Digital Subtraction Angiography (DSA)
- Digital Subtraction Angiography (DSA) in Cerebrovascular Disease: Overview
- What is Digital Subtraction Angiography (DSA)?
- Indications for DSA in Cerebrovascular Disease
- The DSA Procedure: A Step-by-Step Guide
- Advantages of DSA
- Disadvantages and Potential Risks of DSA
- Comparison with Alternative Vascular Imaging Techniques (CTA & MRA)
- The Evolving Role of DSA in Modern Neuroradiology
- When is DSA Recommended?
- References
Digital Subtraction Angiography (DSA) in Cerebrovascular Disease: The Gold Standard for Detailed Vascular Imaging
Cerebrovascular diseases represent a diverse group of conditions that affect the blood vessels responsible for supplying blood to the brain. These conditions include, but are not limited to, stroke (both ischemic, caused by blockages, and hemorrhagic, caused by bleeding), cerebral aneurysms (abnormal outpouchings of arterial walls), arteriovenous malformations (AVMs) and fistulas (abnormal connections between arteries and veins), stenosis (narrowing of arteries), and vasculitis (inflammation of blood vessel walls). The precise diagnosis and detailed characterization of these vascular abnormalities are paramount for formulating effective treatment strategies and improving patient outcomes. While non-invasive imaging techniques such as Computed Tomography Angiography (CTA) and Magnetic Resonance Angiography (MRA) have made remarkable advancements and play crucial roles in initial assessment, Digital Subtraction Angiography (DSA) continues to be regarded as the gold standard for providing the most detailed, high-resolution, and dynamic visualization of the brain's intricate vascular network.
What is Digital Subtraction Angiography (DSA)?
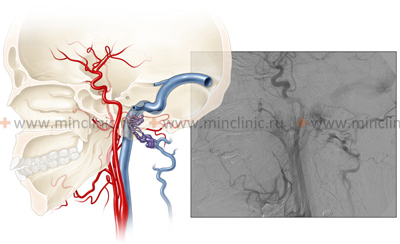
Digital Subtraction Angiography (DSA) is a minimally invasive diagnostic imaging technique that provides high-resolution, real-time visualization of blood vessels. It is a type of fluoroscopy, using X-rays to obtain dynamic images.
The Principle of Subtraction
The core principle of DSA involves "subtracting" background structures to highlight the contrast-filled vessels:
- Mask Image Acquisition: An initial X-ray image, known as a "mask image," is captured of the anatomical region of interest (e.g., head and neck) before any contrast material is introduced. This image contains bone and soft tissue structures.
- Catheterization and Contrast Injection: A thin, flexible tube called a catheter is inserted, typically into a peripheral artery (most commonly the femoral artery in the groin, or sometimes the radial artery in the wrist). Under continuous X-ray guidance (fluoroscopy), the catheter is carefully navigated through the arterial system to the specific arteries supplying the brain (e.g., internal carotid arteries, vertebral arteries). Once in position, an iodine-based contrast material (a dye that is opaque to X-rays) is injected through the catheter directly into these targeted arteries.
- Serial Image Acquisition: As the contrast material flows through the cerebral arteries, capillaries, and veins, a rapid series of X-ray images are taken.
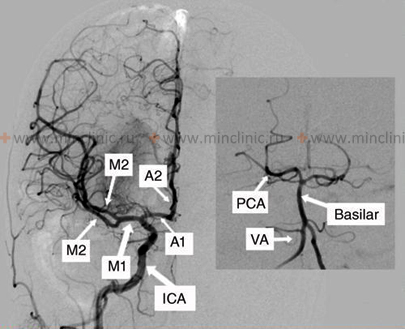
- Digital Subtraction: Specialized computer software then digitally subtracts the initial mask image (containing bone and soft tissue) from the subsequent images that contain the contrast-filled blood vessels. This subtraction process effectively removes the overlying static structures like the skull, leaving a clear, unobstructed, high-resolution image exclusively of the blood vessels.
This technique allows for exceptional detail in visualizing the vascular lumen, identifying abnormalities, and assessing blood flow dynamics.
Indications for DSA in Cerebrovascular Disease
DSA provides unparalleled detail regarding the structure and flow dynamics of cerebral blood vessels, making it invaluable for diagnosing, planning treatment for, and sometimes directly treating various cerebrovascular conditions:
- Cerebral Aneurysms: DSA is considered the most accurate method to precisely define the size, shape (saccular, fusiform), location, and neck characteristics (width, orientation) of brain aneurysms. This detailed information is critical for determining the optimal treatment strategy, whether it be surgical clipping or endovascular techniques like coiling or flow diversion, especially following a subarachnoid hemorrhage (SAH). DSA can also detect very small or blister-like aneurysms that might be missed by CTA or MRA.
- Arteriovenous Malformations (AVMs) and Arteriovenous Fistulas (AVFs): These represent complex tangles of abnormal blood vessels or direct, high-flow connections between arteries and veins, respectively. DSA provides essential dynamic flow information, clearly visualizing feeding arteries, the AVM nidus (core of the malformation), and the pattern of draining veins. This is crucial for planning treatment options such as embolization (blocking off abnormal vessels), surgical resection, or stereotactic radiosurgery.
- Arterial Stenosis (Narrowing) and Occlusion (Blockage): While CTA and MRA are often sufficient for initial assessment, DSA offers the highest accuracy for quantifying the degree of arterial narrowing and confirming complete blockage, particularly for smaller intracranial vessels or when non-invasive imaging results are equivocal or inconclusive. This detailed assessment is important when considering interventions like angioplasty or stenting for conditions such as atherosclerosis, Moyamoya disease, arterial dissection, or fibromuscular dysplasia.
- Vasculitis (Cerebral Arteritis): Inflammation of the central nervous system (CNS) blood vessels can cause subtle irregularities, beading, segmental narrowing, or "string of pearls" appearance of arteries. DSA's high spatial resolution can sometimes detect these characteristic changes more clearly than non-invasive methods, aiding in this often challenging diagnosis. However, a definitive diagnosis of CNS vasculitis may still require brain or leptomeningeal biopsy.
- Acute Ischemic Stroke: While CT/CTA and MRI/MRA are the primary initial diagnostic tools for acute stroke to identify hemorrhage or early ischemic changes, DSA plays an essential role during endovascular treatment, specifically mechanical thrombectomy. It guides the precise placement of stent retrievers or aspiration catheters to remove the occluding clot from large cerebral arteries and allows real-time assessment of blood flow restoration (reperfusion).
- Pre-operative / Pre-interventional Planning: Before complex neurosurgical procedures (e.g., resection of tumors located near major arteries, aneurysm clipping, cerebral bypass surgery) or prior to other endovascular interventions, DSA provides the detailed vascular "roadmap" that surgeons and interventional neuroradiologists require for safe and effective treatment.
- Evaluation of Dural Arteriovenous Fistulas (DAVFs).
- Assessment of Cerebral Venous Sinus Thrombosis (CVST): Though MRV/CTV are primary, DSA can be used in select complex cases or for intervention.
- Spinal Vascular Malformations.
The DSA Procedure: A Step-by-Step Guide
Digital Subtraction Angiography is a specialized procedure performed by interventional neuroradiologists or neurosurgeons in a dedicated angiography suite equipped with fluoroscopy and digital imaging systems.
Patient Preparation
- Fasting: Patients are typically required to fast for several hours (usually 4-6 hours) before the procedure to reduce the risk of aspiration if sedation or anesthesia is needed.
- Medication Review: A thorough review of current medications is conducted. Blood-thinning medications (anticoagulants like warfarin, heparin; antiplatelet drugs like aspirin, clopidogrel) may need to be temporarily stopped or adjusted. Medications for diabetes (e.g., metformin) may also require specific instructions.
- Allergy Assessment: History of allergies, especially to iodine or contrast materials, is carefully assessed. Pre-medication with corticosteroids or antihistamines may be given if there's a known mild allergy.
- Blood Tests: Baseline blood tests are performed to check kidney function (creatinine, eGFR), as the contrast dye is excreted by the kidneys, and coagulation status (PT/INR, PTT, platelet count).
- Informed Consent: The procedure, its benefits, risks, and alternatives are explained to the patient, and informed consent is obtained.
- Pre-Procedure Hydration: Sometimes intravenous fluids are started to ensure good hydration, which can help protect the kidneys from contrast-induced nephropathy.
During the Procedure
- Positioning and Monitoring: The patient lies flat on an X-ray table. Vital signs (heart rate, blood pressure, oxygen saturation) are continuously monitored.
- Sedation/Anesthesia: Depending on the patient's condition and the complexity of the procedure, conscious sedation (making the patient drowsy but responsive) or general anesthesia may be administered.
- Access Site Preparation: The catheter insertion site, most commonly the femoral artery in the groin, is cleaned with an antiseptic solution and draped with sterile towels. Local anesthetic is injected to numb the skin and deeper tissues.
- Catheter Insertion and Navigation: A small needle is used to puncture the artery, followed by the insertion of a guidewire and then a sheath (a short tube that provides access). The angiography catheter is then inserted through the sheath and carefully guided under fluoroscopic (real-time X-ray) visualization through the aorta and into the specific arteries supplying the brain (e.g., carotid or vertebral arteries).
- Contrast Injection and Imaging: Once the catheter is in the desired location, small amounts of iodinated contrast material are injected. As the contrast flows through the blood vessels, a rapid sequence of X-ray images is acquired using the DSA technique. Patients may experience a temporary warm or flushing sensation, a metallic taste, or a feeling of needing to urinate during contrast injection. It is crucial for the patient to remain very still during image acquisition to ensure high-quality images. Multiple injections and imaging runs may be performed to visualize different vessels or views.
The duration of the diagnostic DSA procedure can vary from about 30 minutes to 2-3 hours, depending on the complexity and the number of vessels being examined. If an endovascular treatment is performed concurrently, the procedure will be longer.
Post-Procedure Care and Recovery
- Catheter Removal and Hemostasis: After the procedure, the catheter and sheath are removed. Firm pressure is applied to the arterial puncture site for 10-20 minutes to prevent bleeding, followed by a pressure dressing or closure device.
- Bed Rest: The patient is typically required to lie flat on bed rest for several hours (usually 4-6 hours, or longer if a closure device is not used) to minimize the risk of bleeding or hematoma formation at the puncture site. The leg or arm used for access must be kept straight.
- Monitoring: Vital signs and the puncture site are regularly monitored for any signs of bleeding, swelling, or changes in circulation to the limb.
- Hydration: Patients are encouraged to drink plenty of fluids (or receive IV fluids) to help flush the contrast dye from their system and protect kidney function.
- Discharge: If the DSA was purely diagnostic and uneventful, patients may be discharged the same day or after an overnight observation period, depending on institutional protocols and individual factors. Instructions are given regarding care of the puncture site, activity restrictions, and when to seek medical attention for any complications.
Advantages of DSA
- Highest Spatial Resolution: DSA provides the most detailed anatomical images of blood vessels, allowing for precise visualization of small vessel abnormalities, aneurysm morphology, and the degree of stenosis.
- Excellent Temporal Resolution: It allows for real-time visualization of blood flow dynamics, including arterial, capillary, and venous phases of circulation. This is crucial for understanding AVMs, fistulas, and collateral flow patterns.
- Gold Standard for Diagnosis: For many cerebrovascular conditions, particularly aneurysms and AVMs, DSA is considered the reference standard against which other vascular imaging techniques are often compared.
- Therapeutic Capability: A significant advantage is that DSA allows for immediate endovascular treatment (e.g., aneurysm coiling, AVM embolization, angioplasty and stenting, mechanical thrombectomy for stroke) to be performed during the same session if an abnormality requiring intervention is identified. This "see and treat" capability can be life-saving in acute situations.
Disadvantages and Potential Risks of DSA
Despite its significant benefits, DSA is an invasive procedure and, as such, carries potential risks, although serious complications are relatively uncommon when performed by experienced teams.
- Neurological Complications (Stroke): This is the most significant risk, although generally low for purely diagnostic procedures (often quoted in the range of 0.5% to 1%, but can be higher for interventional procedures or in patients with severe underlying vascular disease). A stroke can be caused by dislodgement of atherosclerotic plaque during catheter manipulation, formation of a blood clot on the catheter or guidewire that then travels to the brain (embolism), or, rarely, dissection (tear) of an artery wall.
- Access Site Complications:
- Bleeding or Hematoma: Bruising, swelling, or a collection of blood at the catheter insertion site (groin or wrist). Large hematomas can sometimes compress nerves or require drainage.
- Pseudoaneurysm: A contained rupture of the arterial wall at the puncture site, forming a pulsating sac.
- Arteriovenous Fistula: An abnormal connection between the punctured artery and an adjacent vein.
- Infection: Rare at the puncture site.
- Vessel Damage: Injury, dissection, or perforation of the artery accessed or navigated by the catheter.
- Contrast Material Reactions:
- Allergic Reactions: Ranging from mild (itching, hives) to severe anaphylaxis (rare). Patients with a history of contrast allergy may require premedication.
- Contrast-Induced Nephropathy (CIN): Potential for temporary or, rarely, permanent kidney damage from the contrast dye, especially in patients with pre-existing kidney disease, diabetes, or dehydration. Adequate hydration before and after the procedure helps mitigate this risk.
- Radiation Exposure: DSA involves the use of X-rays, so there is some radiation exposure to the patient and medical staff. Doses are generally kept as low as reasonably achievable (ALARA principles).
- Other Rare Complications: Nerve injury near the puncture site, vasospasm, air embolism.
The overall risk is weighed against the diagnostic and therapeutic benefits for each individual patient.
Comparison with Alternative Vascular Imaging Techniques (CTA & MRA)
Non-invasive techniques like CTA and MRA are often used as initial screening or diagnostic tools for cerebrovascular disease. DSA is typically reserved for situations where these methods are inconclusive or when intervention is planned.
| Feature | Digital Subtraction Angiography (DSA) | Magnetic Resonance Angiography (MRA) | Computed Tomography Angiography (CTA) |
|---|---|---|---|
| Basic Principle | X-ray imaging with digital subtraction of pre-contrast images from post-contrast images. | Utilizes magnetic fields and radio waves to generate images of blood vessels. Can detect flow or use contrast. | X-ray computed tomography combined with intravenous (IV) contrast injection to visualize blood vessels. |
| Invasiveness | Invasive (requires arterial catheterization). | Generally non-invasive (IV contrast may be used, but no arterial access needed). Non-contrast techniques exist. | Minimally invasive (requires IV contrast injection). |
| Contrast Agent | Iodinated contrast medium (injected intra-arterially). | Gadolinium-based contrast agent (GBCA) often used (IV), but non-contrast techniques (e.g., Time-of-Flight) are common. | Iodinated contrast medium (injected intravenously). |
| Contrast Risks |
|
|
|
| Ionizing Radiation | Yes (Significant dose, variable depending on procedure complexity). | No. | Yes (Significant dose, though modern techniques aim to reduce it). |
| Image Quality / Resolution | Highest spatial and temporal resolution. Considered the "gold standard" for vessel lumen visualization. | Good resolution, particularly for larger vessels. Can be affected by flow artifacts or patient motion. Excellent soft tissue contrast. | Excellent spatial resolution, particularly with multi-detector CT (MDCT). Good for vessel wall and surrounding structures. |
| Procedure Duration | Longer (typically 30 mins to several hours, especially if intervention is performed). | Moderate (typically 20-60 minutes). | Fast (Image acquisition takes seconds to minutes; total room time longer). |
| Real-time Capability | Yes, allows for real-time visualization and intervention. | No real-time capability in the same sense as DSA. | No real-time capability. |
| Patient Contraindications |
|
|
|
| Therapeutic Potential | Yes (Primary advantage - allows for simultaneous diagnosis and endovascular treatment like angioplasty, stenting, embolization). | No. | No. |
| Cost | High (due to invasiveness, equipment, personnel, potential for intervention). | High (due to scanner cost and scan time). | Moderate to High (less than DSA typically, comparable/less than MRA). |
| Common Applications |
|
|
|
| Advantages |
|
|
|
| Disadvantages |
|
|
|
The Evolving Role of DSA in Modern Neuroradiology
With the continuous advancements and improved image quality of non-invasive techniques like CTA and MRA, the role of purely diagnostic DSA has become more selective. In many clinical pathways, CTA or MRA are employed as the initial imaging modalities for screening and primary diagnosis of cerebrovascular diseases.
DSA is now typically reserved for:
- Problem Solving: Cases where non-invasive imaging results are unclear, equivocal, or insufficient for definitive diagnosis or treatment planning.
- Detailed Characterization of Complex Lesions: For intricate anatomical details of aneurysms (especially small or complex ones), AVMs, or dural arteriovenous fistulas prior to determining the best treatment approach.
- Evaluation of Specific Conditions: Assessing conditions where fine vascular detail or dynamic flow information is critical (e.g., suspected cerebral vasculitis, evaluating collateral circulation, detailed assessment of dural fistulas).
- Guiding and Performing Endovascular Interventions: This is now a primary role for DSA. It is an essential component of minimally invasive treatments such as aneurysm coiling/flow diversion, AVM/AVF embolization, carotid or intracranial artery stenting, and mechanical thrombectomy for acute ischemic stroke.
- Post-Treatment Follow-Up: In some cases, DSA is used to assess the results of endovascular or surgical treatments (e.g., completeness of aneurysm occlusion, AVM obliteration).
When is DSA Recommended?
The decision to proceed with Digital Subtraction Angiography is made carefully by a multidisciplinary team (including neurologists, neurosurgeons, and interventional neuroradiologists), weighing the substantial diagnostic and potential therapeutic benefits against the inherent risks of an invasive procedure. It is typically recommended when less invasive tests (CTA/MRA) do not provide sufficient information for a definitive diagnosis or for planning complex treatments, or when an endovascular intervention is anticipated. DSA remains an indispensable tool in the armamentarium for the comprehensive diagnosis and management of a wide spectrum of cerebrovascular diseases, valued for its unparalleled anatomical detail and real-time assessment of blood flow, especially in the context of guiding minimally invasive therapies.
References
- Osborn AG, Salzman KL, Katzman G, et al. Diagnostic Cerebral Angiography. 2nd ed. Lippincott Williams & Wilkins; 1999.
- Morris PP. Practical Neuroangiography. 3rd ed. Lippincott Williams & Wilkins; 2016.
- Brinjikji W, Cloft HJ, Kallmes DF. Risks of diagnostic cerebral angiography performed by training and attending physicians. AJNR Am J Neuroradiol. 2009 Sep;30(8):1527-30.
- Willinsky RA, Taylor SM, TerBrugge K, Farb RI, Tomlinson G, Montanera W. Neurologic complications of cerebral angiography: a prospective study of 2,899 procedures and review of the literature. Radiology. 2003 May;227(2):522-8.
- Fiehler J, Sychra V, Heiland S, et al. Digital subtraction angiography: still the gold standard? Radiologe. 2009 Jan;49(1):34-40. (German)
- American Heart Association/American Stroke Association. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke. Stroke. 2019;50(12):e344-e418. (Context for DSA in thrombectomy)
- Connors JJ 3rd, Sacks D, Furlan AJ, et al. Training, competency, and credentialing standards for diagnostic cervicocerebral angiography, carotid stenting, and cerebrovascular intervention: a joint statement from the American Academy of Neurology, the American Association of Neurological Surgeons, the American Society of Interventional and Therapeutic Neuroradiology, the American Society of Neuroradiology, the Congress of Neurological Surgeons, the AANS/CNS Cerebrovascular Section, and the Society of Interventional Radiology. J Vasc Interv Radiol. 2005 Jan;16(1):1-11.
- Cloft HJ, Kallmes DF, Linfante I, et al. Risks of cerebral angiography in patients with subarachnoid hemorrhage. Stroke. 2000 Aug;31(8):1882-4.