Brain and skull base CT scan
Head CT Scan (Brain)
A Head CT (Computed Tomography) scan is a non-invasive imaging method that uses X-rays and computer processing to create detailed cross-sectional images of the brain, intracranial spaces, skull bones, and surrounding soft tissues. The technique relies on measuring how different tissues absorb X-ray beams, allowing for mathematical reconstruction of the internal structures.
A Head CT scan can visualize the following structures, often allowing for viewing in different planes (axial, coronal, sagittal) and 3D reconstructions:
- Brain parenchyma (grey and white matter)
- Ventricles (fluid-filled spaces within the brain)
- Cranial nerves (partially, especially at the skull base)
- Blood vessels (arteries, veins, venous sinuses) - especially with CT Angiography (CTA)
- Skull bones (calvarium and skull base)
- Paranasal sinuses
- Orbits and their contents
- Soft tissues of the scalp and face
Skull Base CT Anatomy
Computed tomography (CT) provides excellent detail of the complex bony anatomy of the skull base. Key structures visible include:
- a. Pterygopalatine fossa: A small space behind the maxilla connecting multiple regions. Communications: nasal cavity via the sphenopalatine foramen (1), masticator space via the pterygomaxillary fissure, orbit via the inferior orbital fissure, cavernous sinus via foramen rotundum, middle cranial fossa via the vidian canal (2) and the palate via the greater palatine canal.
- b. Foramen ovale: An opening in the sphenoid bone transmitting the mandibular nerve (V3), accessory meningeal artery, and other structures.
- c. Carotid canal: Passage in the temporal bone for the internal carotid artery and sympathetic nerves.
- d. Incus: The middle ear ossicle, articulating with the malleus (3) and stapes (4).
- e. Facial nerve (CN VII): Seen here in its descending (mastoid) portion after passing near the lateral semicircular canal.
- f. Petroclival synchondrosis: The cartilaginous joint between the petrous temporal bone and the clivus (part of the occipital bone). A common site for chondrosarcomas.
- g. Cochlear aperture: Opening where the cochlear nerve enters the cochlea from the internal acoustic canal.
- h. Groove for the sigmoid sinus: The S-shaped path of this major dural venous sinus leading towards the jugular foramen.
Indications for Head CT Scan
A Head CT scan is frequently performed in emergency and non-emergency settings for various suspected conditions:
- Head Trauma: To detect skull fractures, intracranial hemorrhage (epidural, subdural, subarachnoid, intraparenchymal), contusions, diffuse axonal injury (though MRI is more sensitive for DAI), and signs of increased intracranial pressure. (Traumatic brain injury)
- Stroke Symptoms: Especially sudden onset neurological deficits. Non-contrast CT is crucial initially to rapidly differentiate between ischemic stroke (blockage) and hemorrhagic stroke (bleeding), guiding immediate treatment. (Stroke)
- Sudden Severe Headache: To rule out subarachnoid hemorrhage, often from a ruptured aneurysm, or other acute intracranial pathology.
- Suspected Brain Tumor: While MRI is often preferred for detailed tumor characterization, CT (especially with contrast) can detect many primary or metastatic brain tumors, assess associated mass effect, edema, or hydrocephalus.
- Hydrocephalus: To evaluate the size of the ventricles and identify potential causes of cerebrospinal fluid (CSF) blockage or impaired absorption.
- Infections: To detect brain abscesses, empyema (pus collection), meningitis complications, or encephalitis (though MRI is often more sensitive). (Brain abscess)
- Congenital Abnormalities: Evaluation of skull shape abnormalities or suspected structural brain defects.
- Sinusitis and Orbital Conditions: CT provides excellent detail of the paranasal sinuses and bony orbits for evaluating infection, inflammation, or tumors.
- Skull Base Pathology: Evaluation of fractures, tumors, infections (like mastoiditis), or CSF leaks involving the skull base. (CSF liquorrhea)
- Altered Mental Status or Seizures: To investigate acute structural causes.
- Post-Operative Evaluation: To assess for complications after neurosurgery.
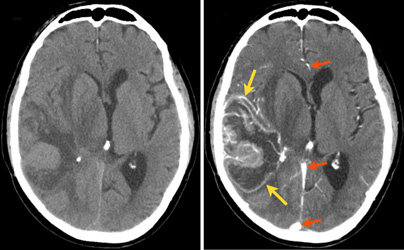
CT Findings in Head Trauma
Head CT is the primary imaging tool in acute head trauma. Key findings include:
- Soft Tissue Injuries: Scalp hematomas or lacerations appear as localized thickening or disruption of soft tissues, sometimes with increased density due to blood infiltration. CT helps assess depth and relation to underlying fractures. Subgaleal hematomas (under the scalp aponeurosis) are distinct.
- Skull Fractures: Linear fractures are best seen if the scan plane aligns well or if there's displacement. Depressed fractures, where bone fragments are pushed inwards, are clearly visualized, allowing assessment of depth and size. CT can show foreign bodies or air within wound tracks.
- Epidural Hematoma (EDH): Typically appears as a lens-shaped (biconvex) collection of blood between the dura mater and the inner skull table. Usually caused by arterial bleeding associated with a skull fracture. Atypical forms (sickle-shaped, multiple) can occur. Acute blood is typically hyperdense (bright) on CT.
- Subdural Hematoma (SDH): Usually crescent-shaped, spreading more widely over the brain surface, located between the dura mater and the arachnoid mater. Often caused by tearing of bridging veins. Acute SDH is also hyperdense. They can be bilateral or extend along the falx cerebri or tentorium cerebelli.
- Intraparenchymal Hemorrhage / Contusion: Bleeding directly within the brain tissue, often seen at sites of direct impact (coup) or opposite the impact (contrecoup). Appears as areas of increased density, often surrounded by edema (darker area).
- Subarachnoid Hemorrhage (SAH): Blood within the subarachnoid space (sulci, cisterns, fissures). Appears as hyperdensity outlining these spaces.
- Intraventricular Hemorrhage (IVH): Blood within the ventricles.
- Diffuse Axonal Injury (DAI): Often characterized by widespread brain swelling (edema) causing compression of ventricles and cisterns. Small petechial hemorrhages may be seen in characteristic locations (corpus callosum, brainstem, grey-white matter junction), but major findings might be subtle on CT; MRI is more sensitive.
- Cerebral Edema / Swelling: Can be focal (around a contusion or hematoma) or diffuse. Appears as areas of decreased density (darker brain tissue) with effacement (compression) of sulci, ventricles, and basal cisterns.
- Herniation: Displacement of brain structures due to mass effect (e.g., subfalcine, uncal, transtentorial herniation), visible as shifting of midline structures or compression of brainstem and cisterns.
The appearance of hematomas changes over time. Acute hematomas (first few days) are hyperdense (bright). Subacute hematomas (days to weeks) become isodense (similar density to brain) and then hypodense (darker). Chronic hematomas (weeks to months) are typically hypodense.
Post-Traumatic Changes & Complications
CT also plays a role in evaluating the consequences and complications of head injury:
- Cerebral Atrophy: Diffuse or focal loss of brain volume, seen as enlarged ventricles and sulci, occurring later after injury.
- Encephalomalacia: Softening or loss of brain tissue in an area of prior injury (contusion, infarction), appearing as a low-density area, sometimes cystic.
- Post-traumatic Hydrocephalus: Enlargement of the ventricles due to impaired CSF flow or absorption following trauma or hemorrhage. CT shows enlarged ventricles, often rounded, sometimes with periventricular low density indicating CSF seepage.
- Chronic Subdural Hematoma / Hygroma: Chronic SDH appears as a crescent-shaped collection that can be hypodense, isodense, or mixed density. Membranes may be visible. Hygromas are collections of clear CSF-like fluid in the subdural space, appearing as low density.
- Leptomeningeal Cysts (Growing Fractures): Rare complication, usually in children, where a dural tear associated with a fracture allows brain or meninges to herniate outwards, leading to progressive bone erosion.
- Infections (Post-traumatic):
- Cerebritis/Abscess: Early inflammation (cerebritis) appears as an ill-defined low-density area, possibly with patchy enhancement. A mature abscess typically has a central low-density (pus) area surrounded by a distinct, ring-enhancing capsule on contrast-enhanced CT, often with significant surrounding edema.
- Empyema (Subdural/Epidural): Collections of pus in the subdural or epidural space. Appear as fluid collections, often enhancing along the margins after contrast administration. Epidural empyema is typically lens-shaped, while subdural empyema is crescent-shaped.
- Pneumocephalus: Air within the cranial cavity, usually due to a skull base fracture or penetrating injury. Appears as very low density (black) areas on CT.
- CSF Leak: Can occur with skull base fractures. Specialized CT cisternography (involving intrathecal contrast) may be needed for precise localization.
Advanced CT techniques allow for thin-section acquisition, enabling multiplanar reformation (MPR) and three-dimensional (3D) reconstructions, which are particularly useful for evaluating complex fractures and planning surgery. CT Angiography (CTA) and CT Venography (CTV) specifically visualize arteries and veins after contrast injection.
Preparation for the Scan
Preparation for a Head CT scan is often minimal, especially in emergencies:
- Clothing and Metal Objects: You will need to remove metal objects from your head and neck area that could interfere with the images, such as eyeglasses, hairpins, jewelry (earrings, necklaces), and dentures. You might be asked to wear a hospital gown.
- Contrast Material: If intravenous (IV) contrast material is planned (e.g., for suspected tumor, infection, or vascular issues), you might be asked to fast for a few hours beforehand. Inform the staff about any allergies (especially to iodine or previous contrast reactions) or kidney problems.
- Medical History: Inform your doctor or the technologist about any relevant medical conditions, current medications, and if there's any possibility you might be pregnant.
- Emergency Scans: For trauma or acute stroke evaluation (often done without contrast initially), minimal preparation is usually required beyond removing interfering objects.
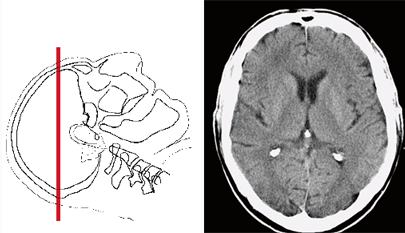
The CT Procedure
During the Head CT scan:
- You will lie on your back on the CT scanner table, which will slide into the large, doughnut-shaped opening of the scanner.
- A head holder or cradle may be used to help keep your head comfortably positioned and still during the scan. It is important to remain motionless to avoid blurring the images.
- If IV contrast is used, a small IV line will be placed in a vein in your arm or hand prior to or during the scan.
- The scanner will rotate around your head, taking multiple X-ray images from different angles. You might hear whirring or clicking sounds.
- The technologist will monitor the scan from an adjacent control room and can communicate with you via an intercom.
- The actual scanning time for a head CT is very fast, often completed in under a minute, although the total time in the room might be 5-15 minutes including positioning and setup.
Use of Contrast Material
Intravenous (IV) contrast material (an iodine-based liquid) may be used in certain situations to enhance the visibility of specific structures or pathologies:
- When is it used? Contrast is often used when investigating suspected brain tumors, infections (abscess, meningitis), inflammation, or certain vascular conditions (though dedicated CTA/CTV is usually preferred for vessels). It helps highlight areas where the blood-brain barrier is disrupted or where there is increased blood supply.
- When is it often NOT used? Initial evaluation for acute stroke (to detect hemorrhage), acute head trauma (to detect blood and fractures), routine sinus evaluation, or initial assessment of hydrocephalus are often performed *without* IV contrast.
- Administration: If used, the contrast is injected through the IV line during the scan. You might feel a temporary warm sensation or metallic taste.
Risks and Benefits
Benefits:
- Head CT is extremely fast, widely available, and highly effective for evaluating acute conditions like head trauma and stroke.
- Excellent at visualizing bone detail (fractures) and acute hemorrhage (bleeding).
- Less sensitive to patient motion than MRI.
- Can be performed safely in patients with most implanted medical devices.
Risks:
- Radiation Exposure: CT scans use ionizing radiation. While efforts are made to minimize the dose (ALARA principle), there is a small theoretical long-term risk associated with radiation exposure, especially with multiple scans. The benefit of an accurate diagnosis in acute situations typically far outweighs this risk.
- Contrast Reaction: If IV contrast is used, there is a small risk of allergic-like reactions, ranging from mild (hives, itching) to rare, severe reactions. Patients with previous reactions, significant allergies, or asthma may be at higher risk.
- Kidney Issues: IV contrast can potentially affect kidney function, particularly in individuals with pre-existing kidney disease. Kidney function screening may be done beforehand in at-risk patients.
- Pregnancy: CT scans are generally avoided in pregnant patients unless medically essential due to potential radiation risk to the fetus.
References
- Radiological Society of North America (RSNA) & American College of Radiology (ACR). (2022). Head CT (Computed Tomography). RadiologyInfo.org. Retrieved from https://www.radiologyinfo.org/en/info/headct
- Mayo Clinic Staff. (2022). CT scan. Mayo Clinic Patient Care & Health Information. Retrieved from https://www.mayoclinic.org/tests-procedures/ct-scan/about/pac-20393675
- National Institute of Biomedical Imaging and Bioengineering (NIBIB). (n.d.). Computed Tomography (CT). NIH - National Institutes of Health. Retrieved from https://www.nibib.nih.gov/science-education/science-topics/computed-tomography-ct
- Osborn, A. G., Hedlund, G. L., & Salzman, K. L. (2018). *Osborn's Brain: Imaging, Pathology, and Anatomy* (2nd ed.). Elsevier. [Note: Comprehensive neuroradiology textbook reference]
- American College of Radiology. (2023). ACR Manual on Contrast Media. Retrieved from https://www.acr.org/Clinical-Resources/Contrast-Manual