Herniated and bulging intervertebral disc
- Understanding Spinal Osteochondrosis and Intervertebral Disc Pathology
- Types of Intervertebral Disc Displacement (Bulging, Herniation, Sequestration)
- Radiological Classification of Herniated Discs
- Imaging Characteristics and Related Tissue Changes
- Symptoms of Herniated and Bulging Intervertebral Discs
- Diagnosis of Intervertebral Disc Pathologies
- Treatment of Herniated and Bulging Intervertebral Discs
- Differential Diagnosis of Low Back and Radiating Leg Pain
- Prevention and Lifestyle Modifications
- When to Consult a Specialist
- References
Understanding Spinal Osteochondrosis and Intervertebral Disc Pathology
Osteochondrosis of the spine is a term often used to describe a dystrophic (degenerative) pathological process affecting the spinal column. This process typically begins with changes in the intervertebral discs, subsequently leading to damage and degenerative changes in other parts of the spine, including vertebral bodies, facet joints, and ligaments. Within the spine, the cervical and lumbar regions are primarily affected by osteochondrosis due to their greater mobility and susceptibility to mechanical overload compared to the thoracic spine.
The thoracic spine, in contrast, is relatively protected and stabilized by the rib cage (ribs and sternum). Consequently, clinically significant disc protrusions or herniations at the thoracic level due to osteochondrosis are quite rare in clinical practice. When spinal osteochondrosis becomes symptomatic, it often manifests with various neurological disorders, primarily pain syndromes and radiculopathy.
Pathophysiology of Disc Degeneration and Herniation
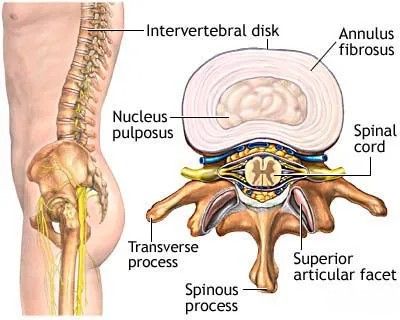
The intervertebral disc functions as a crucial "shock absorber" and pivot point between adjacent vertebral bodies. The human spine, as an axial organ, performs the vital function of supporting an upright posture while accommodating a wide range of static and dynamic loads.
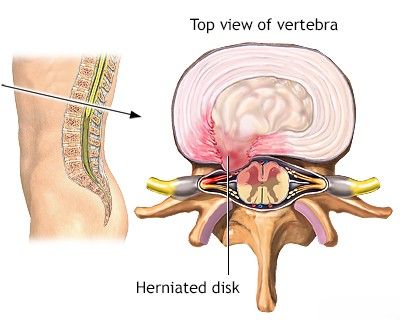
This image shows the normal structure of an intervertebral disc and adjacent vertebrae in a cross-sectional view, highlighting the nucleus pulposus and annulus fibrosus.
The intradiscal pressure within a healthy disc is normally positive, amounting to approximately 5–6 atmospheres. This inherent pressure itself makes the notion of "repositioning a fallen disc" through simple manual manipulation, as sometimes claimed by certain manual therapy practitioners, biomechanically improbable for true herniations.
Biomechanics and Risk Factors
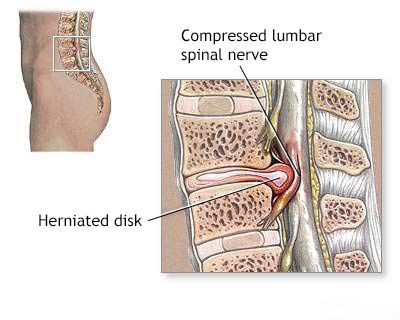
The distribution of intradiscal pressure in a person performing work in a sitting position or while slightly flexing the trunk demonstrates that the posterior (back) parts of the intervertebral disc experience somewhat less compressive load than the anterior (front) parts under these conditions. However, the nucleus pulposus tends to be displaced posteriorly with flexion. This means that intradiscal pressure, especially during flexion and loading, is often directed towards the spinal canal, exerting predominant stress on the posterior arch of the annulus fibrosus and the posterior longitudinal ligament. Consequently, the dystrophic (degenerative) process often develops first in this posterior part of the intervertebral disc, making the possibility of disc herniation towards the spinal canal (where nerve roots and the spinal cord are located) the highest.
This diagram illustrates a hernia or protrusion of the intervertebral disc extending towards the spinal canal and causing compression of an adjacent spinal nerve root.
This specific pattern of load distribution across the intervertebral disc helps to understand the higher frequency of osteochondrosis of the intervertebral disc and its complications (like herniation) in individuals with "sedentary" professions compared to those performing dynamic physical work. During dynamic work and varied movements, all parts of the intervertebral disc are loaded more or less evenly, which can decrease the likelihood of a localized dystrophic lesion developing in one specific part of the disc.
When examining patients with pain in the lower back and leg using imaging modalities like Computed Tomography (CT) or Magnetic Resonance Imaging (MRI), the following signs characteristic of herniated forms of lumbar spine osteochondrosis may be revealed:
Types of Intervertebral Disc Displacement (Bulging, Herniation, Sequestration)
Changes in the contour and size of the intervertebral disc, as visualized on imaging, are primary and constant signs indicating disc pathology. A disc protrusion is frequently observed and is often accompanied by a decrease in its height. In such cases, part of the intervertebral disc extends beyond the normal boundaries of the adjacent vertebral bodies. While similar changes can occur in middle-aged individuals without causing painful sensations (asymptomatic disc bulges), potentially leading to overdiagnosis of clinically significant hernias or protrusions, the relationship between the disc edge and the vertebral body edge is important. Normally, these edges correspond closely. In pathological conditions, the cartilaginous tissue of the intervertebral disc extends beyond the border of the vertebral bodies.
In the practical work of a neurosurgeon, it is crucial to determine the specific type of intervertebral disc herniation present in a patient, as this influences treatment decisions and prognosis. The main types include protrusion, prolapse (extrusion), and sequestration.
Normally, the edges of the vertebral body and the edges of the intervertebral disc are well-aligned and correspond to each other. Pathological displacement signifies disc abnormality.
Intervertebral Disc Protrusion (Bulging Disc)
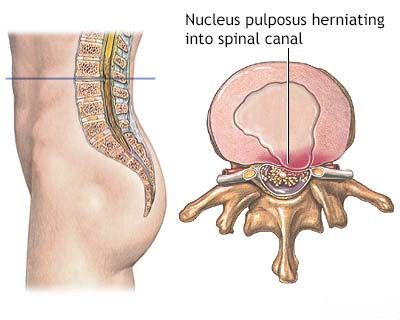
With an intervertebral disc protrusion (often called a bulging disc), there is a localized or diffuse bulging of the disc material beyond the edges of the vertebral bodies. Terminologically, "local protrusion" and "disc protrusion" are often used interchangeably and generally represent different degrees of the same condition, where the disc bulges but the outer fibers of the annulus fibrosus remain intact. In this scenario, the nucleus pulposus (the inner gelatinous part of the disc) remains contained within the stretched but unbroken fibers of the annulus fibrosus.
Intervertebral Disc Prolapse or Extrusion (Herniated Disc)
A disc prolapse, or extruded disc (commonly referred to as a herniated disc), occurs when the nucleus pulposus penetrates through a tear or rupture in the annulus fibrosus. In this case, fragments of the nucleus pulposus are displaced outside the confines of the annulus but may still be contained by the posterior longitudinal ligament, which runs along the back of the vertebral bodies and discs. It is not always possible to definitively distinguish between a large protrusion and a subligamentous extrusion based solely on CT scans of the spine. In such cases, MRI or, historically, discography (an invasive procedure involving contrast injection into the disc) might be necessary for clearer differentiation.
Intervertebral Disc Sequestration or Fragmentation
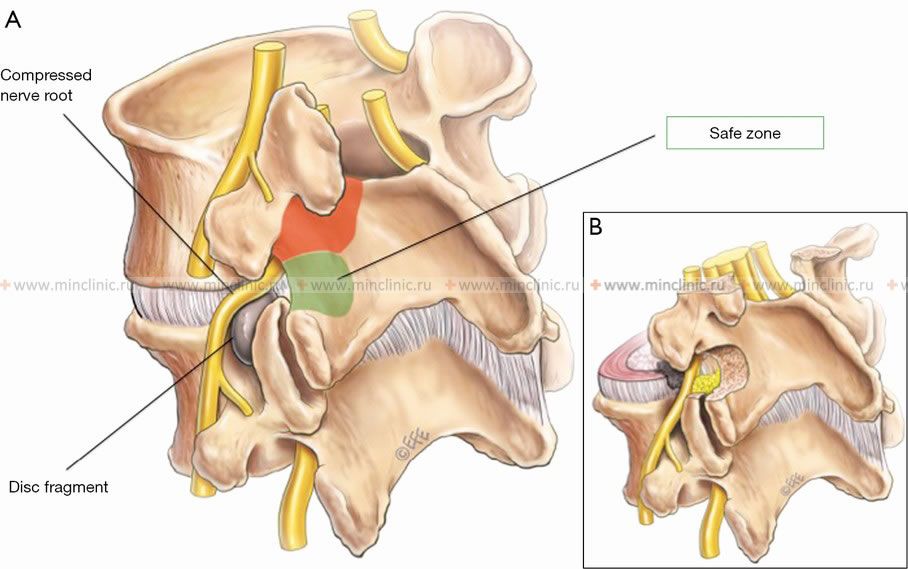
With sequestration or fragmentation of the disc, extruded disc material (a free fragment of the nucleus pulposus) completely separates from the parent disc and is no longer contained by the annulus fibrosus or the posterior longitudinal ligament. This sequestered fragment then lies freely within the epidural space (the space surrounding the dural sac within the spinal canal). Such free fragments can migrate superiorly (cranially), inferiorly (caudally), or laterally from the level of the original disc. Very rarely, a disc fragment can penetrate the dura mater and become intradural (within the dural sac itself).
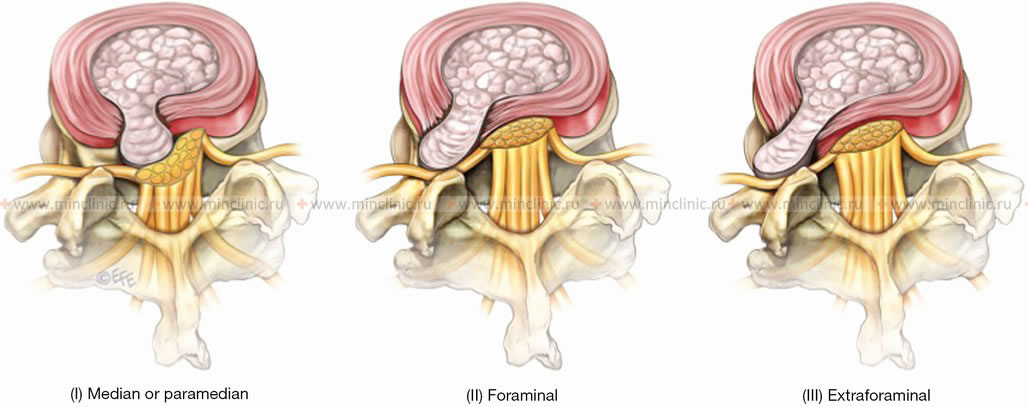
Relationship to Nerve Roots
The usual rule is that a paracentral or posterolateral disc herniation compresses the nerve root that exits at the level *below* the affected intervertebral disc. For example, a herniation or protrusion of the L4–L5 intervertebral disc typically compresses (squeezes) the L5 nerve root. However, with a far lateral (foraminal or extraforaminal) herniation or protrusion of the intervertebral disc, the nerve root exiting at the *same level* within the intervertebral foramen can be compressed. In this scenario, an L4–L5 far lateral disc herniation would compress the L4 nerve root.
This illustration depicts the compression of a spinal nerve root by a herniated or protruding intervertebral disc, a common complication of spinal osteochondrosis.
Radiological Classification of Herniated Discs
Radiological classifications help standardize the description of herniated discs based on their appearance on imaging studies (primarily MRI and CT).
Location-Based Classification
Hernias or protrusions of the intervertebral disc are subdivided according to their anatomical localization, primarily based on their relation to the anterior wall of the spinal canal and the neural foramina:
- Diffuse or Total Bulge/Protrusion: Generalized circumferential extension of the disc beyond the vertebral body edges.
- Central or Median Hernia/Protrusion: Displacement of disc material directly posterior in the midline.
- Paracentral or Paramedian Hernia/Protrusion: Displacement just off the midline, typically located between the midline and a line connecting the medial edges of the articular processes (facet joints). This is a very common location.
- Lateral or Foraminal Hernia/Protrusion: Displacement of disc material into the intervertebral foramen (the bony canal through which the nerve root exits), located outside the inner edge of the articular processes.
- Far Lateral or Extraforaminal Hernia/Protrusion: Displacement of disc material lateral to the intervertebral foramen.
This location-based classification of herniated or protruded intervertebral discs seems to be the most convenient and clinically relevant for the operating neurosurgeon, as it dictates the surgical approach if intervention is required. It is important to note that clinical manifestations in various types of disc herniations or protrusions may not always perfectly correlate with their precise radiological characteristics. For example, a disc herniation that appears median on imaging might clinically manifest as a lateral or paramedian syndrome (affecting one nerve root), or, in some extreme cases, a radiologically evident disc pathology can be an incidental finding without significant clinical symptoms.
MRI of the cervical spine is frequently prescribed for clinical manifestations suggestive of a hernia or protrusion of an intervertebral disc, such as the C5-C6 disc herniation causing myelopathy indicated by the arrow.
MRI Classification of Lumbar Intervertebral Disc Degeneration (Pfirrmann)
The Pfirrmann classification is a widely used system to grade the severity of lumbar intervertebral disc degeneration based on MRI signal intensity and structural changes observed on T2-weighted sagittal images. It primarily assesses the hydration and integrity of the nucleus pulposus and the distinction between the nucleus and annulus fibrosus, as well as disc height.
| Pfirrmann Grade | Description of Disc Appearance on T2-weighted MRI |
|---|---|
| Grade I (Normal) | Homogeneous, bright hyperintense (white) signal intensity of the disc structure. Clear distinction between nucleus pulposus and annulus fibrosus. Normal disc height. |
| Grade II (Early Degeneration) | Inhomogeneous disc structure with hyperintense (white) signal. Possible presence of horizontal hypointense (dark) stripes within the nucleus. Clear distinction between nucleus and annulus. Normal disc height. |
| Grade III (Moderate Degeneration) | Inhomogeneous disc structure with intermediate gray signal intensity. Unclear separation between nucleus pulposus and annulus fibrosus. Disc height normal or slightly decreased. |
| Grade IV (Advanced Degeneration) | Inhomogeneous disc structure with hypointense (dark gray to black) signal. Loss of distinction between nucleus and annulus. Disc height slightly or moderately reduced. |
| Grade V (Severe Degeneration / Collapse) | Homogeneous hypointense (black) disc structure. Loss of distinction between nucleus and annulus. Collapse (significant decline) of the intervertebral disc space. |
Sagittal MRI images of the lumbar spine in T2-weighted mode are primarily used to assess intervertebral disc degeneration according to this classification. For example:
- Image A might show severe degeneration of intervertebral discs according to Pfirrmann: mostly heterogeneous black discs without any clear separation between the nucleus and the annulus fibrosus; with collapse (significant height loss) of discs at the L1-L2 and L4-L5 vertebral levels (consistent with Grade V).
- Image B might demonstrate lumbar intervertebral discs with high elasticity and a low degree of degeneration according to Pfirrmann; a homogeneous structure of discs with a bright hyperintense signal and normal height would be visible (consistent with Grade I or II).
Sagittal T2-weighted MRI images of the lumbar spine are used to assess intervertebral disc degeneration based on the Pfirrmann classification. A. Example showing advanced degeneration: mostly heterogeneous black discs with no clear separation between nucleus and annulus; collapse of discs at L1-L2 and L4-L5 (Pfirrmann Grade V). B. Example showing lumbar discs with high elasticity and low degeneration: homogeneous, bright hyperintense discs with normal height (Pfirrmann Grade I/II).
Imaging Characteristics and Related Tissue Changes
Changes in Physical Properties of the Intervertebral Disc
Densitometric examination of the intervertebral disc using CT can reveal changes in tissue density. In some cases, an increase in the density of the nucleus pulposus tissues may be observed due to calcification, a sign of chronic degeneration. In other instances, a decrease in the density of the nucleus can be seen, indicating loss of hydration or degenerative changes. By assessing the densitometric density, one can sometimes indirectly judge the chronicity or "age" of an intervertebral disc herniation. "Young" or acute hernias or protrusions of the intervertebral disc tend to have a more homogeneous structure with a density typically ranging from 60–80 Hounsfield Units (HU) and may not always have sharply defined contours. Long-standing or chronic intervertebral hernias or protrusions often exhibit higher density (due to fibrosis or calcification) and a more heterogeneous structure. A particularly striking sign of advanced nucleus pulposus dystrophy is the appearance of air or gas cavities within the intervertebral disc, known as the "vacuum phenomenon" or "vacuum disc sign," which appears as very low density (air-like) on CT.
Changes in Tissues Around the Intervertebral Disc
The epidural space, located between the dural sac and the bony spinal canal, normally contains epidural fat, blood vessels, and nerve roots. Pathological changes in this space can be indicative of disc herniation or its consequences. The most significant changes in the epidural tissue are often determined at the level of the lower lumbar discs (L4-L5, L5-S1). The epidural space at the L5–S1 intervertebral disc level is typically wider and contains a significant number of epidural veins (e.g., Batson's venous plexus), which on CT of the spine can appear as a soft tissue component located symmetrically near the disc. Posterior to the vertebral body, in the midline, Batson's venous plexus itself can look like a soft tissue formation, and this normal anatomical structure can sometimes be mistaken for a sequestered herniated disc if not carefully evaluated, especially on non-contrast CT.
The dura mater and nerve roots are normally surrounded by epidural fat, which provides a natural contrast on CT and MRI. Changes in this adipose tissue can also be determined densitometrically or by signal intensity on MRI. Inhomogeneity of the densitometric density or loss of normal fat signal intensity around the nerve roots or dural sac may indicate an inflammatory or adhesive process (epidural fibrosis or scarring), often secondary to chronic disc pathology or previous surgery.
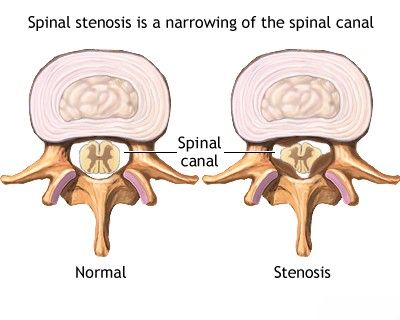
Spinal stenosis (narrowing of the spinal canal) with resultant compression of the spinal cord or cauda equina can be caused by disc herniation, ligamentous hypertrophy, or bony overgrowth, all contributing to changes in tissues around the neural elements.
Obliteration of the epidural space by tissues of increased density or the presence of an abnormal soft tissue component at the level of the disc is highly suggestive of sequestration of the nucleus pulposus. In addition, it is sometimes possible to determine an increase in the volume of epidural tissue below the level of a hernia or protrusion of the intervertebral disc, which can be associated with the expansion or engorgement of epidural veins caudal (below) to the level of compression due to impaired venous return.
Changing the Contour or Position of the Dural Sac
With median (central) or paramedian (paracentral) hernias or protrusions of intervertebral discs, the dural sac (the sheath containing the spinal cord and nerve roots) is often displaced posteriorly (backward). On axial CT or MRI images, the dural sac may take on a deformed shape, appearing bean-shaped or crescent-shaped due to the indentation from the disc material. With lateral hernias or protrusions, the dural sac may be displaced towards the contralateral (opposite) side. Only in the case of very far lateral (foraminal or extraforaminal) hernias or protrusions of intervertebral discs might the dural sac itself be considered intact or minimally affected, as the compression primarily occurs on the exiting nerve root within or lateral to the neural foramen.
Changing the Position of the Nerve Roots
The spinal nerve roots are key structures affected by disc herniations. Most often, the nerve roots in the zone of conflict with the herniated disc material are poorly visualized on imaging, which is especially characteristic of sequestered hernias or protrusions where the fragment may be surrounded by inflammation or scar tissue. In such cases, the proposed location of the compressed or displaced nerve root can often be inferred by tracing its imaginary trajectory, connecting the visible "pre-herniation" segment of the root (before it enters the area of compression) and the "post-herniation" segment (after it exits the area of compression).
In other instances, a herniated disc clearly displaces the nerve root, often posteriorly, medially, or laterally, depending on the location of the herniation. The displacement is usually asymmetrical. With large sequestered hernias or protrusions and a pronounced adhesive process (scarring), the herniated disc material and surrounding epidural tissues (paradiscal tissues) may not be clearly differentiated on imaging and can appear as a single conglomerate mass.
CT changes specifically related to the extrasaccal (outside the dural sac, i.e., within the neural foramen or lateral recess) portion of the nerve root can also be distinguished, including:
- Dislocation: The nerve root is pushed from its normal position.
- Aggregation: Nerve roots may appear clumped together due to compression or inflammation (more common in severe cauda equina compression).
- Compression: The nerve root is visibly flattened or indented by the disc material.
- Conglomeration: Nerve roots and surrounding inflamed/scarred tissues form an indistinct mass.
Symptoms of Herniated and Bulging Intervertebral Discs
The clinical presentation of intervertebral disc herniation or bulging varies greatly depending on the location (cervical, thoracic, or lumbar spine), the size and type of herniation, and whether it compresses nerve roots or the spinal cord.
- Low Back Pain or Neck Pain: Often the initial symptom, can be dull or sharp, localized or diffuse.
- Radicular Pain: Sharp, shooting pain radiating along the course of a compressed nerve root.
- Sciatica: Pain radiating from the buttock down the leg (posterior or lateral thigh, calf, foot) due to lumbar nerve root compression (commonly L4, L5, S1).
- Cervical Radiculopathy: Pain radiating from the neck into the shoulder, arm, forearm, or hand.
- Numbness and Tingling (Paresthesia): In the area supplied by the compressed nerve root.
- Muscle Weakness: In muscles innervated by the affected nerve root (e.g., foot drop with L5 radiculopathy, weakness in arm/hand with cervical radiculopathy).
- Altered Reflexes: Diminished or absent deep tendon reflexes corresponding to the affected nerve root.
- Myelopathy (if spinal cord compression occurs, e.g., large central cervical or thoracic disc herniation): Symptoms can include gait disturbance, balance problems, spasticity, weakness in multiple limbs, bowel/bladder dysfunction, and sensory changes below the level of compression.
- Cauda Equina Syndrome (lumbar disc herniation - a surgical emergency): Characterized by severe low back pain, bilateral sciatica, saddle anesthesia (numbness in the groin, buttocks, inner thighs), bowel and/or bladder dysfunction (retention or incontinence), and significant leg weakness.
It's important to note that many individuals may have asymptomatic disc protrusions or bulges found incidentally on imaging.
Diagnosis of Intervertebral Disc Pathologies
Diagnosis involves a comprehensive approach:
- Medical History: Detailed account of symptoms, onset, aggravating/relieving factors, previous injuries or back/neck problems.
- Physical Examination:
- Assessment of spinal range of motion, posture, and palpation for tenderness or muscle spasm.
- Neurological examination: testing muscle strength, sensation (light touch, pinprick), deep tendon reflexes, and specific provocative tests (e.g., Straight Leg Raise/Lasegue's test for lumbar radiculopathy, Spurling's maneuver for cervical radiculopathy).
- Imaging Studies:
- MRI (Magnetic Resonance Imaging): The gold standard for visualizing intervertebral discs, nerve roots, and the spinal cord. It can clearly show disc herniations, protrusions, sequestrations, and their impact on neural structures.
- CT Scan (Computed Tomography): Provides excellent detail of bony structures and can also identify disc herniations, especially if combined with myelography (CT myelogram). Often used if MRI is contraindicated.
- X-rays: Can show degenerative changes in the spine (e.g., disc space narrowing, osteophytes), alignment issues, or fractures, but do not directly visualize discs or nerves. Often used as an initial screening tool.
- Electromyography (EMG) and Nerve Conduction Studies (NCS): Can help confirm nerve root damage (radiculopathy) and differentiate it from peripheral neuropathy, especially if the diagnosis is unclear or if assessing the severity of nerve involvement.
Treatment of Herniated and Bulging Intervertebral Discs
The treatment approach depends on the severity of symptoms, the type and location of the disc pathology, the presence of neurological deficits, and the patient's overall health and preferences.
Conservative Therapy
At the first stage of treating a patient with symptomatic herniated disc or protrusion, an intensive course of conservative therapy is often proposed. This typically lasts up to 5-6 days (for acute phases, longer for overall conservative management) and can be carried out on an outpatient basis. Clinical practice shows that in approximately 50% of cases in patients with clinical manifestations of nerve root compression by a herniated intervertebral disc, it is possible to achieve a significant reduction or complete elimination of pain symptoms, along with restoration of impaired sensation and existing muscle weakness, through conservative measures alone.
Conservative treatment options include:
- Activity Modification and Relative Rest: Avoiding activities that worsen pain, but prolonged bed rest is generally discouraged. Gradual return to activity is key.
- Pharmacological Therapy:
- NSAIDs (Nonsteroidal Anti-Inflammatory Drugs) to reduce pain and inflammation.
- Analgesics (pain relievers) like acetaminophen.
- Muscle relaxants for acute muscle spasms.
- Neuropathic pain medications (e.g., gabapentin, pregabalin) for radicular pain.
- Oral corticosteroids (e.g., prednisone) for a short course to reduce severe inflammation in acute radiculopathy.
- Therapeutic Injections:
- Epidural steroid injections to deliver anti-inflammatory medication directly to the area of nerve root irritation.
- Selective nerve root blocks.
- Facet joint injections if facet pain coexists.
- Manual Therapy: Techniques performed by qualified practitioners (chiropractors, osteopaths, physical therapists) such as spinal mobilization or manipulation. Non-surgical "reduction" of a vertebral disc herniation using specific muscle, articular, and radicular techniques may be attempted by some, aiming to decompress neural structures and improve biomechanics.
- Physiotherapy (Physical Therapy): A cornerstone of conservative care, including:
- Specific exercises for core strengthening, stabilization, and flexibility (e.g., McKenzie method, dynamic lumbar stabilization).
- Postural education and correction of movement patterns.
- Modalities like heat, cold, TENS (Transcutaneous Electrical Nerve Stimulation), or UHF therapy to alleviate pain and muscle spasm.
- Acupuncture: May provide pain relief for some individuals.
The application of physiotherapy is crucial for eliminating swelling (puffiness) and inflammation, alleviating pain, and restoring the range of motion in the joints and muscles of the lower back when treating spinal osteochondrosis complicated by a hernia or protrusion of an intervertebral disc.
Surgical Treatment
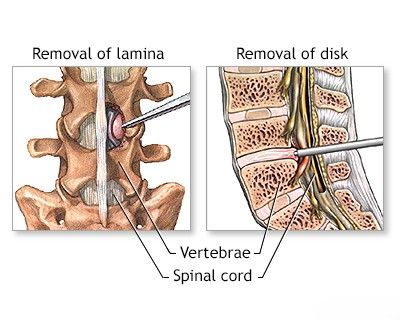
If conservative therapy is ineffective after an adequate trial (typically 6-12 weeks), or if there are significant or progressive neurological deficits, or signs of cauda equina syndrome, surgical treatment is considered. The goal of surgery is to decompress the affected nerve root(s) or spinal cord by removing the herniated disc material.
Common surgical procedures include:
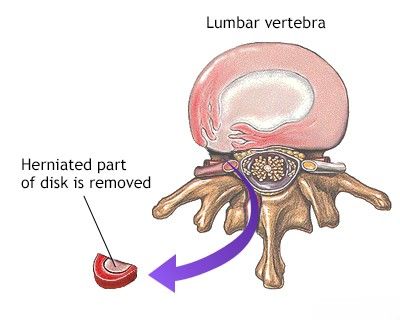
- Microdiscectomy: A minimally invasive procedure to remove the herniated portion of the disc.
- Laminectomy/Laminotomy: Removal of part of the vertebral lamina to create more space for neural elements.
- Foraminotomy: Enlarging the intervertebral foramen to relieve nerve root compression.
- Spinal Fusion: May be performed in cases of associated spinal instability or severe degenerative changes, often in conjunction with decompression.
- Artificial Disc Replacement: An alternative to fusion in selected cases, aiming to preserve motion.
Endoscopic techniques are increasingly used for disc surgery, offering minimally invasive access. The access scheme during endoscopic surgery to remove a hernia or protrusion of an intervertebral disc of the lumbar spine might involve a posterolateral or transforaminal approach. For foraminal and extraforaminal fragments compressing a nerve root, an inter-articular (between facet joints) endoscopic operative access may be utilized. During such procedures, the extruded fragment of the disc is carefully removed to decompress the neural structures.
This diagram illustrates a common access scheme used during endoscopic surgery for the removal of a hernia or protrusion of an intervertebral disc in the lumbar spine.
An inter-articular endoscopic operative access route may be utilized for addressing foraminal and extraforaminal fragments of a herniated intervertebral disc that are compressing a nerve root.
During an endoscopic surgical procedure to remove a hernia or protrusion of an intervertebral disc in the lumbar spine, the extruded or sequestered fragment of the disc that has "fallen out" is carefully removed to decompress the neural structures.
Important Considerations for Cauda Equina Syndrome
![]() Attention! Conservative treatment is **not** performed and is contraindicated in patients presenting with symptoms of cauda equina compression. Cauda equina syndrome is manifested by severe low back pain, bilateral sciatica, saddle anesthesia (numbness in the perineal region), and significant dysfunction of the pelvic organs (such as urinary retention or incontinence, fecal incontinence). This neurological complication in a patient is an **absolute indication for urgent neurosurgical intervention**, which must be performed emergently to decompress the cauda equina nerve roots and maximize the chances of neurological recovery.
Attention! Conservative treatment is **not** performed and is contraindicated in patients presenting with symptoms of cauda equina compression. Cauda equina syndrome is manifested by severe low back pain, bilateral sciatica, saddle anesthesia (numbness in the perineal region), and significant dysfunction of the pelvic organs (such as urinary retention or incontinence, fecal incontinence). This neurological complication in a patient is an **absolute indication for urgent neurosurgical intervention**, which must be performed emergently to decompress the cauda equina nerve roots and maximize the chances of neurological recovery.
Differential Diagnosis of Low Back and Radiating Leg Pain
While disc herniation is a common cause, other conditions can mimic its symptoms:
| Condition | Key Differentiating Features |
|---|---|
| Lumbar Disc Herniation | Radicular pain (sciatica), numbness, weakness in dermatomal/myotomal pattern. Positive SLR. MRI confirms disc displacement impinging on nerve root. |
| Lumbar Spinal Stenosis | Neurogenic claudication (leg pain/numbness with walking/standing, relieved by sitting/flexion). Often bilateral. MRI/CT shows canal narrowing. |
| Facet Joint Arthropathy (Spondyloarthrosis) | Low back pain, sometimes referring to buttock/thigh (rarely below knee). Pain worse with extension, twisting. Tenderness over facet joints. |
| Sacroiliac Joint Dysfunction/Sacroiliitis | Pain over SI joint, buttock, groin, sometimes referring down posterior thigh. Positive SI joint provocative tests. |
| Piriformis Syndrome | Buttock pain, may radiate down posterior thigh (sciatic nerve irritation by piriformis muscle). Tenderness over piriformis. SLR may be negative or pain localized to buttock. |
| Myofascial Pain Syndrome | Localized or regional muscle pain with trigger points in paraspinal, gluteal, or hip muscles. Pain referral patterns from trigger points. |
| Spondylolisthesis | Low back pain, may have radicular symptoms if nerve root compression due to vertebral slippage. X-rays (especially flexion-extension) confirm. |
| Hip Pathology (e.g., Osteoarthritis, Bursitis) | Groin pain, lateral hip pain, pain with hip movements. Can sometimes refer to buttock or thigh. |
| Peripheral Neuropathy | Often bilateral, stocking-glove distribution of numbness/tingling/pain. Reflexes may be diminished. EMG/NCS helpful. |
Prevention and Lifestyle Modifications
While not all disc problems can be prevented, certain measures can reduce the risk:
- Maintaining a healthy weight.
- Regular exercise with a focus on core strength and flexibility.
- Using proper lifting techniques.
- Practicing good posture.
- Ergonomic workspace setup.
- Avoiding smoking, which can accelerate disc degeneration.
When to Consult a Specialist
Consultation with a neurosurgeon, orthopedic spine specialist, or pain management physician is recommended if:
- Back pain or radiating leg pain is severe or persistent despite conservative home care.
- There are significant or progressive neurological deficits (weakness, numbness).
- Symptoms of cauda equina syndrome develop (this is a medical emergency).
- Conservative treatment fails to provide adequate relief after several weeks.
- The diagnosis is uncertain.
A specialist can provide an accurate diagnosis and discuss the full range of treatment options, including whether surgery is appropriate.
References
- Fardon DF, Williams AL, Dohring EJ, et al. Lumbar disc nomenclature: version 2.0: Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J. 2014 Nov 1;14(11):2525-45.
- Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila Pa 1976). 2006 Nov 1;31(23):2724-7.
- Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006 Nov 22;296(20):2441-50.
- Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001 Sep 1;26(17):1873-8.
- Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014 Jan;14(1):180-91.
- Jordan J, Konstantinou K, O'Dowd J. Herniated lumbar disc. BMJ Clin Evid. 2011;2011:1118.
- Valat JP, Genevay S, Marty M, Rozenberg S, Koes B. Sciatica. Best Pract Res Clin Rheumatol. 2010 Apr;24(2):241-52.
- Cohen SP, Argoff CE, Carragee EJ. Management of low back pain. BMJ. 2008 Dec 4;337:a2718.
See also
- Anatomy of the spine
- Ankylosing spondylitis (Bechterew's disease)
- Back pain by the region of the spine:
- Back pain during pregnancy
- Coccygodynia (tailbone pain)
- Compression fracture of the spine
- Dislocation and subluxation of the vertebrae
- Herniated and bulging intervertebral disc
- Lumbago (low back pain) and sciatica
- Osteoarthritis of the sacroiliac joint
- Osteocondritis of the spine
- Osteoporosis of the spine
- Guidelines for Caregiving for Individuals with Paraplegia and Tetraplegia
- Sacrodinia (pain in the sacrum)
- Sacroiliitis (inflammation of the sacroiliac joint)
- Scheuermann-Mau disease (juvenile osteochondrosis)
- Scoliosis, poor posture
- Spinal bacterial (purulent) epiduritis
- Spinal cord diseases:
- Spinal spondylosis
- Spinal stenosis
- Spine abnormalities
- Spondylitis (osteomyelitic, tuberculous)
- Spondyloarthrosis (facet joint osteoarthritis)
- Spondylolisthesis (displacement and instability of the spine)
- Symptom of pain in the neck, head, and arm
- Pain in the thoracic spine, intercostal neuralgia
- Vertebral hemangiomas (spinal angiomas)
- Whiplash neck injury, cervico-cranial syndrome