Spontaneous intracranial (subarachnoid) and intracerebral hemorrhage
Spontaneous Intracranial Hemorrhage: Overview
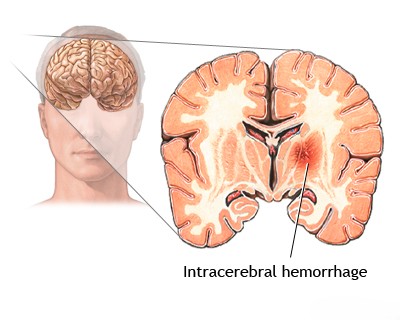
Spontaneous intracranial hemorrhage (ICH) refers to bleeding within the cranial cavity that is not caused by trauma [1]. It is a major subtype of stroke, often termed hemorrhagic stroke [1]. This bleeding can occur in different locations [1, 2]:
- Intracerebral Hemorrhage (ICH): Bleeding directly into the brain parenchyma (tissue).
- Subarachnoid Hemorrhage (SAH): Bleeding into the subarachnoid space, the area between the brain and the membranes covering it, where cerebrospinal fluid (CSF) circulates.
- Intraventricular Hemorrhage (IVH): Bleeding into the brain's ventricular system (often an extension from ICH or SAH).
- Subdural or Epidural Hemorrhage: Usually traumatic, but rare spontaneous cases can occur (less common focus here).
The location, size, and underlying cause of the hemorrhage determine the clinical presentation and prognosis [1]. Common causes vary depending on the type of hemorrhage. For instance, ruptured saccular aneurysms are the most frequent cause of spontaneous SAH, while chronic hypertension is the leading cause of spontaneous deep ICH [1, 2]. Vascular malformations like arteriovenous malformations (AVMs) can cause both ICH and SAH [1].
Less frequent causes include bleeding disorders, rupture of mycotic (infectious) aneurysms, hemorrhage into brain tumors, hemorrhagic transformation of an ischemic stroke, and rare vascular conditions [1, 2]. Brainstem hemorrhages can also occur due to transtentorial herniation (Duret hemorrhages) [1].
Causes of Spontaneous Intracranial Hemorrhage
The specific causes often correlate with the type and location of bleeding [1, 2]:
Primary Causes of Intracerebral Hemorrhage (ICH):
- Hypertensive Vasculopathy: Chronic hypertension damages small penetrating arteries (arteriolosclerosis, lipohyalinosis), leading to rupture, typically in deep brain structures (basal ganglia, thalamus, pons, cerebellum). This is the most common cause of spontaneous ICH.
- Cerebral Amyloid Angiopathy (CAA): Deposition of amyloid protein in the walls of small-to-medium cortical and leptomeningeal arteries, making them fragile. Typically causes lobar hemorrhages (bleeding in the lobes near the brain surface) in older individuals, often recurrent.
Primary Cause of Spontaneous Subarachnoid Hemorrhage (SAH):
- Rupture of Intracranial Aneurysms: Weakened outpouchings on cerebral arteries rupture, releasing blood directly into the CSF-filled subarachnoid space.
- Saccular ("berry") Aneurysms: Most common type, typically at vessel bifurcations in the Circle of Willis.
- Giant Aneurysms: Large aneurysms (≥25 mm) can rupture or cause mass effect.
- Mycotic Aneurysms: Caused by infection weakening the vessel wall.
- Aneurysm rupture can sometimes lead to associated ICH or IVH in addition to SAH. Re-rupture is a major risk after initial SAH if the aneurysm isn't secured.
Causes Leading to Both ICH and/or SAH:
- Vascular Malformations:
- Arteriovenous Malformations (AVMs): Tangles of abnormal arteries and veins prone to rupture.
- Cavernous Malformations (Cavernomas): Clusters of abnormal, leaky capillaries, usually causing ICH.
- Dural Arteriovenous Fistulas (DAVFs): Abnormal connections between dural arteries and veins/sinuses.
- Hemorrhage into Brain Tumors: Both primary (e.g., glioblastoma) and metastatic tumors can bleed.
- Hemorrhagic Transformation of Ischemic Stroke: Bleeding into an area of prior ischemic stroke, especially after reperfusion therapy or with large embolic infarcts.
- Cerebral Venous Sinus Thrombosis (CVST): Blockage of venous drainage can lead to venous hypertension, causing both ischemic and hemorrhagic infarcts.
Other / Systemic Causes:
- Coagulation Disorders / Anticoagulant Therapy: Conditions like hemophilia, thrombocytopenia, liver disease, disseminated intravascular coagulation (DIC), or therapeutic anticoagulation (warfarin, DOACs) or antiplatelet use increase bleeding risk.
- Hematologic Malignancies: Leukemia, aplastic anemia can cause bleeding due to low platelets or coagulation factor abnormalities.
- Inflammatory/Infectious Conditions: Vasculitis (inflammation of blood vessels), infective endocarditis (leading to mycotic aneurysms), certain types of encephalitis (e.g., herpes simplex encephalitis, acute necrotizing hemorrhagic encephalopathy).
- Substance Abuse: Stimulant use (cocaine, amphetamines) can acutely raise blood pressure and trigger hemorrhage.
- Rare Causes: Bleeding after certain procedures (angiography, neurosurgery), associated with Moyamoya disease, radiation-induced vasculopathy, severe hypoxemia, complications of carotid-cavernous fistula (CCF), certain toxins or venoms.
Note: Migraine headache itself is rarely a direct cause of hemorrhage, although severe hypertensive episodes associated with migraine could potentially trigger a bleed in someone with an underlying vascular vulnerability.
Differential Diagnosis of Spontaneous Intracranial Hemorrhage [1, 2]
| Hemorrhage Type / Cause | Typical Location | Key Features / Diagnostic Clues |
|---|---|---|
| ICH - Hypertensive | Deep: Basal ganglia, thalamus, pons, cerebellum. | History of chronic hypertension. CT shows deep hematoma. |
| ICH - Cerebral Amyloid Angiopathy (CAA) | Lobar (cortical/subcortical). | Elderly patient (>60-65). Often multiple/recurrent lobar bleeds. MRI (GRE/SWI) shows lobar microbleeds, siderosis. |
| SAH - Aneurysmal Rupture | Subarachnoid space (basal cisterns, sulci). May have associated ICH/IVH. | Sudden "thunderclap" headache. CT shows SAH. CTA/DSA identifies aneurysm. |
| Vascular Malformation Rupture (AVM, Cavernoma) | ICH location depends on malformation site. AVMs can also cause SAH/IVH. | Often younger patients. MRI (AVM: flow voids; Cavernoma: "popcorn" + hemosiderin) and/or Angiography (AVM) identify lesion. |
| Hemorrhage into Tumor | Location of tumor (primary or metastasis). | MRI with contrast shows hemorrhage associated with enhancing mass. History of cancer (for mets). |
| Hemorrhagic Transformation of Ischemic Stroke | Within an area of prior ischemic infarction (vascular territory). | Occurs days after ischemic stroke onset. Imaging shows blood within established infarct. |
| Anticoagulant / Coagulopathy Related ICH | Can occur anywhere (deep or lobar). May be larger/expand. | History of anticoagulant use or bleeding disorder. Abnormal coagulation tests (INR, PTT, platelets). |
| Mycotic Aneurysm Rupture | Often distal, peripheral ICH or SAH over convexity. | Associated with infective endocarditis/sepsis. Fever common. Angiography shows distal aneurysm(s). Blood cultures positive. |
| Cerebral Venous Thrombosis (CVT) | Can cause hemorrhagic venous infarcts (often bilateral or not respecting arterial territories). | MRV/CTV confirms sinus/vein thrombosis. MRI shows infarct +/- hemorrhage. |
| Vasculitis | Rare cause. Can cause ICH or ischemic stroke. Often systemic symptoms. | Inflammatory markers. Angiography may show vessel irregularities. Biopsy needed if suspected. |
References
- Ropper AH, Samuels MA, Klein JP, Prasad S. Adams and Victor's Principles of Neurology. 11th ed. McGraw Hill; 2019. Chapter 34: Cerebrovascular Diseases (Sections on Intracerebral Hemorrhage and Subarachnoid Hemorrhage).
- Grotta JC, Albers GW, Broderick JP, et al. Stroke: Pathophysiology, Diagnosis, and Management. 7th ed. Elsevier; 2021. Chapter on Intracerebral Hemorrhage & Chapter on Subarachnoid Hemorrhage.
- Greenberg MS. Handbook of Neurosurgery. 9th ed. Thieme; 2019. Chapter 36: Spontaneous Intracerebral Hemorrhage.
- Osborn AG, Hedlund GL, Salzman KL. Osborn's Brain: Imaging, Pathology, and Anatomy. 2nd ed. Elsevier; 2017. Section on Intracranial Hemorrhage.
See also
- Ischemic stroke, cerebral ischemia
- Vertebrobasilar insufficiency (VBI) with vertigo symptom
- Somatoform autonomic dysfunction
- Dizziness, stuffiness in ear and tinnitus
- Ischemic brain disease:
- Atherosclerotic thrombosis
- Atherothrombotic occlusion of internal carotid artery
- Asymptomatic carotid bifurcation stenosis with noise
- Atherothrombotic occlusion of vertebrobasilar and posterior cerebral arteries
- Atherothrombotic occlusion of posterior cerebral artery
- Atherothrombotic occlusion of vertebral and posterior inferior cerebellar arteries (PICA)
- Atherothrombotic occlusion of basilar artery
- Small-vessel stroke (lacunar infarction)
- Other causes of ischemic stroke (cerebral infarction)
- Cerebral embolism
- Spontaneous intracranial (subarachnoid) and intracerebral hemorrhage:
- Arteriovenous malformations of the brain
- Hypertensive intracerebral hemorrhage
- Cerebral arteries inflammatory diseases (cerebral arteritis)
- Giant intracranial aneurysms
- Other causes of intracerebral hemorrhage
- Lobar intracerebral hemorrhage
- Saccular aneurysm and subarachnoid hemorrhage
- Mycotic intracranial aneurysms
- Repeated cerebral artery aneurysm rupture
- Communicating hydrocephalus after intracerebral hemorrhage with ruptured aneurysm
- Cerebral vasospasm
- Cerebrovascular diseases - ischemic stroke, transient ischemic attack (TIA):
- Transient ischemic attack (TIA)
- Sigmoid sinus suppurative thrombophlebitis with thrombosis