Lobar intracerebral hemorrhage
Lobar Intracerebral Hemorrhage Causes
As hypertension control improves in the population, the relative proportion of intracerebral hemorrhages occurring outside the typical deep hypertensive locations (basal ganglia, thalamus) increases [1]. These hemorrhages, often termed "lobar hemorrhages," typically appear on brain imaging (MRI or CT) as oval or rounded collections of blood primarily located within the subcortical white matter of the cerebral lobes [1, 2]. While chronic hypertension can be a contributing risk factor, especially for Cerebral Amyloid Angiopathy (CAA), it is often *not* the primary underlying cause, and many patients with lobar hemorrhage do not have a history of significant hypertension [1, 3]. Specific underlying structural lesions or conditions are identified in a substantial proportion of cases, including [1, 2]:
- Cerebral Amyloid Angiopathy (CAA): A very common cause, especially in older adults (>60-65 years). It involves the deposition of amyloid protein in the walls of small- to medium-sized arteries in the cortex and leptomeninges, making them prone to rupture [1, 3].
- Structural Vascular Lesions: Such as Arteriovenous Malformations (AVMs) or Cavernous Malformations (cavernomas). These are more frequent causes in younger patients [1, 4].
- Coagulopathy or Anticoagulant Use: Bleeding related to inherited or acquired clotting disorders, or therapeutic anticoagulation (e.g., with warfarin or direct oral anticoagulants) [1, 5].
- Hemorrhage into Brain Tumors: Bleeding occurring within primary brain tumors or, more commonly, metastatic lesions (certain metastases like melanoma, renal cell carcinoma, choriocarcinoma are particularly prone to bleeding) [1, 6].
- Ruptured Saccular Aneurysms: While typically causing subarachnoid hemorrhage, aneurysms (especially those pointing into brain tissue) can occasionally rupture primarily into the brain parenchyma, causing a lobar hemorrhage, although this is less common than the other causes listed above [1].
Frequently, the specific underlying cause of a lobar intracerebral hemorrhage remains unidentified even after comprehensive investigation, including cerebral angiography (such as Digital Subtraction Angiography - DSA), especially if initial imaging does not suggest an obvious structural lesion [1].
In such cases, particularly in individuals older than 60-65 years with strictly lobar hemorrhages (often involving the subcortical white matter), Cerebral Amyloid Angiopathy (CAA) is the most probable underlying etiology [1, 3]. While definitive diagnosis requires pathological examination demonstrating amyloid deposition (which stains positive with Congo red dye under polarized light) in cortical and leptomeningeal vessels post-mortem, a probable clinical diagnosis is often made based on characteristic clinical and imaging features (e.g., the Boston Criteria [7]) [3, 7]. The beta-amyloid protein involved in CAA accumulates specifically in the cerebral vasculature and is distinct from the protein deposition seen in systemic amyloidosis affecting other organs [3].
CAA is a major cause of spontaneous, often recurrent, lobar hemorrhage in the elderly [3]. Patients with CAA may also exhibit other imaging findings like cerebral microbleeds (predominantly in lobar locations), cortical superficial siderosis, and white matter hyperintensities on MRI [2, 3].
Lobar Intracerebral Hemorrhage Symptoms & Diagnosis
While many lobar hemorrhages are relatively small and can cause focal neurological deficits that might mimic the symptoms of an ischemic stroke affecting a specific brain region, larger hemorrhages also occur frequently [1]. These more massive bleeds often lead to significant increases in intracranial pressure, resulting in impaired consciousness (stupor or coma) and extensive neurological deficits related to the involved cerebral lobe(s) [1].
Headache is a common symptom at the onset of lobar hemorrhage, often localized to the general area overlying the bleed (e.g., frontal pain with a frontal lobe hemorrhage, temporal pain with a temporal hemorrhage) [1]. However, the pain can sometimes be diffuse or less clearly localized [1].
Nuchal rigidity (neck stiffness, indicating meningeal irritation) or seizures may occur at the onset of a lobar hemorrhage [1]. Vomiting and altered level of consciousness (ranging from drowsiness to coma) are also frequently observed, particularly with larger bleeds [1]. The neurological deficit typically evolves progressively over minutes to hours as the hematoma expands, which can sometimes help distinguish it clinically from the hyperacute, maximal-at-onset presentation often seen with embolic ischemic stroke, although this distinction is not absolute [1].
The specific clinical neurological syndrome resulting from a lobar hemorrhage depends primarily on the location and size of the hematoma [1]:
- Occipital Lobe Hemorrhage: Typically presents with a contralateral homonymous hemianopia (loss of the visual field on the side opposite the hemorrhage). Larger hemorrhages may cause confusion or altered mental status.
- Temporal Lobe Hemorrhage: If involving the dominant temporal lobe (usually left), symptoms often include receptive aphasia (Wernicke's aphasia - difficulty understanding language). Non-dominant temporal lobe hemorrhages may cause confusion, agitation, or contralateral superior quadrantanopia. Seizures are relatively common with temporal lobe lesions.
- Parietal Lobe Hemorrhage: Often results in contralateral sensory loss (hemianesthesia), neglect of the contralateral side (if in the non-dominant hemisphere), apraxia, or difficulties with spatial awareness. A contralateral inferior quadrantanopia may also occur.
- Frontal Lobe Hemorrhage: Commonly causes contralateral hemiparesis (weakness), particularly affecting the leg more than the arm if located superiorly/medially, or the arm/face more if located laterally. Other potential symptoms include expressive aphasia (Broca's aphasia, if in the dominant frontal lobe), executive dysfunction (problems with planning, judgment), abulia (lack of initiative), or urinary incontinence.
Larger hemorrhages or those extending into adjacent lobes or causing significant edema and mass effect will naturally lead to more widespread and severe neurological deficits, often including impaired consciousness [1].
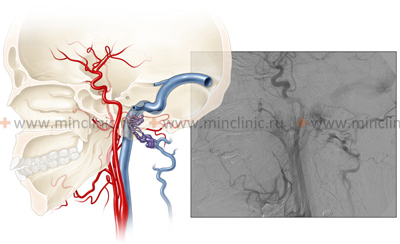
Cerebral angiography is often indicated in patients with lobar hemorrhage to investigate for an underlying vascular cause, such as an Arteriovenous Malformation (AVM) or aneurysm, especially in younger patients or those without clear risk factors like advanced age and hypertension (suggesting Cerebral Amyloid Angiopathy - CAA) [1, 5].
While initial angiography (often CT Angiography - CTA, or sometimes Digital Subtraction Angiography - DSA) may be performed acutely, small vascular malformations can sometimes be obscured by the hematoma and associated mass effect [1, 5]. Therefore, if the initial study is negative but clinical suspicion for an underlying lesion remains high (e.g., based on patient age or hemorrhage characteristics), repeat angiography (typically DSA, the gold standard for detecting subtle malformations) is often recommended [1, 5]. This delayed study is usually performed several weeks to months later (e.g., 2-4 months) after significant hematoma resolution allows for better visualization of the vasculature [1].
Differential Diagnosis of Lobar Intracerebral Hemorrhage [1, 2, 5]
| Cause | Typical Features | Diagnostic Clues / Investigations |
|---|---|---|
| Cerebral Amyloid Angiopathy (CAA) | Most common cause in elderly (>60-65). Strictly lobar location (often subcortical), frequently multiple or recurrent bleeds. May have associated cognitive decline. | MRI (GRE/SWI): Lobar ICH, often multiple lobar microbleeds, cortical superficial siderosis. Meets Boston Criteria clinically. Hypertension less common. |
| Arteriovenous Malformation (AVM) | More common cause in younger adults (<40-50). Hemorrhage often parenchymal +/- IVH/SAH. May have history of seizures or headache. | CTA/MRA/DSA: Identifies nidus, feeding arteries, draining veins. MRI may show flow voids. |
| Cavernous Malformation (Cavernoma) | Can occur at any age. Often smaller bleeds, may be recurrent. Can present with seizures or focal deficits without overt hemorrhage. Familial forms exist. | MRI: Characteristic "popcorn" lesion with mixed signal, hemosiderin rim. Angiographically occult. |
| Hemorrhage into Tumor (Primary or Metastatic) | Bleeding within a pre-existing mass. May have prior progressive neurological symptoms. Certain tumor types predispose (melanoma, RCC, chorio, GBM). | MRI with contrast: Shows hematoma associated with enhancing tumor mass, often significant surrounding edema. History of primary cancer (for mets). |
| Anticoagulant-Associated ICH | Lobar location possible (though deep also common). Hematoma may be larger or expand more. | History of anticoagulant use. Elevated INR or relevant drug assay. Requires reversal. |
| Coagulopathy / Hematologic Disorder | Can occur anywhere, including lobar. May be multiple. Often associated systemic bleeding signs. | Abnormal blood counts/coagulation studies. Evidence of underlying disorder (liver disease, thrombocytopenia, leukemia). |
| Ruptured Saccular Aneurysm | Less common cause of primary lobar ICH. Usually causes SAH. Can cause lobar bleed if aneurysm points into parenchyma or ruptures laterally. Sudden severe headache typical. | CT shows SAH +/- ICH. CTA/DSA identifies aneurysm. |
| Hemorrhagic Transformation of Ischemic Stroke | Bleeding within area of prior infarct. Follows ischemic stroke symptoms. | Imaging shows blood within established infarct territory. |
| Septic Embolism / Mycotic Aneurysm Rupture | Associated with infective endocarditis. Fever, signs of infection. Hemorrhage can occur from septic infarct or rupture of infected aneurysm. | Blood cultures. Echocardiogram. Angiography may show mycotic aneurysm(s). |
| Vasculitis | Rare cause. May cause hemorrhage or infarcts. Often systemic symptoms. | Inflammatory markers. Angiography may show vessel irregularities. Biopsy may be needed. |
Lobar intracerebral hemorrhage treatment
The optimal treatment strategy for a lobar intracerebral hemorrhage (ICH) depends on several factors, including the patient's clinical condition (level of consciousness, neurological deficits), the size and location of the hematoma, evidence of ongoing bleeding or expansion, and the underlying cause, if identified (e.g., AVM, tumor, anticoagulation) [1, 5].
The role of surgical hematoma evacuation for spontaneous lobar ICH remains debated, and decisions are individualized [5, 8]. For patients who are conscious or only mildly drowsy with smaller hematomas not causing significant mass effect, conservative medical management is often the primary approach [5]. Conservative management focuses on critical care principles including strict blood pressure control (targeting specific goals, often systolic <140 mmHg or <160 mmHg acutely), reversal of any coagulopathy (e.g., stopping anticoagulants and administering reversal agents), monitoring for and managing elevated intracranial pressure (ICP) if it develops (using measures like head elevation, osmotic therapy with mannitol or hypertonic saline, and potentially cerebrospinal fluid drainage via an external ventricular drain), seizure prophylaxis in select cases, DVT prophylaxis, and general supportive care [5]. Notably, corticosteroids are *not* beneficial and are generally contraindicated in acute ICH [5].
Surgical intervention (typically craniotomy with hematoma evacuation) is more likely to be considered for patients with larger lobar hemorrhages causing significant mass effect and neurological deterioration (e.g., progression to stupor or coma), especially if the hematoma is located superficially and is considered surgically accessible [5, 8]. Urgent surgery may be life-saving in cases with clinical signs of brain herniation that are rapidly progressive or unresponsive to initial medical ICP management [5]. The primary goal of surgery in these situations is brain decompression by removing the blood clot, thereby alleviating mass effect and potentially improving neurological outcome [8].
References
- Ropper AH, Samuels MA, Klein JP, Prasad S. Adams and Victor's Principles of Neurology. 11th ed. McGraw Hill; 2019. Chapter 34: Cerebrovascular Diseases (Section on Intracerebral Hemorrhage).
- Grotta JC, Albers GW, Broderick JP, et al. Stroke: Pathophysiology, Diagnosis, and Management. 7th ed. Elsevier; 2021. Chapter on Intracerebral Hemorrhage.
- Charidimou A, Gang Q, Werring DJ. Sporadic cerebral amyloid angiopathy revisited: recent insights into pathophysiology and clinical spectrum. J Neurol Neurosurg Psychiatry. 2012 Feb;83(2):124-37.
- Greenberg MS. Handbook of Neurosurgery. 9th ed. Thieme; 2019. Chapter 38: Arteriovenous Malformations & Chapter 39: Cavernous Malformations.
- Hemphill JC 3rd, Greenberg SM, Anderson CS, et al; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015 Jul;46(7):2032-60.
- Greenberg MS. Handbook of Neurosurgery. 9th ed. Thieme; 2019. Chapter 20: Brain Tumors (sections on specific tumor types and complications like hemorrhage).
- Knudsen KA, Rosand J, Karluk D, Greenberg SM. Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria. Neurology. 2001 Aug 14;57(3):560-2.
- Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM; STICH II Investigators. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013 Aug 3;382(9890):397-408. (Example surgical trial for lobar ICH).
See also
- Ischemic stroke, cerebral ischemia
- Vertebrobasilar insufficiency (VBI) with vertigo symptom
- Somatoform autonomic dysfunction
- Dizziness, stuffiness in ear and tinnitus
- Ischemic brain disease:
- Atherosclerotic thrombosis
- Atherothrombotic occlusion of internal carotid artery
- Asymptomatic carotid bifurcation stenosis with noise
- Atherothrombotic occlusion of vertebrobasilar and posterior cerebral arteries
- Atherothrombotic occlusion of posterior cerebral artery
- Atherothrombotic occlusion of vertebral and posterior inferior cerebellar arteries (PICA)
- Atherothrombotic occlusion of basilar artery
- Small-vessel stroke (lacunar infarction)
- Other causes of ischemic stroke (cerebral infarction)
- Cerebral embolism
- Spontaneous intracranial (subarachnoid) and intracerebral hemorrhage:
- Arteriovenous malformations of the brain
- Hypertensive intracerebral hemorrhage
- Cerebral arteries inflammatory diseases (cerebral arteritis)
- Giant intracranial aneurysms
- Other causes of intracerebral hemorrhage
- Lobar intracerebral hemorrhage
- Saccular aneurysm and subarachnoid hemorrhage
- Mycotic intracranial aneurysms
- Repeated cerebral artery aneurysm rupture
- Communicating hydrocephalus after intracerebral hemorrhage with ruptured aneurysm
- Cerebral vasospasm
- Cerebrovascular diseases - ischemic stroke, transient ischemic attack (TIA):
- Transient ischemic attack (TIA)
- Sigmoid sinus suppurative thrombophlebitis with thrombosis