Bacterial otogenic meningitis
Bacterial Otogenic Meningitis Causes
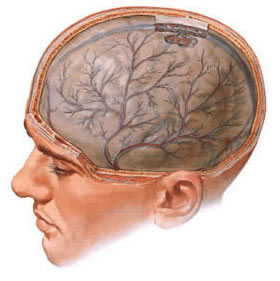
Meningitis is an inflammation of the leptomeninges (the pia mater and arachnoid mater, the inner two membranes) surrounding the brain and spinal cord. It can be caused by various pathogens, including bacteria, viruses, fungi, or parasites. Otogenic meningitis specifically refers to bacterial meningitis that arises as a complication of an infection originating in the middle ear cleft (middle ear cavity, Eustachian tube, mastoid air cells) [1]. Infection spreads from these ear structures into the subarachnoid space, the space containing cerebrospinal fluid (CSF), leading to meningeal inflammation.
Otogenic meningitis can also occur secondary to other established otogenic intracranial complications, such as epidural abscesses, subdural empyemas, intraparenchymal brain abscesses, or septic sigmoid sinus thrombosis, where the infection originating from the ear has already breached initial barriers and then extends into or seeds the subarachnoid space [2].
The most common bacterial species responsible for otogenic meningitis reflect the typical pathogens found in acute and chronic ear infections. Historically and currently, leading causes include: Streptococcus pneumoniae (pneumococcus) and Haemophilus influenzae type b (Hib - much less common now in vaccinated populations, but non-typeable strains still occur). Other important pathogens include Streptococcus pyogenes (Group A Strep), Staphylococcus aureus (particularly in chronic otitis or post-surgical cases), and less frequently, Gram-negative bacilli (like Pseudomonas aeruginosa, Proteus species, Klebsiella species, E. coli) especially in the context of chronic suppurative otitis media (CSOM) or cholesteatoma [3]. Anaerobic bacteria (e.g., Bacteroides, Peptostreptococcus) can also play a significant role, particularly in chronic infections. In some cases, despite clinical evidence of bacterial meningitis, initial CSF cultures may be negative ("culture-negative bacterial meningitis" or "aseptic meningitis" presentation), often due to prior antibiotic administration before lumbar puncture, or sometimes due to fastidious organisms.
The spread of infection from the middle ear/mastoid to the meninges occurs through several recognized pathways [4]:
- Direct Extension (Contiguous Spread): Infection erodes through the thin bony walls separating the middle ear/mastoid cavity from the intracranial dura mater (e.g., the tegmen tympani superiorly separating from the middle cranial fossa, or the posterior fossa dural plate posteriorly separating from the cerebellum/sigmoid sinus). This pathway is particularly common in complications arising from CSOM, chronic mastoiditis, or cholesteatoma, which are inherently bone-destructive processes. Pre-existing bony defects (congenital dehiscences, previous fractures, post-surgical defects) can also facilitate direct spread even from acute infections. Often, an epidural or subdural collection (abscess/empyema) forms as an intermediate stage before leptomeningitis develops.
- Labyrinthine Route: Infection spreads from the middle ear cavity directly into the inner ear structures (cochlea, vestibule, semicircular canals), causing suppurative labyrinthitis. From the infected inner ear, bacteria can then gain access to the subarachnoid space via pre-formed pathways like the cochlear aqueduct, vestibular aqueduct, or the internal auditory canal (following the vestibulocochlear nerve). This route is considered particularly important in the pathogenesis of meningitis complicating acute otitis media or acute labyrinthitis, especially in young children where these pathways may be more patent.
- Hematogenous Spread (Bloodborne): Bacteria from the localized ear infection enter the bloodstream (transient bacteremia), cross the blood-brain barrier, and directly seed the meninges. This pathway may be more typical in the early, fulminant stages of acute otitis media associated with highly virulent pathogens (like S. pneumoniae), particularly in infants and young children before immune responses contain the infection locally. This can lead to a rapidly progressing meningitis, sometimes without obvious signs of severe local ear disease initially.
- Thrombophlebitic Spread: Infection causes inflammation and septic clotting (thrombophlebitis) within small emissary veins draining the middle ear/mastoid air cells or within major adjacent dural venous sinuses (sigmoid sinus, superior petrosal sinus). Septic emboli can dislodge from these clots and travel through the bloodstream to seed the meninges, or the inflammation can spread directly along the venous walls into the subarachnoid space. Sigmoid sinus thrombosis is a well-known complication that frequently leads to meningitis or other intracranial issues.
Otogenic meningitis is a recognized complication of both acute otitis media (AOM), especially if complicated by acute mastoiditis, and chronic suppurative otitis media (CSOM), particularly the cholesteatomatous type (attic or pars flaccida disease) due to its bone-eroding nature. The relative frequency depends on the population and prevalence of effective AOM treatment and vaccination.
Pathologically, once bacteria reach the subarachnoid space, they incite an intense inflammatory response. The pia mater and arachnoid become inflamed, hyperemic (congested with blood), and edematous. Inflammatory mediators are released, increasing blood-brain barrier permeability. Neutrophils migrate into the CSF, leading to the accumulation of inflammatory exudate (initially serous, rapidly becoming purulent) in the CSF, particularly coating the brain surface, filling the sulci, and accumulating in the basal cisterns. This widespread inflammation (leptomeningitis) can extend to involve the underlying cerebral cortex (causing cerebritis or meningoencephalitis), cranial nerves traversing the subarachnoid space (leading to palsies), and blood vessels (causing vasculitis, vasospasm, or thrombosis leading to stroke). The dura mater may also show reactive inflammatory changes (pachymeningitis). In severe cases, the inflammatory exudate can obstruct CSF flow pathways (e.g., aqueduct of Sylvius, fourth ventricle outlets), leading to hydrocephalus, or impair CSF absorption at the arachnoid granulations.
Bacterial Otogenic Meningitis Symptoms and Clinical Presentation
The clinical presentation of bacterial meningitis, including otogenic meningitis, is typically acute, developing over hours to a few days. The classic clinical triad consists of fever, headache, and nuchal rigidity (neck stiffness), although studies show that only about 40-50% of patients present with all three [5]. The presence of altered mental status (ranging from lethargy to coma) is also a key feature, occurring in a majority of cases.
Key symptoms and signs include:
- Headache: Usually severe, generalized, persistent, often described as throbbing or bursting, and frequently the earliest prominent symptom.
- Fever: Typically high grade (≥38.5°C or 101.3°F), present in most patients, often accompanied by chills or rigors. Hypothermia can occur in severe sepsis or shock.
- Meningeal Signs (Signs of Meningeal Irritation):
- Nuchal Rigidity: Resistance and pain upon passive flexion of the neck towards the chest. Highly suggestive but may be absent in infants, elderly, deeply comatose, or severely immunocompromised patients.
- Kernig's Sign: Pain in the hamstrings and resistance upon attempting to passively extend the knee when the patient is supine with the hip flexed at 90 degrees.
- Brudzinski's Sign: Involuntary flexion of the patient's hips and knees when the examiner passively flexes the patient's neck.
- Note: Kernig's and Brudzinski's signs have relatively low sensitivity but higher specificity for meningitis.
- Altered Mental Status: A very common finding (>75%), ranging from mild confusion, irritability, lethargy, or drowsiness to delirium, obtundation, stupor, or deep coma (low Glasgow Coma Scale score). This reflects increased intracranial pressure (ICP), cortical inflammation/ischemia, or sepsis-associated encephalopathy.
- Photophobia and Phonophobia: Increased sensitivity to light and sound are common due to meningeal irritation.
- Nausea and Vomiting: Common, often severe, related to increased ICP and meningeal irritation.
- Other Neurological Signs:
- Seizures: Occur in about 20-30% of adults, more common in children. Can be focal or generalized, occurring early or later in the course.
- Focal Neurological Deficits: Occur in 10-30%. Cranial nerve palsies are common, especially involving CN VI (abducens nerve, causing lateral gaze palsy/diplopia due to susceptibility to raised ICP), CN III/IV (oculomotor/trochlear, causing other eye movement abnormalities), CN VII (facial nerve palsy, especially if otogenic source involves Fallopian canal), or CN VIII (vestibulocochlear nerve, causing sensorineural hearing loss - a common sequela). Hemiparesis, aphasia, or visual field defects are less common in uncomplicated meningitis and raise suspicion for associated complications like stroke (vasculitis/thrombosis), cerebritis, or abscess.
- Papilledema: Swelling of the optic discs due to sustained raised ICP. Usually takes time to develop (hours to days), so often absent on initial presentation but may appear later.
- Abnormal reflexes (e.g., positive Babinski sign) may indicate corticospinal tract involvement.
- Systemic Signs: Tachycardia (rapid heart rate) is common with fever and stress. Hypotension and signs of shock may indicate sepsis. A petechial or purpuric rash, especially if rapidly progressing, strongly suggests meningococcal meningitis but is typically absent in otogenic cases caused by other bacteria.
- Otological Signs: Evidence of the underlying acute or chronic ear infection may be present on examination (e.g., purulent otorrhea, tympanic membrane perforation or retraction, cholesteatoma debris, hearing loss, mastoid tenderness or swelling). However, signs of ear infection might be subtle or absent, especially if partially treated or if meningitis developed rapidly via hematogenous or labyrinthine routes.
Patients, particularly children, may exhibit irritability, lethargy, poor feeding, or adopt a characteristic posture with neck retraction (opisthotonos) and knee flexion to minimize meningeal stretch.
Laboratory findings typically show peripheral leukocytosis (high white blood cell count) with a predominance of neutrophils ('left shift') and often elevated inflammatory markers like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).
Cerebrospinal fluid (CSF) analysis obtained via lumbar puncture is the cornerstone of diagnosis [6, 7]. Perform LP promptly unless there are contraindications (clinical signs of severely raised ICP like coma, papilledema, posturing; new focal deficit; recent seizure; immunocompromised state; known CNS mass lesion - obtain head CT first in these cases to rule out mass effect/herniation risk). Typical CSF findings in bacterial meningitis include:
- Appearance: Turbid or grossly purulent (cloudy, milky, yellow/green).
- Opening Pressure: Markedly elevated (often >200-300 mmH2O; normal <180-200 mmH2O).
- White Blood Cell (WBC) Count: Markedly elevated (pleocytosis), typically ranging from 100 to >10,000 cells/mm3 (often thousands), with a strong predominance of neutrophils (>80%).
- Protein: Significantly elevated (often >100-500 mg/dL or >1-5 g/L; normal <45 mg/dL).
- Glucose: Markedly reduced (hypoglycorrhachia), typically <40 mg/dL (2.2 mmol/L), and the CSF/serum glucose ratio is usually low (<0.4, often <0.3).
- Gram Stain: May reveal causative bacteria (positive in ~60-90% of untreated cases, sensitivity varies by organism). Crucial for early pathogen identification.
- Bacterial Culture: Usually positive (~70-85% sensitivity before antibiotics), identifies the specific organism and allows susceptibility testing to guide targeted therapy.
- Other Tests: Bacterial antigen tests (e.g., latex agglutination) or PCR panels (multiplex PCR for common pathogens) can be useful for rapid diagnosis or if cultures are negative after antibiotic administration.
The widespread use of oral antibiotics for preceding infections (like otitis media) can significantly modify the clinical picture and CSF findings ("partially treated meningitis"). Symptoms may be less severe or subacute, fever lower, meningeal signs less pronounced. CSF findings can be atypical: lower WBC count, potential shift towards lymphocyte predominance later, higher glucose, potentially normal protein, and often negative Gram stain and culture, making diagnosis more challenging. Clinical suspicion must remain high.
With prompt diagnosis, initiation of appropriate high-dose IV antibiotics, and timely surgical management of the otogenic source if required, the prognosis for uncomplicated otogenic meningitis is generally favorable, although neurological sequelae (especially hearing loss) can occur. However, delays in treatment, presence of resistant organisms, development of intracranial complications (abscess, empyema, hydrocephalus, stroke), or fulminant presentation significantly worsen outcomes, increasing morbidity and mortality.
Bacterial Otogenic Meningitis Diagnosis
The diagnosis of bacterial meningitis relies on recognizing the clinical syndrome (fever, headache, neck stiffness, altered mental status) and confirming it with cerebrospinal fluid (CSF) analysis demonstrating characteristic findings (neutrophilic pleocytosis, high protein, low glucose). Identifying the specific bacterial pathogen via CSF Gram stain, culture, or molecular methods (PCR) is ideal.
Establishing the meningitis as otogenic (originating from the ear) requires linking the meningitis episode to a concurrent or recent infection of the middle ear or mastoid. Key diagnostic steps include:
- Clinical Correlation: A detailed history focusing on preceding or current ear symptoms (otalgia, otorrhea, hearing loss, vertigo), history of recurrent or chronic ear infections, previous ear surgery, or head trauma involving the temporal bone. Physical examination confirming signs of acute otitis media (AOM), chronic suppurative otitis media (CSOM), cholesteatoma, or acute mastoiditis (postauricular swelling, erythema, tenderness) strongly supports an otogenic source.
- Neuroimaging: Essential both to rule out contraindications to LP (mass effect) and to identify the otogenic source and associated complications.
- High-Resolution CT Scan of the Temporal Bones: This is crucial for evaluating the bony anatomy of the middle ear, mastoid, and inner ear structures. It accurately demonstrates the extent of mastoid opacification, presence of fluid, signs of bone erosion (destruction of the tegmen tympani, sigmoid plate, semicircular canals), presence of cholesteatoma (soft tissue mass with bone erosion), and potential bony defects that could serve as pathways for infection spread [8].
- MRI of the Brain with Gadolinium Contrast: Primarily used to assess the intracranial effects. It confirms meningitis by showing diffuse enhancement of the leptomeninges after contrast. Critically, it evaluates for associated intracranial complications commonly linked to otogenic sources: epidural abscess, subdural empyema, intraparenchymal brain abscess (especially temporal lobe or cerebellum), venous sinus thrombosis (MR Venography - MRV is often included), hydrocephalus, cerebritis, or labyrinthitis (enhancement of inner ear structures) [2].
- CSF Analysis: Confirms bacterial meningitis but usually does not identify the source. The specific bacteria isolated might offer clues (e.g., Pseudomonas strongly suggests chronic otitis source).
- Microbiology: Positive cultures from middle ear discharge (if present), mastoid aspirate (if surgery performed), or blood cultures, yielding typical otogenic pathogens, further support the link.
- Differential Diagnosis (of Meningitis source & type): Differentiating otogenic meningitis from meningitis originating from other sites (paranasal sinuses, pneumonia/bacteremia, neurosurgery, CSF leak) relies heavily on clinical history and imaging findings identifying the primary focus. Differentiating bacterial from other types of meningitis (viral, fungal, TB) depends primarily on CSF analysis (see table below).
Differential Diagnosis of Acute Meningitis Syndrome
| Condition | Key Clinical Features | Typical CSF Findings (Requires LP) | Other Diagnostics |
|---|---|---|---|
| Bacterial Meningitis (e.g., Otogenic, Pneumococcal, Meningococcal) | Acute onset (<24-48h), high fever, headache, neck stiffness, altered mental status. +/- Seizures, focal deficits, rash (meningococcal). Identify source (ear, sinus, lungs etc.). | Turbid. High pressure. WBC >1000 (often >>), >80% Neutrophils. High Protein (>100 mg/dL). Low Glucose (<40 mg/dL or ratio <0.4). Positive Gram stain (~60-90%), Culture (~70-85%). | Blood cultures. Imaging (CT/MRI) to rule out mass/complications & identify source (Otogenic, Sinusitis-associated). PCR panels on CSF. |
| Viral Meningitis (e.g., Enterovirus, HSV-2, VZV) | Acute onset, fever, headache, neck stiffness, photophobia. Usually less severe than bacterial, mental status often clearer initially. | Clear/slightly turbid. Normal/slight high pressure. WBC 10-1000 (usually <300), Lymphocyte predominant (may be neutrophils early). Normal/slight high Protein. Normal Glucose. Negative Gram stain/bacterial culture. | CSF PCR for specific viruses (Enterovirus, HSV, VZV). Clinical course often self-limited. |
| Viral Encephalitis (e.g., HSV-1, West Nile, Arboviruses) | Similar to viral meningitis but prominent altered mental status, confusion, lethargy, personality changes, focal neurological deficits (hemiparesis, aphasia), seizures reflecting brain parenchyma involvement. | CSF often similar to viral meningitis (lymphocytic pleocytosis, normal glucose), may have RBCs (esp. HSV). Protein often more elevated. | MRI Brain essential, shows characteristic parenchymal T2/FLAIR signal changes (e.g., temporal lobes in HSV-1). EEG often abnormal (focal/diffuse slowing, PLEDs). CSF PCR for viruses. |
| Tuberculous (TB) Meningitis | Subacute onset (days to weeks). Headache, low-grade fever, malaise, night sweats, weight loss, confusion, cranial nerve palsies (esp. VI, III, IV, VII). History of TB exposure/risk factors (HIV, endemic area). | Clear/viscous/web-like clot. High pressure. WBC 100-500, Lymphocyte predominant. Very High Protein (>150-500 mg/dL). Very Low Glucose (<40 mg/dL). AFB stain low sensitivity (~10%). Culture (~50-70%, slow). PCR more rapid. Adenosine deaminase (ADA) elevated. | Chest X-ray (pulmonary TB). MRI brain may show basal meningeal enhancement, hydrocephalus, tuberculomas, infarcts. PPD/IGRA test. |
| Fungal Meningitis (e.g., Cryptococcus, Candida, Coccidioides) | Often subacute/chronic onset. Common in immunocompromised (HIV/AIDS, transplant, steroids). Headache, fever, altered mental status. Neck stiffness may be mild or absent. | Clear/viscous. High pressure. WBC 20-500, Lymphocyte predominant. High Protein. Low Glucose. India ink stain (Crypto), Cryptococcal antigen test (serum/CSF, high sensitivity/specificity), Fungal culture (may be slow), Beta-D-glucan assay. | Assess immune status (HIV test). MRI brain may show enhancement, cryptococcomas, gelatinous pseudocysts. Chest imaging. |
| Subarachnoid Hemorrhage (SAH) | Sudden, severe "thunderclap" headache. Neck stiffness (meningeal irritation from blood), photophobia, altered consciousness. Fever possible due to chemical meningitis from blood. No primary infection source usually. | CSF: Uniformly bloody appearance (all tubes), high RBC count (no clearing). Xanthochromia (yellow supernatant after spinning, indicates prior bleeding) develops after several hours. High pressure/protein common. Glucose normal. | Non-contrast CT head is primary diagnostic test (high sensitivity early). LP used if CT negative but suspicion high. CTA/DSA needed to find source (aneurysm). |
| Parameningeal Focus (e.g., Subdural Empyema, Brain Abscess, Epidural Abscess) | May present with headache, fever, neck stiffness mimicking meningitis, but often prominent focal neurological deficits and/or seizures occur early. History of sinusitis/otitis/trauma common. | LP often contraindicated due to mass effect risk. If performed, CSF may be normal or show reactive changes (mild pleocytosis/protein elevation) unless rupture occurs. | Contrast-enhanced MRI Brain is diagnostic, shows characteristic extra-axial collection (SDE, EDA) or intraparenchymal ring-enhancing lesion (abscess). |
| Non-infectious Inflammatory Meningitis (e.g., Lupus, Sarcoidosis, Behçet's, Drug-induced) | Variable onset (often subacute/chronic). Headache, neck stiffness, +/- fever, may have cranial neuropathies or other systemic features of underlying disease. History of specific drug exposure. | CSF shows aseptic pattern (lymphocytic pleocytosis, normal glucose, variable protein). Negative cultures/stains. Specific markers may be present (e.g., ACE in sarcoidosis). | Diagnosis requires excluding infection and identifying underlying systemic disease or drug exposure. MRI may show meningeal enhancement. |
LP = Lumbar Puncture. LP should only be performed after excluding contraindications, particularly signs of significant increased intracranial pressure or mass effect on neuroimaging if indicated.
In a patient presenting with confirmed bacterial meningitis and concurrent imaging or clinical evidence of acute or chronic suppurative otitis media and/or mastoiditis, an otogenic source is highly likely. This warrants prompt otolaryngology (ENT) consultation regarding potential surgical intervention on the ear/mastoid, which is often necessary in addition to antibiotic therapy for source control.
Surgical exploration of the mastoid and middle ear can sometimes provide definitive confirmation by revealing direct evidence of infection spread, such as osteomyelitis, bony defects eroded through to the dura, granulation tissue tracking intracranially, or associated epidural/subdural collections requiring drainage. Persistent meningitis or neurological deficits despite appropriate antibiotics should strongly raise suspicion for an undiagnosed, inadequately drained otogenic complication (e.g., occult abscess, venous sinus thrombosis), requiring repeat, detailed imaging (usually MRI/MRV).
Bacterial Otogenic Meningitis Treatment
The management of bacterial otogenic meningitis is a medical and often surgical emergency requiring prompt hospitalization, rapid initiation of appropriate therapy, and typically collaboration between infectious disease specialists, otolaryngologists (ENT surgeons), neurologists, and potentially neurosurgeons [9].
- Antibiotic Therapy: Immediate administration of high-dose, broad-spectrum intravenous (IV) antibiotics that achieve good penetration across the blood-brain barrier is the cornerstone of treatment and should be started empirically as soon as bacterial meningitis is suspected (ideally after blood cultures drawn, but without delaying the first dose for LP or imaging unless absolutely necessary for safety) [6, 7].
- Initial empiric therapy must cover the most likely otogenic pathogens, including resistant S. pneumoniae, H. influenzae (including non-typeable), other Streptococci, S. aureus, and potentially Gram-negatives/anaerobes if CSOM is the source.
- A common empiric regimen for adults includes: Vancomycin (for resistant pneumococci and MRSA) PLUS a third-generation cephalosporin (e.g., Ceftriaxone 2g IV q12h or Cefotaxime 2g IV q4-6h).
- Metronidazole is often added if anaerobic infection is suspected (e.g., source is CSOM, cholesteatoma, brain abscess).
- Coverage may need adjustment based on age (e.g., add ampicillin for Listeria coverage in infants/elderly/immunocompromised, though less relevant for typical otogenic source), local resistance patterns, and patient factors (e.g., penicillin allergy requires alternative regimen like meropenem +/- vancomycin).
- Antibiotic therapy is subsequently tailored based on CSF Gram stain results (if positive) and definitive culture and susceptibility results.
- Duration of IV antibiotic therapy is typically prolonged for meningitis complicated by an adjacent focus, often 10-14 days at minimum, and frequently longer (e.g., 3 weeks or more) depending on the pathogen, clinical response, and presence of associated complications (abscess, osteomyelitis) [10].
- Adjunctive Dexamethasone: Administration of corticosteroids (dexamethasone 0.15 mg/kg IV q6h for 2-4 days) initiated just before or concurrently with the first dose of antibiotics is generally recommended for suspected bacterial meningitis in adults and children (> 6 weeks old) in high-income countries, primarily to reduce the inflammatory response and decrease the risk of neurological sequelae, particularly hearing loss associated with S. pneumoniae meningitis [11]. Its benefit is most established for pneumococcal meningitis. While specific data on purely otogenic meningitis may be limited, it is often administered empirically given the high prevalence of pneumococcus as a cause. It should generally be discontinued if a non-bacterial diagnosis is made or if the pathogen is proven not to be pneumococcus (though practice varies).
- Surgical Management of the Otogenic Source: Eradication of the primary infectious focus in the middle ear/mastoid is often essential for definitive treatment, source control, and prevention of recurrence, especially in cases arising from chronic otitis media, cholesteatoma, or acute mastoiditis with coalescence or subperiosteal abscess [12]. This typically involves:
- Mastoidectomy: The type depends on the underlying pathology. A complete mastoidectomy (canal wall up or down) is usually necessary to remove all infected air cells and diseased tissue. A radical or modified radical mastoidectomy is often required for cholesteatoma removal. The goal is to create a safe, aerated space and eliminate the source communicating with the intracranial cavity.
- Dural Exposure and Inspection: During mastoidectomy, the surgeon typically exposes the dura of the middle cranial fossa (tegmen tympani) and posterior cranial fossa (sigmoid sinus plate) widely to identify any granulations, inflammation, defects, fistulae, or associated epidural/subdural collections.
- Drainage of Associated Complications: If concurrent epidural abscess, subdural empyema, or easily accessible brain abscess related to the otogenic source are identified, they require appropriate surgical drainage, often performed concurrently by the ENT surgeon or in conjunction with neurosurgery.
- Timing of Surgery: Urgent mastoidectomy (often within 24-48 hours of diagnosis and medical stabilization) is generally indicated for otogenic meningitis associated with acute coalescent mastoiditis, subperiosteal abscess, cholesteatoma, or CT evidence of significant bone destruction/intracranial collection. Surgery may sometimes be delayed slightly in uncomplicated AOM-related meningitis if rapid clinical improvement occurs with antibiotics alone, but close monitoring and low threshold for surgery remain [13].
- Supportive Care: Essential for managing critically ill patients. Includes:
- Close neurological monitoring (GCS, pupils).
- Management of fever (antipyretics).
- Pain control (analgesics).
- Intravenous fluids for hydration and electrolyte balance (avoiding fluid overload which can worsen cerebral edema).
- Nutritional support.
- Monitoring for and managing complications like seizures (antiepileptic drugs if occur), increased ICP, septic shock, disseminated intravascular coagulation (DIC), syndrome of inappropriate antidiuretic hormone secretion (SIADH).
- Management of Increased Intracranial Pressure (ICP): If clinical signs (deteriorating consciousness, pupillary changes, posturing) or imaging suggest significantly raised ICP or developing hydrocephalus:
- Elevate head of bed (30 degrees).
- Consider osmotic therapy (Mannitol or hypertonic saline).
- Controlled ventilation (avoiding hypercapnia, cautious use of brief hyperventilation only for impending herniation).
- ICP monitoring may be considered in comatose patients.
- Urgent neurosurgical consultation for potential CSF diversion (EVD placement) or decompressive surgery in refractory cases.
- Follow-up Lumbar Punctures (LPs): Repeat LPs are generally not performed routinely if the patient is improving clinically as expected. They may be considered after 24-48 hours of therapy if the initial diagnosis was uncertain, if the organism was resistant, or if the patient fails to show clinical improvement, to assess CSF sterilization and inflammatory response.
Successful treatment relies on the rapid initiation of appropriate antibiotics combined with timely surgical control of the infectious source in the ear/mastoid when indicated. Delay in either component significantly increases the risk of mortality and long-term neurological sequelae such as hearing loss, cognitive impairment, seizures, or focal deficits.
![]() Attention! Bacterial meningitis is a medical emergency. Suspected cases require immediate medical evaluation, lumbar puncture (if safe), and prompt initiation of empiric antibiotic therapy. Otogenic meningitis needs specific attention to the ear source, usually requiring ENT involvement and potential surgery.
Attention! Bacterial meningitis is a medical emergency. Suspected cases require immediate medical evaluation, lumbar puncture (if safe), and prompt initiation of empiric antibiotic therapy. Otogenic meningitis needs specific attention to the ear source, usually requiring ENT involvement and potential surgery.
References
- Chapter on Intracranial Complications of Otitis Media. In: Bailey BJ, Johnson JT, Newlands SD, eds. Head & Neck Surgery - Otolaryngology. 5th ed. Lippincott Williams & Wilkins; 2014.
- Osborn AG, Salzman KL, Jhaveri MD, et al. Osborn's Brain. 2nd ed. Elsevier; 2018.
- Merkus P, et al. Intracranial complications of otitis media: predictors of outcome. Eur Arch Otorhinolaryngol. 2015;272(3):571-7. doi: 10.1007/s00405-014-3024-6
- Barry B, et al. Otogenic intracranial infections: a 15-year retrospective review. Am J Otolaryngol. 2013;34(6):680-4. doi: 10.1016/j.amjoto.2013.05.006
- van de Beek D, et al. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med. 2004;351(18):1849-59. doi: 10.1056/NEJMoa040845
- Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis. 2004;39(9):1267-84. doi: 10.1086/425368
- Tunkel AR, Hasbun R, Bhimraj A, et al. 2017 Infectious Diseases Society of America’s Clinical Practice Guidelines for Healthcare-Associated Ventriculitis and Meningitis. Clin Infect Dis. 2017;64(6):e34-e65. doi: 10.1093/cid/ciw861
- Lo WWM, et al. Intracranial complications of sinus and otic infections. Neuroimaging Clin N Am. 2004;14(2):197-218. doi: 10.1016/j.nic.2004.03.005
- Manolidis S, et al. Complications of otitis media. In: Snow JB, Wackym PA, eds. Ballenger's Otorhinolaryngology Head and Neck Surgery. 17th ed. BC Decker; 2009.
- Southwick FS. Treatment of bacterial meningitis. UpToDate. Accessed [Insert Access Date - e.g., April 20, 2024]. (Subscription required - represents current clinical practice summary)
- van de Beek D, et al. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst Rev. 2007;(1):CD004405. Updated 2015. doi: 10.1002/14651858.CD004405.pub5
- Palma S, et al. Surgical treatment of otogenic intracranial complications: personal experience. Acta Otorhinolaryngol Ital. 2011;31(5):311-6.
- Cassano P, et al. Management of otogenic lateral sinus thrombosis. J Otolaryngol. 2003;32(1):11-5. doi: 10.2310/7070.2003.11115
See also
- Anatomy of the nervous system
- Central nervous system infection:
- Brain abscess (lobar, cerebellar)
- Eosinophilic granuloma, Langerhans cell histiocytosis (LCH), Hennebert's symptom
- Epidural brain abscess
- Sinusitis-associated intracranial complications
- Otogenic intracranial complications
- Sinusitis-associated ophthalmic complications
- Bacterial otogenic meningitis
- Subdural brain abscess
- Sigmoid sinus suppurative thrombophlebitis
- Cerebral 3rd Ventricle Colloid Cyst
- Cerebral and spinal adhesive arachnoiditis
- Corticobasal Ganglionic Degeneration (Limited Brain Atrophy)
- Encephalopathy
- Headache, migraine
- Traumatic brain injury (concussion, contusion, brain hemorrhage, axonal shearing lesions)
- Increased intracranial pressure and hydrocephalus
- Parkinson's disease
- Pituitary microadenoma, macroadenoma and nonfunctioning adenomas (NFPAs), hyperprolactinemia syndrome
- Spontaneous cranial cerebrospinal fluid leak (CSF liquorrhea)