Radial nerve neuropathy
- Understanding Radial Nerve Neuropathy
- Symptoms and Clinical Presentation of Radial Nerve Neuropathy
- Diagnosis of Radial Nerve Neuropathy
- Treatment of Radial Nerve Neuropathy
- Differential Diagnosis of Wrist/Finger Extensor Weakness
- Prognosis and Potential Complications
- Prevention Strategies
- When to Consult a Specialist (Neurologist, Hand Surgeon)
- References
Understanding Radial Nerve Neuropathy
Radial nerve neuropathy refers to damage or dysfunction of the radial nerve (nervus radialis), a major peripheral nerve of the upper limb. This condition can result in characteristic motor and sensory deficits, most notably wrist drop and weakness of finger/thumb extension, along with sensory changes on the back of the hand and forearm.
Anatomy and Function of the Radial Nerve
The radial nerve is a mixed nerve, meaning it carries both motor fibers (for muscle movement) and sensory fibers (for sensation). It is primarily formed from nerve fibers originating from the C5, C6, C7, C8, and T1 spinal nerve roots. These fibers initially pass through the middle trunk and then predominantly form the posterior cord of the brachial plexus, from which the radial nerve arises.
The radial nerve courses from the axilla, winds around the humerus in the spiral groove (radial groove), passes across the lateral epicondyle of the humerus, and then divides into superficial (sensory) and deep (motor - posterior interosseous nerve, PIN) branches in the forearm.
Key functions innervated by the radial nerve and its branches include:
- Motor Functions:
- Extension of the elbow (triceps brachii muscle).
- Supination of the forearm (supinator muscle, brachioradialis assists). The term "instep support of the forearm" in the original text likely refers to supination or the role of brachioradialis in stabilizing/flexing the elbow.
- Extension of the wrist (wrist extensors like extensor carpi radialis longus/brevis, extensor carpi ulnaris).
- Extension of the fingers at the metacarpophalangeal (MCP) joints (extensor digitorum, extensor indicis, extensor digiti minimi).
- Extension and abduction of the thumb (extensor pollicis longus/brevis, abductor pollicis longus).
- The brachioradialis muscle, innervated by the radial nerve before its division, also contributes to elbow flexion, especially in a mid-prone position.
- Sensory Functions: The sensory fibers of the radial nerve innervate the skin of:
- The posterior surface of the upper arm (shoulder region).
- The posterior surface of the forearm.
- The lateral aspect of the dorsum (back) of the hand.
- Partially, the dorsal aspect of the thumb (I), index finger (II), and sometimes the middle finger (III), typically up to the distal interphalangeal joints.
Common Causes and Sites of Injury
Damage to the radial nerve can occur as a result of various mechanisms, leading to inflammatory changes (neuritis) and impaired motor and sensory function in its area of innervation on the arm. Common causes include:
- Trauma:
- Fractures of the Humerus: Especially mid-shaft fractures involving the spiral groove, where the nerve is in close proximity to the bone. This is a very common cause.
- Dislocations of the shoulder or elbow joints.
- Direct blows or penetrating injuries to the arm or axilla.
- Post-injection injury if a drug is inadvertently injected into or near the nerve.
- Compression:
- "Saturday Night Palsy": Prolonged compression of the nerve in the axilla or against the humerus, often from sleeping with the arm draped over a chair or in an awkward position, especially with alcohol intoxication.
- Crutch Palsy: Improper use of crutches causing pressure in the axilla.
- Prolonged clamping or pressure during surgery or prolonged immobility.
- Tight bands, tourniquets, or handcuffs.
- Entrapment at specific anatomical sites (e.g., radial tunnel syndrome, posterior interosseous nerve syndrome at the arcade of Frohse).
- Inflammatory/Infectious Conditions: Though less common as a primary cause of isolated radial neuropathy, systemic inflammatory conditions or local infections could theoretically involve the nerve.
- Tumors or Cysts: Pressing on the nerve.
- Iatrogenic Injury: During surgical procedures in the arm or shoulder region.
Symptoms and Clinical Presentation of Radial Nerve Neuropathy
The clinical manifestations of radial nerve neuropathy depend on the level and severity of the nerve lesion.
Impact of Lesion Level on Symptoms
- High Lesion (Axillary Fossa / Upper Arm, proximal to triceps branches):
- Paralysis of elbow extension (triceps weakness).
- Weakness of forearm flexion (brachioradialis involvement).
- Complete wrist drop (paralysis of all wrist extensors).
- Finger drop (paralysis of finger extensors at MCP joints).
- Thumb drop (paralysis of thumb extensors and abductor pollicis longus).
- Weakness of forearm supination.
- Loss of triceps tendon reflex. Carporadial (brachioradialis) reflex may also be weakened or absent.
- Sensory loss on the posterior aspect of the arm, forearm, and the characteristic radial-innervated area of the dorsal hand and fingers.
- Lesion at the Spiral Groove of Humerus (Middle Third of Upper Arm): This is a very common site of injury (e.g., "Saturday night palsy," humerus fracture).
- Triceps function (elbow extension) is usually spared because branches to the triceps arise proximal to the spiral groove.
- Brachioradialis function (elbow flexion in mid-prone) may be weakened or spared depending on the exact level.
- Characteristic wrist drop, finger drop, and thumb drop are present.
- Weakness of supination.
- Triceps reflex is preserved; brachioradialis reflex may be diminished or absent.
- Sensory loss is typically on the posterior forearm and dorsal hand/fingers; sensation on the posterior arm is usually spared.
- Lesion in the Lower Third of the Upper Arm (distal to triceps and brachioradialis branches):
- Elbow extension (triceps) and elbow flexion (brachioradialis) are preserved.
- Wrist drop, finger drop, and thumb drop are present.
- Sensory loss on the posterior forearm and dorsal hand/fingers may be present.
- Lesion in the Forearm (affecting Posterior Interosseous Nerve - PIN): The PIN is a purely motor branch.
- Wrist extension is often partially spared (due to extensor carpi radialis longus, which is innervated by the radial nerve proper before PIN branches off), but ulnar deviation may occur during wrist extension due to weakness of extensor carpi radialis brevis and extensor carpi ulnaris.
- Significant finger drop (MCP joint extension weakness) and thumb extension weakness are characteristic.
- No sensory loss, as the PIN is motor. Pain may be present at the site of entrapment (e.g., radial tunnel).
- Lesion of Superficial Radial Nerve (Sensory Branch):
- Causes isolated sensory loss or paresthesias on the radial aspect of the dorsal hand, dorsal thumb, index, and middle fingers (up to DIP joints). No motor weakness. This can occur from tight wristbands, handcuffs ("cheiralgia paresthetica"), or local trauma.
It's important to note that the zone of complete sensory loss (anesthesia) on the hand is often smaller than the anatomical distribution due to significant overlap in innervation from neighboring nerves (median and ulnar). Joint-muscular sense (proprioception) is generally not affected by isolated radial nerve lesions.
With lesions of the **C7 spinal nerve root** or the **middle trunk of the brachial plexus**, the main extensor functions typically supplied by the radial nerve are lost. This often occurs in combination with partial damage to the median nerve (specifically its upper root/leg originating from C7 via the lateral cord), leading to associated weakness in forearm pronation and wrist/finger flexion.
With damage to the **posterior cord of the brachial plexus** (from which the radial and axillary nerves arise), the same primary functions of the radial nerve are lost, but this occurs in combination with damage to the axillary nerve (causing deltoid weakness and sensory loss over the lateral shoulder).
Motor Deficits (Wrist Drop, Finger Drop)
The most characteristic motor sign of significant radial nerve neuropathy is **wrist drop**, where the patient is unable to extend the wrist against gravity. This is often accompanied by **finger drop** (inability to extend the fingers at the MCP joints) and **thumb drop** (inability to extend and abduct the thumb). Weakness of forearm supination may also be present.
Sensory Disturbances
Sensory loss or paresthesias typically occur in the distribution of the superficial radial nerve: the posterior aspect of the arm (if lesion is high), posterior forearm, dorsolateral aspect of the hand, and dorsal surfaces of the thumb, index, middle, and sometimes the radial half of the ring finger, usually sparing the fingertips (which are supplied by the median and ulnar nerves).
Specific Clinical Tests
Among the numerous clinical tests described to determine movement disorders with radial nerve damage, key findings include:
- Inability to extend the wrist and fingers:** The classic "wrist drop" and "finger drop."
- Inability to extend and abduct the thumb ("hitchhiker's sign").
- Test for Finger Extension: When asked to place palms together with fingers straightened and then attempt to separate the hands while keeping fingers extended, the fingers on the affected hand are not actively extended (retracted) but rather flex passively and "slide" along the palm of the healthy, extended hand.
- Weakness of grip (due to lack of synergistic wrist extension).
Diagnosis of Radial Nerve Neuropathy
Diagnosis involves a comprehensive clinical evaluation, often supported by electrodiagnostic studies and sometimes imaging.
Clinical Examination
As detailed above, this includes a thorough motor and sensory examination of the upper limb, reflex testing (triceps, brachioradialis), and careful assessment for Tinel's sign along the course of the nerve, especially at common entrapment sites (e.g., spiral groove, radial tunnel).
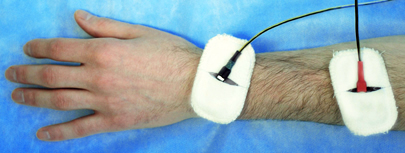
Electrodiagnostic Studies (EMG/NCS)
Electromyography (EMG) and Nerve Conduction Studies (NCS/ENG) are invaluable for:
- Confirming radial neuropathy and localizing the site of the lesion (e.g., axilla, spiral groove, radial tunnel, PIN lesion).
- Differentiating from brachial plexopathy or cervical radiculopathy (e.g., C7).
- Determining the type of nerve injury (axonal loss vs. demyelination/conduction block).
- Assessing severity and providing prognostic information.
Imaging Studies
- X-rays: To identify fractures of the humerus or other bony abnormalities.
- Ultrasound: High-resolution ultrasound can visualize the radial nerve, detect focal swelling, compression, or discontinuity.
- MRI: May be used to evaluate for soft tissue masses, tumors compressing the nerve, or to assess inflammation or denervation changes in muscles if the diagnosis is unclear or a more proximal lesion is suspected.
Treatment of Radial Nerve Neuropathy
Treatment for radial nerve neuritis or neuropathy is selected individually for each case, depending on the cause, severity, and duration of symptoms. It often includes a combination of conservative procedures, and in some instances, surgical intervention.
Conservative Management
This is the initial approach for many radial neuropathies, especially compressive types like "Saturday night palsy" or mild traumatic injuries.
- Observation: Many traumatic radial neuropathies (especially neurapraxia or mild axonotmesis due to compression or closed fracture) recover spontaneously over weeks to months.
- Wrist Splinting: A dynamic wrist/finger extension splint (cock-up splint) is crucial to support the wrist in a functional position, prevent wrist drop contracture, and improve hand function during recovery.
- Physical Therapy:
- Passive and active range-of-motion exercises for the wrist, fingers, and thumb to prevent stiffness and contractures.
- Strengthening exercises for weakened extensor muscles as reinnervation occurs.
- Activity Modification: Avoiding activities or postures that compress or irritate the nerve.
Pharmacological Treatment
- Pain Management: For neuropathic pain, medications such as gabapentin, pregabalin, or tricyclic antidepressants may be used. NSAIDs can help with inflammatory pain.
- Vitamins: B-complex vitamins (B1, B6, B12), Vitamin C, and Vitamin E are often prescribed as supportive therapy for nerve health.
- Corticosteroids: A short course of oral corticosteroids may be considered in some acute inflammatory or compressive neuropathies to reduce swelling, but their role in direct traumatic radial neuropathy is not definitively established.
Rehabilitative Therapies
- Acupuncture: May be used for pain relief and to potentially promote nerve recovery.
- Nerve Stimulation and Muscle Stimulation:
- Transcutaneous Electrical Nerve Stimulation (TENS) for pain control.
- Neuromuscular Electrical Stimulation (NMES) to help maintain muscle mass and prevent disuse atrophy in denervated extensor muscles while awaiting reinnervation.
- Homeopathic Remedies: Some individuals may choose to explore homeopathic treatments, though their efficacy is not supported by mainstream scientific evidence.
Surgical Intervention
Surgical treatment is considered in specific situations:
- Open Injuries: Lacerations or penetrating trauma with known or suspected nerve transection require early surgical exploration and repair (neurorrhaphy).
- Failure of Spontaneous Recovery: For closed injuries (e.g., associated with humerus fracture or prolonged compression), if there are no clinical or electrophysiological signs of recovery after an appropriate observation period (typically 3-6 months), surgical exploration may be indicated.
- Persistent Compression: If a clear compressive lesion is identified (e.g., tumor, scar tissue from fracture callus, fibrous bands in radial tunnel) that does not resolve with conservative measures.
- Progressive Neurological Deficit.
Surgical procedures may include:
- Neurolysis: Freeing the nerve from external compression or scar tissue.
- Nerve Repair (Neurorrhaphy): Direct end-to-end suturing of a transected nerve.
- Nerve Grafting: If a segment of the nerve is damaged beyond repair, a nerve graft (often using the sural nerve) is used to bridge the defect.
- Tendon Transfers: For permanent wrist/finger drop with no prospect of nerve recovery, tendon transfer procedures (e.g., transferring flexor tendons to act as extensors) can restore some active extension and improve hand function.
Differential Diagnosis of Wrist/Finger Extensor Weakness
Wrist drop and finger extensor weakness, the hallmark of radial neuropathy, must be differentiated from other conditions:
| Condition | Key Differentiating Features |
|---|---|
| Radial Nerve Neuropathy | Weakness of wrist/finger/thumb extensors, supinator, brachioradialis (depending on level). Sensory loss in radial nerve distribution. Triceps reflex may be affected with high lesions. Specific site of compression/injury often identifiable. |
| C7 Radiculopathy | Weakness can involve triceps, wrist extensors, and finger extensors (overlapping with radial nerve). Often associated with neck pain, radiating arm pain in C7 dermatome. Other C7-innervated muscles (e.g., pronators, wrist flexors - partially) may be weak. Triceps reflex often diminished/absent. |
| Brachial Plexopathy (Posterior Cord or Upper/Middle Trunk) | More widespread weakness involving other nerves arising from posterior cord (axillary, thoracodorsal, subscapular) or trunks. Sensory loss may be more extensive. |
| Central Causes (Stroke, Brain Lesion - very rare for isolated wrist drop) | Usually associated with upper motor neuron signs (spasticity, hyperreflexia, Babinski sign), other neurological deficits (hemiparesis, aphasia). Pattern of weakness often different (e.g., entire arm affected, not just extensors). |
| Lead Neuropathy (Plumbism) | Classically causes bilateral wrist drop and finger extensor weakness (motor predominant). History of lead exposure. Other systemic signs of lead poisoning. |
| Myopathy (e.g., Facioscapulohumeral Dystrophy - FSHD, Inclusion Body Myositis - IBM) | Muscle weakness is primary; FSHD can have scapular winging, facial weakness. IBM often asymmetrical, can affect finger flexors more than extensors initially. EMG shows myopathic changes. Sensory exam usually normal. |
| Tendon Rupture or Enthesopathy (e.g., Lateral Epicondylitis - "Tennis Elbow") | Pain at lateral epicondyle with resisted wrist extension (tennis elbow). Rupture of extensor tendons causes inability to extend specific digits/wrist, often after trauma or chronic tendinopathy. No primary sensory loss. |
Prognosis and Potential Complications
The prognosis for radial nerve neuropathy is generally good, especially for compressive neuropathies (like "Saturday night palsy") where the cause is transient and there is primarily neurapraxia (conduction block without axonal death).
- Neurapraxia: Full recovery is expected, usually within weeks to a few months, once the compression is removed.
- Axonotmesis (axonal damage, nerve sheath intact): Recovery depends on axonal regeneration (approx. 1 mm/day or 1 inch/month). It can be slow and may be incomplete, especially for more proximal lesions or severe axonal loss.
- Neurotmesis (complete nerve transection or severe disruption): Spontaneous recovery is unlikely without surgical repair. Prognosis even with surgery is variable.
Potential complications include:
- Persistent weakness (wrist/finger drop).
- Chronic pain or paresthesias.
- Muscle atrophy.
- Joint contractures (e.g., wrist flexion contracture).
- Functional impairment of the hand.
Prevention Strategies
Measures to prevent radial nerve neuropathy include:
- Avoiding prolonged pressure on the axilla or spiral groove of the humerus (e.g., not sleeping with arm draped over hard surfaces, proper crutch use).
- Careful positioning during surgery or prolonged immobilization.
- Prompt and appropriate management of humerus fractures.
- Awareness of activities or postures that might compress the nerve.
When to Consult a Specialist (Neurologist, Hand Surgeon)
Medical evaluation by a neurologist, hand surgeon, or physician specializing in peripheral nerve injuries is recommended if an individual experiences:
- Sudden or gradual onset of wrist drop, finger drop, or thumb weakness.
- Numbness or tingling on the back of the hand or forearm in the radial nerve distribution.
- Symptoms following a trauma to the arm or shoulder.
- Weakness or sensory changes that do not improve or worsen over time.
Early diagnosis, identification of the cause, and appropriate management are crucial for maximizing the chances of recovery from radial nerve neuropathy.
References
- Stewart JD. Focal Peripheral Neuropathies. 3rd ed. Lippincott Williams & Wilkins; 2000. Chapter 8: Radial Neuropathy.
- Preston DC, Shapiro BE. Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic Correlations. 3rd ed. Elsevier Saunders; 2013. Chapter 19: Radial Neuropathy.
- Spinner RJ, Poliakoff MB, Tiel RL. The origin of the anconeus muscle and its relationship to the J Laryngol Otol. 2001;115(1):38-41. (Anatomical context)
- Latef TJ, Bilal M, Kundi M, et al. Radial Nerve Palsy: A Review. Cureus. 2018 Feb 27;10(2):e2238.
- Bumbasirevic M, Lesic A, Bumbasirevic V, et al. Radial nerve palsy. EFORT Open Rev. 2016 Aug 10;1(8):286-294.
- DeFranco MJ, Lawton JN. Radial nerve injuries associated with humeral fractures. J Hand Surg Am. 2006 Jan;31(1):152-6.
- Mansukhani KA. Electrodiagnosis in traumatic radial nerve injuries. Neurol India. 2000 Dec;48(4):329-34.
- Kim DH, Kline DG. Management and results of extensive traumatic longitudinal nerve injuries including the brachial plexus and lumbosacral plexus. Neurosurgery. 2004 Jul;55(1):136-46; discussion 146-7.
See also
- Anatomy of the nervous system
- Spinal disc herniation
- Pain in the arm and neck (trauma, cervical radiculopathy)
- The eyeball and the visual pathway:
- Anatomy of the eye and physiology of vision
- The visual pathway and its disorders
- Eye structures and visual disturbances that occur when they are affected
- Retina and optic disc, visual impairment when they are affected
- Impaired movement of the eyeballs
- Nystagmus and conditions resembling nystagmus
- Dry Eye Syndrome
- Optic nerve and retina:
- Compression neuropathy of the optic nerve
- Edema of the optic disc (papilledema)
- Ischemic neuropathy of the optic nerve
- Meningioma of the optic nerve sheath
- Optic nerve atrophy
- Optic neuritis in adults
- Optic neuritis in children
- Opto-chiasmal arachnoiditis
- Pseudo-edema of the optic disc (pseudopapilledema)
- Toxic and nutritional optic neuropathy
- Neuropathies and neuralgia:
- Diabetic, alcoholic, toxic and small fiber sensory neuropathy (SFSN)
- Facial nerve neuritis (Bell's palsy, post-traumatic neuropathy)
- Fibular (peroneal) nerve neuropathy
- Median nerve neuropathy
- Neuralgia (intercostal, occipital, facial, glossopharyngeal, trigeminal, metatarsal)
- Post-traumatic neuropathies
- Post-traumatic trigeminal neuropathy
- Post-traumatic sciatic nerve neuropathy
- Radial nerve neuropathy
- Tibial nerve neuropathy
- Trigeminal neuralgia
- Ulnar nerve neuropathy
- Tumors (neoplasms) of the peripheral nerves and autonomic nervous system (neuroma, sarcomatosis, melanoma, neurofibromatosis, Recklinghausen's disease)
- Carpal tunnel syndrome
- Ulnar nerve compression in the cubital canal