Neuropathies and neuralgia
- Understanding Neuropathies and Neuralgia
- Diagnosis of Neuropathy and Neuralgia
- Treatment of Neuropathy and Neuralgia
- Differential Diagnosis of Neuropathic Symptoms
- Prognosis and Potential Complications
- Prevention Strategies
- When to Consult a Specialist (Neurologist, Neurosurgeon, Pain Specialist)
- References
Understanding Neuropathies and Neuralgia
Neuropathies and neuralgias encompass a broad spectrum of disorders affecting the peripheral nervous system. These conditions can cause a variety of symptoms, including pain, sensory disturbances, muscle weakness, and autonomic dysfunction, depending on the nerves involved and the nature of the damage.
Definitions: Neuropathy, Polyneuropathy, Neuritis, Neuralgia
- Neuropathy: A general term referring to a persistent lesion, damage, or dysfunction of one or more peripheral nerves. It can involve motor, sensory, and/or autonomic fibers.
- Mononeuropathy: Affects a single peripheral nerve (e.g., carpal tunnel syndrome affecting the median nerve).
- Mononeuritis Multiplex: Affects two or more individual nerves in separate parts of the body (often due to vasculitis).
- Polyneuropathy: A widespread, often symmetrical, dysfunction of multiple peripheral nerves throughout the body (e.g., diabetic polyneuropathy).
- Neuritis: Specifically implies inflammation of a nerve or nerves. While many neuropathies have an inflammatory component, "neuropathy" is the broader term. "Polyneuritis" is an older term often used interchangeably with polyneuropathy but again implies inflammation as the primary cause.
- Neuralgia: Characterized by pain along the course of a nerve or in its area of innervation. The pain is typically sharp, stabbing, burning, or electric shock-like and results from irritation or damage to a sensory nerve or a mixed nerve with sensory components.
Symptoms arise from the affected nerve's zone of innervation.
Common Types of Neuropathies and Neuralgia
Some of the most common types of neuropathies, polyneuropathies, and neuralgias encountered in clinical practice include:
- Alcoholic Polyneuropathy: Nerve damage due to chronic excessive alcohol consumption and associated nutritional deficiencies.
- Diabetic Polyneuropathy: A common complication of diabetes mellitus affecting sensory, motor, and autonomic nerves.
- Intercostal Neuralgia: Pain along an intercostal nerve, often associated with herpes zoster ("shingles").
- Trigeminal Neuralgia: Severe facial pain in the distribution of the trigeminal nerve.
- Facial Nerve Neuritis (Bell's Palsy, Post-Traumatic Neuropathy): Inflammation or damage to the facial nerve causing facial muscle weakness or paralysis.
- Trigeminal Neuritis: Inflammation of the trigeminal nerve, often causing sensory changes or pain.
- Optic Neuritis: Inflammation of the optic nerve, causing vision loss and eye pain.
- Radial Nerve Neuropathy: Affects muscles and sensation in the posterior arm, forearm, and hand (e.g., wrist drop).
- Median Nerve Neuropathy: Commonly known as Carpal Tunnel Syndrome when compressed at the wrist.
- Ulnar Nerve Neuropathy: Often due to compression at the elbow (cubital tunnel syndrome) or wrist (Guyon's canal).
- Sciatic Nerve Neuropathy: Affects the large nerve in the posterior thigh, leading to leg weakness and sensory loss.
- Tibial Nerve Neuropathy: Affects muscles and sensation in the posterior leg and sole of the foot.
- Fibular (Peroneal) Nerve Neuropathy: Commonly causes foot drop.
- Traumatic Neuropathy: Nerve damage resulting from physical injury, such as post-injection neuritis or neuropathy after bone fractures.
- Small Fiber Sensory Neuropathy (SFSN): Affects small sensory nerves, causing pain and temperature sensation changes.
General Symptoms Based on Nerve Damage Level
Depending on the type of nerve fibers damaged (motor, sensory, autonomic) and the anatomical level of the lesion in neuritis (neuropathy) or polyneuropathy (polyneuritis), a patient will manifest a variety of symptoms. Sensory disorders, such as numbness, tingling (paresthesias), or "chills" (dysesthesias or altered temperature sensation), will present at different levels corresponding to the affected nerve's distribution.
More broadly, symptoms can include:
- Motor disturbances: Weakness (paresis) or complete paralysis in a particular muscle or group of muscles. This can lead to functional impairments like foot drop or wrist drop, difficulty with fine motor skills, or gait abnormalities.
- Sensory changes:
- Negative symptoms: Numbness (hypoesthesia or anesthesia), decreased sensation to touch, pain, or temperature.
- Positive symptoms: Paresthesias (tingling, pins-and-needles), dysesthesias (unpleasant abnormal sensations), hyperalgesia (increased pain sensitivity), allodynia (pain from normally non-painful stimuli), or spontaneous pain (neuralgia).
- Autonomic disturbances (if autonomic fibers are involved): Changes in sweating (hyperhidrosis or anhidrosis), skin color and temperature changes (vasomotor instability), gastrointestinal motility issues, bladder dysfunction, or orthostatic hypotension.
- Trophic disorders (long-term changes due to denervation and altered autonomic function): Muscle wasting and atrophy, cyanosis or pallor of the skin, poor healing of skin injuries, development of trophic ulcers, brittle nails, hair loss in the affected area.
Diagnosis of Neuropathy and Neuralgia
Clinical Evaluation and Neurological Examination
The diagnostic process begins with a detailed medical history and a comprehensive neurological examination. This includes:
- Assessing the nature, onset, duration, distribution, and progression of symptoms.
- Evaluating motor strength, muscle tone, and reflexes.
- Testing sensory modalities (light touch, pinprick, temperature, vibration, proprioception).
- Observing for autonomic signs and trophic changes.
- Performing specific provocative maneuvers if an entrapment neuropathy is suspected (e.g., Tinel's sign, Phalen's maneuver for carpal tunnel syndrome).
Electrodiagnostic Studies (ENG/NCS and EMG)
Classical electrodiagnostic studies, including Electroneurography (ENG), also known as Nerve Conduction Studies (NCS), and Electromyography (EMG), are of great importance in the comprehensive evaluation of neuritis (neuropathy) and polyneuritis (polyneuropathy). These tests are typically most informative from 2 weeks onwards after nerve damage, allowing time for Wallerian degeneration to occur if axons are injured. Electrodiagnostics help to:
- Confirm the presence of nerve damage.
- Differentiate between axonal loss (degenerative disorder) and demyelination (non-degenerative disorder, affecting the nerve sheath and slowing conduction), or mixed patterns.
- Localize the site of nerve injury (e.g., focal entrapment, diffuse polyneuropathy).
- Assess the severity of the neuropathy.
- Provide prognostic information regarding the potential for recovery. For example, with closed traumatic injuries to nerve trunks, such as the brachial plexus, if accompanied by significant axonal degeneration, the prognosis for complete and high-quality restoration of movements, especially in distal parts of the limb, is always doubtful.
Restoration of muscle movements to a functional strength (e.g., 4–5 points on the MRC scale) is generally observed only in those muscles where ENG/NCS reveals reduced electroexcitability or signs of partial degeneration (indicating some preserved axons capable of regeneration or collateral sprouting). If studies show a reaction of complete degeneration of the nerve (no electrical response from the muscle), restoration of movement in those muscles is typically not observed without intervention or very slow reinnervation.
In very late periods after nerve injury, the identification of complete loss of electrical excitability in paralyzed muscles provides an additional reason to reconsider or advise against surgical nerve exploration or repair, as the target muscles may have undergone irreversible atrophy and fibrosis. It has been observed, contrary to some conventional wisdom, that small intrinsic muscles of the hand often demonstrate more robust stability in their ability to respond to electrical stimulation over time compared to larger, more proximal muscles.
Electromyography (EMG) is a particularly promising research method for closed injuries of structures like the brachial plexus. It allows for the recording of the dynamics of changes in the neuromuscular apparatus during the recovery process in neuritis. The appearance of previously absent motor unit action potentials (MUAPs) on an EMG can sometimes allow clinicians to expect the restoration of movement long before the first clinical signs of such recovery become apparent.
Imaging and Other Diagnostic Tests
- Imaging (MRI, CT, Ultrasound): To visualize nerves, surrounding structures, and identify potential causes of compression (e.g., tumors, herniated discs, entrapment sites) or traumatic injury.
- Blood Tests: To screen for underlying systemic causes like diabetes, vitamin deficiencies, autoimmune diseases, infections, or exposure to toxins.
- Lumbar Puncture: For CSF analysis if inflammatory or demyelinating polyneuropathies like Guillain-Barré syndrome or CIDP are suspected.
- Nerve Biopsy: Rarely performed, but may be considered in specific cases (e.g., suspected vasculitic neuropathy, amyloid neuropathy, or undiagnosed progressive neuropathy) to obtain histological information.
- Skin Biopsy for Epidermal Nerve Fiber Density (ENFD): For diagnosing small fiber neuropathy.
Treatment of Neuropathy and Neuralgia
Treatment is selected individually for each patient and each specific case of neuropathy or neuralgia. It is crucial to consider and address the underlying cause of the neuritis or neuralgia for treatment to be effective.
The treatment of neuropathy and neuralgia should typically include a comprehensive set of conservative procedures. The primary goal is to stimulate the restoration of the nerve sheath (myelin) and its conductive properties for nerve impulses, alleviate pain, and improve function.
Common treatment modalities include:
- Addressing the Underlying Cause: This is paramount (e.g., glycemic control in diabetes, alcohol cessation, removal of toxins, treatment of infections or autoimmune conditions).
- Pharmacological Management:
- Pain relief for neuralgia: Anticonvulsants (gabapentin, pregabalin, carbamazepine), tricyclic antidepressants (amitriptyline), SNRIs (duloxetine, venlafaxine).
- Anti-inflammatory drugs (NSAIDs, corticosteroids) if inflammation is a significant component.
- Specific treatments (e.g., antiviral drugs for herpes zoster-related neuralgia).
- Vitamins, particularly B-complex ("B"), Vitamin C ("C"), and Vitamin E ("E"), are often prescribed for their neurotrophic properties and as antioxidants.
- Physical and Rehabilitative Therapies:
- Physiotherapy: To maintain range of motion, improve strength, balance, and function. Modalities like TENS, heat/cold therapy.
- Occupational Therapy: To adapt daily activities and provide assistive devices.
- Acupuncture: Can effectively help restore reduced sensitivity, relieve pain, and improve muscle weakness in the treatment of neuritis and polyneuritis of peripheral nerves.
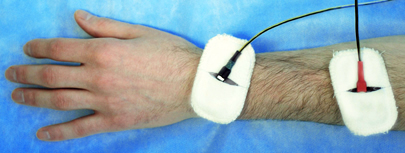
- Nerve Stimulation and Muscle Stimulation: Electrical stimulation techniques may be used to modulate pain or maintain muscle viability during reinnervation.
- Interventional Pain Management: Nerve blocks, radiofrequency ablation for certain chronic neuralgias.
- Homeopathic Remedies: Some patients explore these options, though scientific evidence for efficacy in nerve regeneration or significant pain relief is often limited.
- Surgical Treatment: Considered if conservative therapy fails or if there is a surgically correctable cause, such as:
- Neurolysis: Surgical decompression of a nerve trunk entrapped by scar tissue, fibrous bands, or in anatomical tunnels.
- Nerve Repair (Neurorrhaphy): Stitching of a severed nerve trunk.
- Nerve grafting or transfers for severe nerve injuries.
- Removal of tumors or other compressive lesions.
The duration of treatment and its frequency (number of courses) will be dictated in the future by the functional state of the nerve itself (as assessed by clinical improvement and follow-up ENG/EMG), the condition of the muscles it innervates, and the degree to which lost sensitivity is restored.
Differential Diagnosis of Neuropathic Symptoms
Symptoms of neuropathy and neuralgia can overlap with various other conditions, requiring careful differential diagnosis:
| Presenting Symptom Complex | Neuropathic Conditions to Consider | Other Non-Neuropathic Differentials |
|---|---|---|
| Distal, symmetrical numbness, tingling, pain, weakness ("stocking-glove") | Polyneuropathy (diabetic, alcoholic, toxic, nutritional, inflammatory, hereditary) | Vascular insufficiency (peripheral artery disease), severe vitamin deficiencies with systemic effects, some myelopathies. |
| Localized nerve pain (sharp, shooting, burning) in a specific nerve distribution | Mononeuropathy (e.g., carpal tunnel syndrome, peroneal neuropathy), Neuralgia (trigeminal, occipital, intercostal, postherpetic) | Musculoskeletal pain (tendinitis, bursitis, myofascial pain), localized arthritis, vascular pain (e.g., claudication if activity-related), referred pain from visceral organs. |
| Focal weakness in specific muscles | Mononeuropathy, Mononeuritis multiplex, Motor neuron disease (early stages) | Myopathy, neuromuscular junction disorder (e.g., myasthenia gravis), orthopedic injury (tendon rupture, joint instability), stroke (central weakness pattern). |
| Sensory loss in a dermatomal pattern with or without radicular pain | Radiculopathy (nerve root compression, e.g., from herniated disc, spinal stenosis) | Peripheral nerve entrapment mimicking radicular pattern (less common), referred pain. |
| Autonomic dysfunction (postural dizziness, sweating changes, GI/bladder issues) | Autonomic neuropathy (can be part of polyneuropathy like diabetic or alcoholic, or isolated) | Primary cardiovascular conditions, medication side effects, primary gastrointestinal or urological disorders. |
Prognosis and Potential Complications
The prognosis for neuropathies and neuralgias is highly variable:
- Depends on the underlying cause, severity of nerve damage (axonal vs. demyelinating), duration of symptoms before treatment, and overall health of the patient.
- Acute inflammatory or compressive neuropathies treated promptly may have good recovery.
- Chronic, progressive polyneuropathies (e.g., advanced diabetic neuropathy, some hereditary forms) may lead to irreversible deficits.
Potential complications include:
- Chronic pain and impaired quality of life.
- Permanent sensory loss, leading to increased risk of injury (burns, pressure sores).
- Muscle atrophy, weakness, and disability (e.g., foot drop, hand weakness).
- Joint contractures and deformities.
- Development of trophic ulcers.
- Impact on mental health (anxiety, depression).
Prevention Strategies
Preventive measures depend on the specific type of neuropathy/neuralgia:
- Diabetes: Strict glycemic control, regular foot care.
- Alcohol: Moderation or abstinence.
- Toxins/Medications: Avoiding exposure to known neurotoxins; careful monitoring with potentially neurotoxic drugs.
- Trauma: Using protective gear, safe practices to avoid injuries.
- Nutritional Deficiencies: Maintaining a balanced diet.
- Repetitive Strain: Ergonomic adjustments, regular breaks for occupational risks.
- Infections: Vaccination (e.g., shingles vaccine for older adults).
When to Consult a Specialist (Neurologist, Neurosurgeon, Pain Specialist)
Consultation with a relevant specialist is crucial if an individual experiences:
- Persistent or progressive numbness, tingling, weakness, or pain in the limbs or face.
- Symptoms suggestive of neuralgia (sharp, shooting, or burning nerve pain).
- Muscle wasting or unexplained changes in skin, hair, or nails in an affected area.
- Difficulty with balance, coordination, or walking.
- Symptoms that interfere significantly with daily activities or quality of life.
- Known risk factors for neuropathy (e.g., diabetes, chemotherapy, trauma) and development of new neurological symptoms.
A neurologist can conduct a comprehensive evaluation, including electrodiagnostic tests, to diagnose the type and cause of neuropathy or neuralgia and recommend an appropriate management plan. A neurosurgeon may be involved if surgical intervention is needed for nerve compression or trauma. A pain management specialist can help with complex or refractory neuralgic pain.
References
- Barohn RJ, Amato AA. Peripheral neuropathy. Continuum (Minneap Minn). 2013 Feb;19(1 Peripheral Nervous System Disorders):86-108.
- England JD, Gronseth GS, Franklin G, et al. Practice Parameter: Evaluation of distal symmetric polyneuropathy: Role of laboratory and genetic testing (an evidence-based review). Report of the American Academy of Neurology, American Association of Neuromuscular and Electrodiagnostic Medicine, and American Academy of Physical Medicine and Rehabilitation. Neurology. 2009 Jan 13;72(2):185-92.
- Dyck PJ, Thomas PK. Peripheral Neuropathy. 4th ed. Elsevier Saunders; 2005. (Comprehensive reference)
- Preston DC, Shapiro BE. Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic Correlations. 3rd ed. Elsevier Saunders; 2013.
- Callaghan BC, Price RS, Feldman EL. Distal Symmetric Polyneuropathy: A Review. JAMA. 2015 Nov 24;314(20):2172-81.
- Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010 Sep;17(9):1113-e88.
- Cruccu G, Sommer C, Anand P, et al. EFNS guidelines on neuropathic pain assessment: revised 2009. Eur J Neurol. 2010 Aug;17(8):1010-8.
- Said G. Inflammatory neuropathies. Rev Neurol (Paris). 2007 Apr;163(4):409-20.
See also
- Anatomy of the nervous system
- Spinal disc herniation
- Pain in the arm and neck (trauma, cervical radiculopathy)
- The eyeball and the visual pathway:
- Anatomy of the eye and physiology of vision
- The visual pathway and its disorders
- Eye structures and visual disturbances that occur when they are affected
- Retina and optic disc, visual impairment when they are affected
- Impaired movement of the eyeballs
- Nystagmus and conditions resembling nystagmus
- Dry Eye Syndrome
- Optic nerve and retina:
- Compression neuropathy of the optic nerve
- Edema of the optic disc (papilledema)
- Ischemic neuropathy of the optic nerve
- Meningioma of the optic nerve sheath
- Optic nerve atrophy
- Optic neuritis in adults
- Optic neuritis in children
- Opto-chiasmal arachnoiditis
- Pseudo-edema of the optic disc (pseudopapilledema)
- Toxic and nutritional optic neuropathy
- Neuropathies and neuralgia:
- Diabetic, alcoholic, toxic and small fiber sensory neuropathy (SFSN)
- Facial nerve neuritis (Bell's palsy, post-traumatic neuropathy)
- Fibular (peroneal) nerve neuropathy
- Median nerve neuropathy
- Neuralgia (intercostal, occipital, facial, glossopharyngeal, trigeminal, metatarsal)
- Post-traumatic neuropathies
- Post-traumatic trigeminal neuropathy
- Post-traumatic sciatic nerve neuropathy
- Radial nerve neuropathy
- Tibial nerve neuropathy
- Trigeminal neuralgia
- Ulnar nerve neuropathy
- Tumors (neoplasms) of the peripheral nerves and autonomic nervous system (neuroma, sarcomatosis, melanoma, neurofibromatosis, Recklinghausen's disease)
- Carpal tunnel syndrome
- Ulnar nerve compression in the cubital canal