-Mau disease (juvenile osteochondrosis)
- Scoliosis, poor posture
- Spinal bacterial (purulent) epiduritis
- Spinal cord diseases:
- Spinal spondylosis
- Spinal stenosis
- Spine abnormalities
- Spondylitis (osteomyelitic, tuberculous)
- Spondyloarthrosis (facet joint osteoarthritis)
- Spondylolisthesis (displacement and instability of the spine)
- Symptom of pain in the neck, head, and arm
- Pain in the thoracic spine, intercostal neuralgia
- Vertebral hemangiomas (spinal angiomas)
- Whiplash neck injury, cervico-cranial syndrome



.jpg)



