Cerebrovascular arteriovenous malformations (AVMs)
Morphology of Cerebrovascular Arteriovenous Malformations (AVMs)
Note: While the terms angioma or hemangioma are sometimes used colloquially in relation to AVMs, Arteriovenous Malformation (AVM) is the specific term for the type of vascular malformation described here, characterized by direct artery-to-vein connections. True hemangiomas are typically benign vascular tumors, distinct from AVMs [1].
Certain genetic disorders, like Hereditary Hemorrhagic Telangiectasia (HHT), also known as Osler-Weber-Rendu disease, are characterized by the formation of multiple vascular malformations, including arteriovenous malformations (AVMs) – abnormal tangles of blood vessels lacking a proper capillary bed [2, 3].
In HHT, these malformations can manifest externally as telangiectases (small, dilated blood vessels visible as red markings on the skin). Importantly, AVMs associated with HHT or arising sporadically can also develop internally, particularly in the brain, spinal cord, lungs, and other organs [2, 3]. Rupture of these fragile AVMs is a major risk, potentially leading to significant hemorrhage (bleeding) into surrounding tissues.
HHT follows an autosomal dominant inheritance pattern, meaning an individual with one affected parent has a 50% chance of inheriting the predisposition to form these vascular anomalies [2]. This disorder affects a significant number of people globally (estimated over 1.4 million) and is frequently misdiagnosed or underdiagnosed due to the wide variability in its clinical presentations [3].
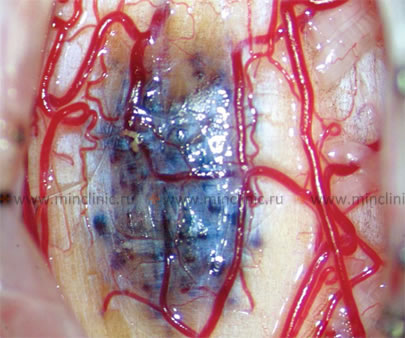
Cerebral **Arteriovenous Malformations (AVMs)** are complex, abnormal vascular structures representing developmental anomalies [1, 4]. They are fundamentally defined by the presence of direct connections (shunts or fistulas) between feeding arteries and draining veins, bypassing the normal intervening capillary network [1, 5]. This abnormal connection is often referred to as the AVM "nidus." A key characteristic of AVMs is the tendency for progressive dilation (widening) and elongation of the vessels involved in these arteriovenous connections over time [1].
AVMs vary greatly in size. They can range from tiny lesions, just a few millimeters across, located deep within the cerebral cortex or white matter, to extensive, convoluted networks forming large arteriovenous shunts [1, 5]. These high-flow shunts between cerebral arteries and veins can sometimes place a significant strain on the heart, potentially increasing cardiac output [1]. Typically, one or more enlarged, hypertrophied arterial 'feeder' vessels supply the AVM nidus, often penetrating the cerebral cortex before transitioning into the tangled network of thin-walled, abnormal vessels within the nidus [1, 5]. Subsequently, this vascular network drains rapidly into enlarged, often pulsating veins that carry highly oxygenated, arterialized blood (due to the direct shunting) [1, 5].
Histologically, the blood vessels composing the AVM nidus (the tangle between the feeding arteries and draining veins) are typically abnormal. They are pathologically thinned and lack the distinct structural layers (like the muscular tunica media) found in normal arteries and veins, making them prone to rupture [1, 5].
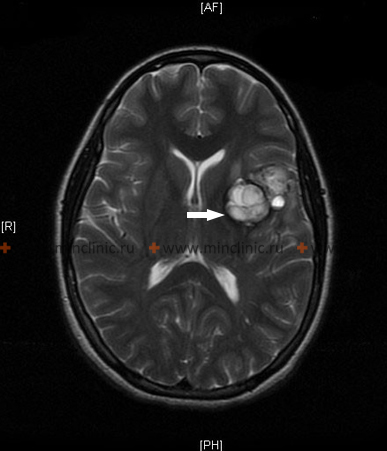
Arteriovenous malformations can occur anywhere within the central nervous system, including the cerebral hemispheres, brainstem, and spinal cord [1, 6]. However, larger AVMs are statistically more frequent in the posterior regions of the cerebral hemispheres [1]. They often present radiologically as wedge-shaped lesions with the base towards the cortex and the apex pointing towards the deeper white matter or the ventricular system [5, 7].
AVMs are slightly more prevalent in men than women (approximate 2:1 ratio) and occasionally exhibit familial clustering, suggesting a genetic predisposition in some cases beyond known syndromes like HHT [1, 4]. Although this vascular anomaly is congenital (present from birth), patients most commonly become symptomatic and present for medical attention between the ages of 10 and 30 years, though initial presentation can occur even after 50 years of age (often due to hemorrhage, seizures, or headaches) [1, 4].
Cerebrovascular Arteriovenous Malformations (AVMs): Clinical Presentation and Diagnosis
Cerebral arteriovenous malformations (AVMs) are significant vascular anomalies that can become symptomatic in various ways. Common modes of clinical presentation include [1, 4]:
- Incidental Finding: Discovered during brain imaging for unrelated reasons in asymptomatic patients (approx. 15% of cases).
- Seizures: Focal or generalized seizures occur as the initial symptom in about 20-30% of patients.
- Headaches: Chronic or acute headaches, sometimes mimicking migraines.
- Ischemic Events: Neurological deficits caused by the "vascular steal" phenomenon, where the high-flow AVM diverts blood away from adjacent normal brain tissue (relatively uncommon presentation).
- Hemorrhage: Bleeding (intraparenchymal, subarachnoid, or intraventricular) is the most common and dangerous presentation (approx. 50-65% of symptomatic cases). The annual risk of AVM rupture is estimated at 2-4%, and the risk of re-rupture after an initial bleed is higher, especially in the first year [1, 8].
Elaborating on the primary clinical manifestations [1]:
- Headache: May present as hemicrania (affecting one side of the head), can be pulsating (like migraine) or dull and diffuse. In some instances, headache associated with transient neurological deficits like hemiplegia can resemble hemiplegic migraine.
- Seizures: Patients may experience focal seizures (originating in one brain area) which can sometimes spread and become generalized tonic-clonic seizures. Seizures are a presenting symptom in roughly 30% of individuals with AVMs and are often well-controlled with standard anticonvulsant medications.
- Hemorrhage: Occurs as the presenting symptom in approximately 50% (or more) of patients with AVMs [1, 4]. The bleeding is most commonly *intraparenchymal* (within the brain tissue itself) rather than purely *subarachnoid* (in the space surrounding the brain) [1]. Because AVM hemorrhages often do not pool significantly in the basal cisterns (fluid spaces at the base of the brain) like ruptured aneurysms sometimes do, clinically significant cerebral vasospasm (narrowing of arteries due to blood irritation) is relatively rare after AVM rupture [1, 9].
The risk of AVM *re-rupture* shortly after an initial bleed (e.g., within the first few weeks) is generally considered lower than the early re-rupture risk associated with unsecured saccular aneurysms [1]. Consequently, antifibrinolytic agents (medications to prevent clot breakdown) are typically not used for AVM hemorrhage [1]. While hemorrhages can be massive and potentially cause sudden death, they can also be small (e.g., hematoma up to 1 cm), producing only mild or transient focal symptoms, and some patients may recover with minimal or no residual neurological deficits [1].
- Ischemia (Vascular Steal): In rare instances, particularly with very large, high-flow AVMs, the malformation can cause a "steal" effect [1, 5]. It shunts so much blood directly from arteries to veins that it deprives adjacent, normal brain tissue of adequate blood supply, leading to ischemic symptoms in those areas. This steal phenomenon is more often considered with large AVMs involving major vascular territories, such as those bridging the middle cerebral–posterior cerebral artery or middle cerebral–anterior cerebral artery distributions, often extending from the cortical surface deep towards the ventricular system [1].
- Other Manifestations: Involvement of the deep venous system, particularly the vein of Galen, in an AVM (leading to a "Vein of Galen Malformation" - a specific AVM subtype) can obstruct cerebrospinal fluid pathways and lead to hydrocephalus (fluid buildup in the brain) [1, 10]. For large, superficial AVMs, a systolic and diastolic bruit (vascular murmur) may sometimes be detected with a stethoscope over the patient’s orbit, forehead, or neck, occasionally accompanied by a noticeably forceful carotid pulse on palpation [1].
Distinguishing AVM rupture from other causes of intracranial hemorrhage can sometimes be aided by clinical clues. At the moment of AVM rupture, systemic arterial blood pressure is often normal (unlike some hypertensive hemorrhages), which might raise suspicion for an underlying vascular malformation or aneurysm [1]. Compared to a ruptured saccular aneurysm, severe headache may be less prominent or frequent during the initial phase of AVM rupture, although nausea and vomiting remain common symptoms across most types of acute intracranial hemorrhage [1].
Differential Diagnosis of Intracranial Hemorrhage / Lesions Mimicking AVM [1, 7, 11]
| Condition | Key Features / Distinguishing Points | Typical Imaging Findings |
|---|---|---|
| Arteriovenous Malformation (AVM) Hemorrhage | Often younger patients (10-40 yrs). Hemorrhage typically intraparenchymal +/- intraventricular/subarachnoid. Seizures, headache common prior. BP often normal at rupture. | CT: Acute hemorrhage. CTA/MRA/DSA: Shows tangled nidus, enlarged feeding arteries, early draining veins. MRI: Flow voids, hemosiderin (old bleeds). |
| Ruptured Saccular Aneurysm | Sudden "thunderclap" headache. SAH predominantly in basal cisterns. Loss of consciousness, meningismus common. Often associated with HTN, smoking. | CT: Diffuse SAH. CTA/DSA: Identifies saccular outpouching, usually at vessel bifurcation. Vasospasm common later. |
| Hypertensive Intracerebral Hemorrhage (ICH) | Older adults typically. History of hypertension crucial. Hemorrhage often in characteristic locations (basal ganglia, thalamus, pons, cerebellum). Often presents with focal deficit, decreased LOC. | CT: Hyperdense hematoma in typical location. No underlying vascular malformation usually seen on subsequent CTA/MRA/DSA (unless secondary cause). |
| Cavernous Malformation (Cavernoma) Hemorrhage | Can present with hemorrhage (often smaller, contained), seizures, or focal deficits. Bleeds less catastrophic than AVM/aneurysm. Familial forms exist. | MRI: Characteristic "popcorn" lesion with mixed signal intensities (blood products of different ages) surrounded by hemosiderin rim (T2 dark). Usually angiographically occult (not seen on DSA). |
| Hemorrhagic Tumor (Primary or Metastatic) | Hemorrhage occurs within a pre-existing tumor (e.g., GBM, melanoma, RCC, choriocarcinoma metastases). May have history of progressive symptoms before bleed. | CT: Intraparenchymal hematoma. MRI with contrast: Shows underlying enhancing tumor mass associated with the hemorrhage. |
| Dural Arteriovenous Fistula (DAVF) | Acquired shunt within dural leaflets. Can present with pulsatile tinnitus, hemorrhage (ICH or SAH), seizures, focal deficits, venous hypertension symptoms. | MRI/MRA may show dilated cortical veins. DSA is gold standard, shows fistula site within dura, pattern of venous drainage (critical for risk assessment). |
| Hemorrhagic Ischemic Stroke | Hemorrhagic transformation occurs within an area of prior ischemic infarction, usually days after initial stroke. | CT/MRI: Shows hemorrhage within an area consistent with recent infarction (often wedge-shaped, vascular territory). |
| Cerebral Amyloid Angiopathy (CAA) | Causes lobar ICH (often multiple, recurrent) in elderly. Associated with cognitive decline. Bleeding often superficial (cortical/subcortical). | MRI (GRE/SWI sequences): Shows lobar hemorrhages of varying ages, characteristic cortical microbleeds. |
| Developmental Venous Anomaly (DVA) | Common vascular variant, usually benign. Rarely associated with hemorrhage (often linked to co-existing cavernoma). | MRI: Characteristic "caput medusae" appearance of draining veins converging to a collector vein. Enhances post-contrast. |
Diagnostic Imaging: Visualizing AVMs to determine their precise location, size, feeding arteries, draining veins, and nidus structure is crucial for treatment planning. Key imaging modalities include [1, 7]:
- Magnetic Resonance Imaging (MRI) and MR Angiography (MRA): Excellent for showing the AVM nidus, surrounding brain tissue, evidence of prior hemorrhage, and associated anatomical changes. MRA provides non-invasive visualization of feeding arteries and draining veins.
- Computed Tomography (CT) and CT Angiography (CTA): CT is very sensitive for detecting acute hemorrhage. CTA provides rapid visualization of the AVM's vascular anatomy, often used in the emergency setting.
- Digital Subtraction Angiography (DSA): Considered the gold standard for detailed assessment of AVM angioarchitecture. It involves injecting contrast directly into arteries via a catheter and provides high-resolution, dynamic images of blood flow, clearly identifying all feeding arteries, the nidus structure, draining veins, and importantly, any associated aneurysms on the feeding arteries or within the nidus, which significantly increase rupture risk.
These imaging techniques help neurosurgeons and neurointerventionalists understand the AVM's characteristics and plan the most appropriate treatment strategy.
Treatment of Cerebrovascular Arteriovenous Malformations (AVMs)
While many cerebral Arteriovenous Malformations (AVMs) carry a risk of rupture over a person's lifetime, the decision regarding intervention (active treatment versus observation) is complex and individualized based on the AVM's characteristics and the patient's condition [1, 12]. For unruptured AVMs, treatment decisions involve carefully weighing the estimated lifetime risk of hemorrhage and other symptoms against the risks associated with potential interventions [8, 12, 13]. Following an initial rupture, treatment is often recommended more strongly due to the increased risk of re-hemorrhage, which is highest in the first year after the bleed [1, 8]. The long-term average annual risk of hemorrhage or re-rupture for an untreated AVM is often cited in the range of 2-4% per year [1, 8].
The primary curative treatment option is often microsurgical resection (complete surgical removal) of the AVM [1, 12]. However, surgery can present significant technical challenges or be considered too high-risk depending on factors like the AVM's location (especially if in or near critical brain areas, known as eloquent cortex), its size, and its venous drainage pattern (often assessed using the Spetzler-Martin grading scale) [1, 14]. In such situations, or sometimes as part of a planned multi-modality treatment strategy, other methods are employed. These include endovascular embolization (using catheters guided through blood vessels to inject materials like glue or coils into the AVM's feeding arteries and core 'nidus' to block blood flow) and stereotactic radiosurgery (highly focused radiation therapy) [1, 12, 15].
Stereotactic radiosurgery aims to gradually obliterate (close off) the AVM blood vessels over a period of months to years using precisely targeted radiation [1, 15]. Different technologies are available:
- Proton beam therapy (Proton Therapy): Utilizes beams of protons (heavy charged particles) to deliver the radiation dose.
- Photon-based radiosurgery systems: Utilize highly focused beams of photons (X-rays or gamma rays). Common platforms include:
- Gamma Knife®: Delivers radiation from numerous fixed cobalt sources converging on the target. Often cited for very high precision (e.g., directional error typically not exceeding 0.3 mm) [15].
- Linear Accelerator (LINAC)-based systems (e.g., CyberKnife®): Use a machine (linear accelerator) to generate high-energy X-rays. The machine or the beam delivery system moves to target the AVM from multiple angles, also achieving high precision (e.g., directional error typically less than 1 mm) [15].
Observation (conservative management with regular imaging surveillance) may also be considered, particularly for unruptured AVMs deemed to have a low risk of future hemorrhage or other complications, especially when compared to the risks of intervention [13]. Often, the optimal management involves a combination of these techniques (e.g., pre-operative embolization to reduce blood flow followed by microsurgery, or embolization combined with radiosurgery) [1, 12].
References
- Ropper AH, Samuels MA, Klein JP, Prasad S. Adams and Victor's Principles of Neurology. 11th ed. McGraw Hill; 2019. Chapter 34: Cerebrovascular Diseases (Section on Vascular Malformations).
- McDonald J, Bayrak-Toydemir P, Pyeritz RE. Hereditary hemorrhagic telangiectasia: an overview of diagnosis, management, and pathogenesis. Genet Med. 2011 Jun;13(6):607-16.
- Shovlin CL. Hereditary haemorrhagic telangiectasia: pathophysiology, diagnosis and treatment. Blood Rev. 2010 Nov;24(6):203-19.
- Greenberg MS. Handbook of Neurosurgery. 9th ed. Thieme; 2019. Chapter 38: Arteriovenous Malformations.
- Kumar V, Abbas AK, Aster JC. Robbins & Cotran Pathologic Basis of Disease. 10th ed. Elsevier; 2020. Chapter 28: The Central Nervous System (Section on Vascular Diseases).
- Osborn AG, Hedlund GL, Salzman KL. Osborn's Brain: Imaging, Pathology, and Anatomy. 2nd ed. Elsevier; 2017. Section on Vascular Malformations (Spinal).
- Osborn AG, Hedlund GL, Salzman KL. Osborn's Brain: Imaging, Pathology, and Anatomy. 2nd ed. Elsevier; 2017. Section on Vascular Malformations (Brain).
- Stapf C, Mast H, Sciacca RR, et al. Predictors of hemorrhage in patients with untreated brain arteriovenous malformation. Neurology. 2006 May 23;66(10):1350-5.
- Gross BA, Du R. Cerebral vasospasm after arteriovenous malformation rupture. J Clin Neurosci. 2013 Feb;20(2):201-6.
- Lasjaunias PL, Chng SM, Sachet M, Alvarez H, Rodesch G, Garcia-Monaco R. The vein of Galen aneurysmal malformations. Childs Nerv Syst. 2006 Mar;22(3):362. (Note: This reference is older but addresses the specific malformation).
- Winn HR. Youmans and Winn Neurological Surgery. 7th ed. Elsevier; 2017. Volume 4, Chapters on Intracranial Hemorrhage, Vascular Malformations.
- Derdeyn CP, Zipfel GJ, Albuquerque FC, et al. Management of Brain Arteriovenous Malformations: A Scientific Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2017 Aug;48(8):e200-e224.
- Mohr JP, Parides MK, Stapf C, et al; ARUBA Investigators. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet. 2014 Feb 15;383(9917):614-21.
- Spetzler RF, Martin NA. A proposed grading system for arteriovenous malformations. J Neurosurg. 1986 Oct;65(4):476-83.
- Lunsford LD, Kondziolka D, Flickinger JC. Gamma knife radiosurgery for arteriovenous malformations of the brain. J Neurosurg. 2013 Dec;119 Suppl:1-4. (Or similar review on radiosurgery for AVMs).
See also
- Ischemic stroke, cerebral ischemia
- Vertebrobasilar insufficiency (VBI) with vertigo symptom
- Somatoform autonomic dysfunction
- Dizziness, stuffiness in ear and tinnitus
- Ischemic brain disease:
- Atherosclerotic thrombosis
- Atherothrombotic occlusion of internal carotid artery
- Asymptomatic carotid bifurcation stenosis with noise
- Atherothrombotic occlusion of vertebrobasilar and posterior cerebral arteries
- Atherothrombotic occlusion of posterior cerebral artery
- Atherothrombotic occlusion of vertebral and posterior inferior cerebellar arteries (PICA)
- Atherothrombotic occlusion of basilar artery
- Small-vessel stroke (lacunar infarction)
- Other causes of ischemic stroke (cerebral infarction)
- Cerebral embolism
- Spontaneous intracranial (subarachnoid) and intracerebral hemorrhage:
- Arteriovenous malformations of the brain
- Hypertensive intracerebral hemorrhage
- Cerebral arteries inflammatory diseases (cerebral arteritis)
- Giant intracranial aneurysms
- Other causes of intracerebral hemorrhage
- Lobar intracerebral hemorrhage
- Saccular aneurysm and subarachnoid hemorrhage
- Mycotic intracranial aneurysms
- Repeated cerebral artery aneurysm rupture
- Communicating hydrocephalus after intracerebral hemorrhage with ruptured aneurysm
- Cerebral vasospasm
- Cerebrovascular diseases - ischemic stroke, transient ischemic attack (TIA):
- Transient ischemic attack (TIA)
- Sigmoid sinus suppurative thrombophlebitis with thrombosis