Anatomy of the eye and physiology of vision
The Eye: A Window to Vascular and Nervous Tissue
The human eye is a remarkable organ of vision, uniquely structured to capture and process light. For medical professionals, particularly neurologists, neurosurgeons, and ophthalmologists, the eye holds special significance. During an eye examination, it is possible to directly observe vascular (blood vessels) and nervous tissue (the optic nerve head and retina) of the examined individual. The eye is the only organ in the body that allows a physician to visualize nerves and blood vessels in their natural state without performing any preliminary incisions or punctures of healthy tissues.
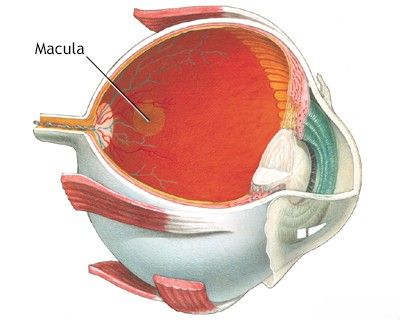
Anatomy of the Eyeball and Retina
The eyeball is intricately designed to focus light onto a highly sensitive neuronal membrane – the retina. Light entering the eyeball first passes through several transparent refractive media:
- Cornea: The clear outer front surface that covers the iris and pupil, responsible for most of the eye's focusing power.
- Aqueous Humor: The clear, watery fluid in the anterior and posterior chambers of the eye (between the cornea and the lens).
- Lens: A transparent, biconvex structure located behind the iris and pupil, which fine-tunes focus by changing its shape (accommodation).
- Vitreous Humor: The clear, gel-like substance that fills the space between the lens and the retina, maintaining the eyeball's shape.
After traversing these media, light crosses the transparent inner layers of the retina to reach the photoreceptor cells (rods and cones) located in the outer nuclear layer of the retina.
The amount of light entering the eye and falling on the retina is regulated by the iris, a pigmented muscular diaphragm. The central opening in the iris is the pupil. Specialized muscles within the iris (sphincter and dilator pupillae) control the pupil's diameter, allowing it to constrict (narrow) in bright light or dilate (widen) in dim light, thereby controlling the light influx required to produce a clear image on the retina.
Photoreceptors: Rods and Cones
Light that reaches the retina is captured by photoreceptor cells in the fundus (the back part of the eye visible through an ophthalmoscope). These specialized nerve cells are of two types: rods and cones, each containing visual pigments that absorb photons (light particles).
- Rods: These photoreceptors are highly sensitive and responsible for vision in low-light conditions (scotopic vision). They detect shades of gray and are not involved in color perception. Rods are more numerous than cones in the human retina (approximately 100-120 million rods). They are absent in the very center of the fovea (the dimple) but their concentration peaks at about 20° eccentricity from the fovea, gradually decreasing towards the retinal periphery.
- Cones: These photoreceptors respond to light of greater intensity and are responsible for sharp, detailed central vision (photopic vision) and color perception. There are three types of cones, each sensitive to different wavelengths of light (red, green, and blue), enabling color vision. Cones are abundantly located in the center of the retina, particularly in the macula lutea (yellow spot). The macula contains a central depression called the fovea centralis, and within it, a smaller, even more specialized dimple, the foveola. The fovea is located approximately 3-4 mm temporal (towards the temple) from the edge of the optic nerve head (optic disc). This foveal region is where the highest visual acuity (sharpness of vision, normally 20/20 or 6/6) is achieved. Visual acuity drops sharply in the paramacular zone (areas surrounding the macula) where the density of cones decreases significantly. There are approximately 6-7 million cones in the human retina.
The absorption of light by visual pigments triggers a cascade of photochemical reactions within the rods and cones, leading to physiological responses of nervous excitation and inhibition at complex synaptic levels involving other retinal cells (bipolar cells, horizontal cells, amacrine cells, and ganglion cells). This intricate processing within the retina allows for the evaluation of various properties of incoming light, including spatial details, light intensity, spectral composition (color), and temporal changes.
Visual Pathway to the Brain
The distribution of ganglion cells (the output neurons of the retina) mirrors that of the cones, being most concentrated in the macular region. In the fovea, there is often a one-to-one connection where a single ganglion cell receives input (via a bipolar neuron) from a single cone. This 1:1 ratio maximizes visual resolution and acuity. In peripheral retinal areas, multiple photoreceptors converge onto single ganglion cells, increasing light sensitivity but reducing resolution.
Primary processing of visual information occurs within the complex layers of the retina. The processed information is then transmitted in the form of electrical impulses (action potentials) from the ganglion cells along their axons. These axons converge to form the optic nerve (cranial nerve II), which exits the eyeball at the optic disc (blind spot). The optic nerves from both eyes partially decussate (cross over) at the optic chiasm. Fibers continue as the optic tracts to the lateral geniculate nucleus (LGN) of the thalamus in the brain. After synaptic switching in the LGN, the visual information travels along the geniculocalcarine tract (optic radiations) to the primary visual cortex located in the occipital lobe of the brain, where conscious perception of vision occurs.
Physiology of Vision: Types and Assessment
Human vision is a multifaceted sense, encompassing several distinct perceptual abilities. Clinically, it is often divided into form vision (visual acuity), color vision, and light perception (including visual fields).
Form Vision and Visual Acuity Assessment
Form vision refers to the ability to distinguish shapes and details of objects. In clinical practice, it is primarily assessed by determining visual acuity, which measures the resolving power of the eye. This should be a part of any complete medical or neurological examination, regardless of whether the patient has specific visual complaints.
Standardized charts are used for this assessment:
- Snellen Chart (1862): This chart, consisting of rows of letters (optotypes) of decreasing size, is typically placed at a distance of 6 meters (or 20 feet) from the patient. Each row corresponds to a specific visual acuity level.
- Sivtsev Table: Used in some regions (e.g., historically in the USSR), this table is located at a distance of 5 meters from the patient and serves a similar purpose.
The Snellen chart has letters of various sizes, and next to each row is an indication of the distance at which a person with normal vision should be able to read that line (e.g., the "20/20" line letters subtend an angle of 5 minutes of arc at 20 feet, with individual strokes subtending 1 minute of arc). A patient with corrected refractive errors (e.g., myopia, hyperopia, astigmatism) should wear their prescribed glasses or contact lenses during the examination.
Visual acuity is expressed as a fraction (e.g., 20/20, 6/6). The numerator indicates the testing distance, and the denominator indicates the distance at which a person with normal vision can read the smallest line of letters identified by the patient. For example:
- Normal vision is typically 20/20 (US) or 6/6 (metric).
- If a patient can only read letters down to the line marked "20/30," their visual acuity is recorded as 20/30 (meaning they can see at 20 feet what a person with normal vision can see at 30 feet).
- If the patient is unable to distinguish the largest letter E on the top line (e.g., the 20/200 or 20/400 line), they must be moved closer to the chart, and the distance is noted (e.g., "visual acuity is 10/400" if the patient can distinguish the 20/400 letter at a distance of 10 feet or 3 meters from the chart).
- If vision is poorer still, acuity may be recorded as "counts fingers (CF) at x feet," "hand motion (HM) at x feet," "light perception (LP)," or "no light perception (NLP)."
If a patient cannot read, for example, the 20/30 line, pinhole acuity (stenopic vision) should be examined. The patient views the chart through a small pinhole aperture. This device effectively reduces the impact of refractive errors by allowing only central light rays to enter the eye, thus creating a sharper image on the retina. If pinhole testing improves visual acuity significantly (e.g., to 20/20), it suggests that the reduced vision is primarily due to an uncorrected or undercorrected refractive error. If the pinhole does not improve visual acuity, another cause for the decreased vision should be sought, such as clouding of the ocular media (e.g., corneal opacity, cataract, vitreous hemorrhage), macular disease, or damage to the optic nerve or visual pathways.
Visual acuity corrected by glasses or contact lenses to 20/200 or less in the better eye, or a concentric narrowing of visual fields to 20 degrees or less (not 10° as mentioned in the original text, though definitions can vary slightly by jurisdiction) is often considered legal blindness in many regions, including the United States. Such a patient would typically be registered with relevant societies or agencies for the blind.
Color Vision and its Impairments
Color vision is mediated by the three types of cone photoreceptors in the retina. Impairments in human vision are often characterized by acquired or congenital defects in color perception.
- Acquired Color Vision Defects: These can occur due to various ocular or systemic conditions. For example, in some cases of macular lesions (due to drug intoxication, degenerative causes like age-related macular degeneration, or hereditary dystrophies) or optic nerve diseases (such as optic neuritis in multiple sclerosis, toxic optic neuropathy from substances like methanol or ethambutol, nutritional optic neuropathy, or tobacco-alcohol amblyopia), patients may experience difficulty distinguishing between red and green colors (dyschromatopsia), even though their perception of white color (and often visual acuity for black and white) might remain relatively normal initially. Blue-yellow color vision defects can also occur, for instance, in some forms of optic neuropathy or glaucoma.
- Hereditary Color Vision Defects (Color Blindness): These are typically X-linked recessive conditions, more common in males. The most common types are red-green color deficiencies (protanopia/protanomaly for red, deuteranopia/deuteranomaly for green). Blue color deficiency (tritanopia/tritanomaly) is rarer. Complete color blindness (achromatopsia) is very rare.
For the clinical study of color vision, various tests are used:
- Ishihara Polychromatic Plates: Most commonly used for screening red-green color vision defects. These plates consist of dots of various colors and sizes, arranged to form numbers or patterns visible to those with normal color vision but difficult or impossible for color-deficient individuals to discern.
- Hardy-Rand-Rittler (HRR) Pseudoisochromatic Plates: These can identify defects in red-green as well as blue-yellow color perception.
- Farnsworth D-15 Test or Farnsworth-Munsell 100 Hue Test: More sophisticated arrangement tests used for classifying the type and severity of color vision defects.
Normal color vision is essential for certain occupations and daily tasks.
Light Perception and Visual Field Studies (Perimetry)
Light perception involves the ability to detect light and differentiate varying intensities. A person's overall field of vision (the entire area visible when the eye is fixed in one position) is assessed by examining the visual fields. The procedure for mapping the visual fields is called perimetry. Changes or defects in the visual fields (e.g., scotomas - blind spots, hemianopias - loss of half the visual field) indicate damage to a portion of the visual pathway, from the retina, along the optic nerve, optic chiasm, optic tracts, optic radiations, to the visual cortex in the occipital lobe.
Methods for visual field testing include:
- Confrontation Visual Field Testing: A simple screening test where the examiner compares their own visual field with the patient's by having the patient fixate on the examiner's nose and detect fingers or objects brought in from the periphery.
- Kinetic Perimetry (e.g., Goldmann Hemispheric Perimeter): This method is convenient for studying the overall extent of visual fields. It involves moving a test object of a specific size and brightness from the periphery towards the center of fixation. The patient signals when they first see the object. By testing multiple meridians, an isopter (a line connecting points of equal retinal sensitivity for that specific target) is plotted, outlining the visual field.
- Static Perimetry (e.g., Humphrey Field Analyzer, Octopus Perimeter): This automated method presents light stimuli of varying intensities at fixed locations within the visual field. The patient presses a button when they see a light. This provides a more detailed and quantitative map of retinal sensitivity, useful for detecting and monitoring subtle defects, particularly in glaucoma or neurological conditions.
During perimetry, the patient gives a signal when they see a test object, indicates when it disappears (if testing for scotomas), and when it then reappears. In this way, a diagram of the patient's visual fields can be drawn up, accurately indicating defects from the periphery to the central fixation point. It's also possible to compare the patient's peripheral visual fields with those of the examiner during confrontation testing.
Normal monocular visual fields, when tested with a standard target during perimetry, typically extend approximately:
- Temporally (side of the temple): 90-100° from fixation
- Nasally (side of the nose): 60° from fixation
- Superiorly (upwards): 60° from fixation
- Inferiorly (downwards): 70-75° from fixation
(Note: The original text values of 50° nasally/up and 65° down are slightly more restricted than commonly cited averages, but field extent can vary with target size, brightness, and individual factors like facial anatomy.)
Causes of Visual Impairment
The listed visual impairments (reduced acuity, color defects, field loss) in patients can occur either individually or in various combinations. Such impairments can result from a wide range of pathologies affecting different parts of the visual system:
- Refractive Errors: Changes in the refractive (light-bending) properties of the transparent media of the eye (cornea, lens). Examples include myopia (nearsightedness), hyperopia (farsightedness), astigmatism, and presbyopia (age-related loss of accommodation).
- Opacities of Ocular Media:
- Corneal diseases (scars, dystrophies, edema, keratitis).
- Cataracts (clouding of the lens).
- Vitreous opacities (hemorrhage, inflammation, floaters).
- Retinal Diseases:
- Macular degeneration (age-related or other forms).
- Diabetic retinopathy.
- Retinal detachment.
- Retinal vascular occlusions (artery or vein).
- Inherited retinal dystrophies (e.g., retinitis pigmentosa).
- Retinal infections or inflammations (e.g., chorioretinitis).
- Optic Nerve Lesions:
- Optic neuritis (e.g., associated with multiple sclerosis).
- Glaucoma (optic neuropathy characterized by progressive optic nerve damage).
- Ischemic optic neuropathy (anterior or posterior).
- Compressive optic neuropathy (e.g., from tumors, thyroid eye disease).
- Traumatic optic neuropathy.
- Papilledema (optic disc swelling due to increased intracranial pressure).
- Toxic or nutritional optic neuropathies.
- Lesions of Other Parts of the Brain Involved in Vision:
- Optic chiasm lesions (e.g., pituitary adenoma causing bitemporal hemianopia).
- Optic tract, lateral geniculate nucleus, optic radiation, or visual cortex lesions (due to stroke, tumor, trauma, inflammation), leading to various types of homonymous hemianopias or other field defects.
Differential Diagnosis of Common Visual Disturbances
| Symptom | Potential Causes (Non-Exhaustive) | Key Differentiating Features/Investigations |
|---|---|---|
| Blurred Vision (Gradual) | Refractive error, Cataract, Macular degeneration, Diabetic retinopathy, Glaucoma (chronic) | Refraction, Slit-lamp exam, Fundoscopy, OCT, Tonometry, Visual fields |
| Sudden Vision Loss (Painless) | Retinal detachment, Retinal artery occlusion, Retinal vein occlusion, Vitreous hemorrhage, Ischemic optic neuropathy, Stroke affecting visual pathway | Fundoscopy, Fluorescein angiography, OCT, B-scan ultrasound, Neuroimaging (CT/MRI) |
| Sudden Vision Loss (Painful) | Acute angle-closure glaucoma, Optic neuritis, Temporal arteritis (Giant Cell Arteritis), Corneal ulcer/abrasion, Uveitis | Tonometry, Slit-lamp exam, Fundoscopy, ESR/CRP (for GCA), Neurological exam |
| Visual Field Defects (e.g., Scotoma, Hemianopia) | Glaucoma, Optic neuropathy, Retinal detachment, Stroke, Brain tumor (chiasm, optic radiations, cortex), Migraine with aura | Perimetry (visual field testing), Fundoscopy, Neuroimaging (CT/MRI) |
| Color Vision Defects | Congenital color blindness, Optic neuropathy, Macular disease, Certain medications or toxins | Color vision testing (Ishihara, HRR, Farnsworth D-15), Fundoscopy, OCT |
| Diplopia (Double Vision) | Cranial nerve palsy (III, IV, VI), Myasthenia gravis, Thyroid eye disease, Orbital mass/fracture, Decompensated phoria | Ocular motility assessment, Neurological exam, Imaging (orbit/brain), Tensilon test (for MG) |
| Photophobia (Light Sensitivity) | Corneal abrasion/infection, Uveitis, Migraine, Meningitis, Certain medications | Slit-lamp exam, Neurological exam |
General Eye Health and Prevention of Vision Loss
Maintaining good eye health involves several practices:
- Regular Comprehensive Eye Examinations: Including dilation, especially for individuals over 40 or those with risk factors for eye diseases (diabetes, family history of glaucoma, etc.).
- Control of Systemic Diseases: Managing conditions like diabetes, hypertension, and high cholesterol, which can affect eye health.
- Healthy Diet: Rich in fruits, vegetables (especially leafy greens), and omega-3 fatty acids.
- UV Protection: Wearing sunglasses that block 100% of UVA and UVB rays.
- Avoid Smoking: Smoking increases the risk of macular degeneration, cataracts, and optic nerve damage.
- Eye Safety: Using protective eyewear during sports or hazardous activities.
- Managing Screen Time: Taking regular breaks (e.g., 20-20-20 rule: every 20 minutes, look at something 20 feet away for 20 seconds) to reduce eye strain.
When to Consult an Ophthalmologist or Neurologist
It is crucial to seek professional medical advice if any of the following symptoms occur:
- Sudden loss or significant decrease in vision in one or both eyes.
- Sudden onset of blurred vision or double vision.
- Appearance of flashes of light, new floaters, or a "curtain" or "shadow" in the field of vision (symptoms of retinal detachment).
- Eye pain, especially if severe or accompanied by redness or vision changes.
- Gradual but noticeable decline in visual acuity or changes in color perception.
- New or worsening visual field defects (e.g., peripheral vision loss, blind spots).
- Symptoms associated with increased intracranial pressure, such as persistent headache with transient visual obscurations or papilledema found on exam.
- Visual symptoms associated with neurological signs (e.g., weakness, numbness, speech changes).
An ophthalmologist is the primary specialist for most eye conditions. A neurologist or neuro-ophthalmologist may be consulted if visual symptoms are suspected to be related to optic nerve or brain pathology.
References
- Kandel ER, Schwartz JH, Jessell TM, Siegelbaum SA, Hudspeth AJ, Mack S. Principles of Neural Science. 6th ed. McGraw Hill; 2021. Chapters on Vision.
- Yanoff M, Duker JS. Ophthalmology. 5th ed. Elsevier; 2019.
- American Academy of Ophthalmology. Basic and Clinical Science Course (BCSC). Multiple sections (e.g., Section 1: Update on General Medicine; Section 2: Fundamentals and Principles of Ophthalmology; Section 5: Neuro-Ophthalmology; Section 12: Retina and Vitreous). San Francisco, CA: American Academy of Ophthalmology. (Published annually).
- Forrester JV, Dick AD, McMenamin PG, Roberts F, Pearlman E. The Eye: Basic Sciences in Practice. 4th ed. Saunders Elsevier; 2015.
- Bowling B, Kanski JJ. Kanski's Clinical Ophthalmology: A Systematic Approach. 9th ed. Elsevier; 2020.
- Walsh TJ, ed. Walsh & Hoyt's Clinical Neuro-Ophthalmology: The Essentials. 3rd ed. Lippincott Williams & Wilkins; 2016.
- Snellen H. Probebuchstaben zur Bestimmung der Sehschärfe. Utrecht: P. W. van de Weijer; 1862.
- Ishihara S. Tests for Colour-Blindness. Tokyo: Kanehara & Co; 1917.
See also
- Anatomy of the nervous system
- Spinal disc herniation
- Pain in the arm and neck (trauma, cervical radiculopathy)
- The eyeball and the visual pathway:
- Anatomy of the eye and physiology of vision
- The visual pathway and its disorders
- Eye structures and visual disturbances that occur when they are affected
- Retina and optic disc, visual impairment when they are affected
- Impaired movement of the eyeballs
- Nystagmus and conditions resembling nystagmus
- Dry Eye Syndrome
- Optic nerve and retina:
- Compression neuropathy of the optic nerve
- Edema of the optic disc (papilledema)
- Ischemic neuropathy of the optic nerve
- Meningioma of the optic nerve sheath
- Optic nerve atrophy
- Optic neuritis in adults
- Optic neuritis in children
- Opto-chiasmal arachnoiditis
- Pseudo-edema of the optic disc (pseudopapilledema)
- Toxic and nutritional optic neuropathy
- Neuropathies and neuralgia:
- Diabetic, alcoholic, toxic and small fiber sensory neuropathy (SFSN)
- Facial nerve neuritis (Bell's palsy, post-traumatic neuropathy)
- Fibular (peroneal) nerve neuropathy
- Median nerve neuropathy
- Neuralgia (intercostal, occipital, facial, glossopharyngeal, trigeminal, metatarsal)
- Post-traumatic neuropathies
- Post-traumatic trigeminal neuropathy
- Post-traumatic sciatic nerve neuropathy
- Radial nerve neuropathy
- Tibial nerve neuropathy
- Trigeminal neuralgia
- Ulnar nerve neuropathy
- Tumors (neoplasms) of the peripheral nerves and autonomic nervous system (neuroma, sarcomatosis, melanoma, neurofibromatosis, Recklinghausen's disease)
- Carpal tunnel syndrome
- Ulnar nerve compression in the cubital canal