Cerebral vasospasm
Cerebral Vasospasm: Definition and Pathophysiology
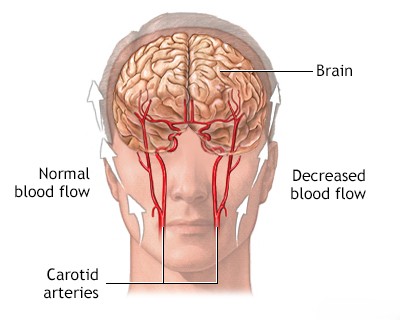
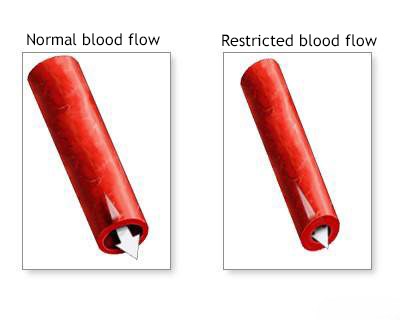
Cerebral vasospasm refers to the delayed narrowing (constriction) of large and medium-sized cerebral arteries at the base of the brain, occurring typically after an aneurysmal subarachnoid hemorrhage (SAH) [1, 2]. While angiographic vasospasm (narrowing seen on imaging) is common, the major concern is symptomatic vasospasm, which leads to reduced blood flow and can cause Delayed Cerebral Ischemia (DCI) – neurological deficits or cerebral infarction arising days after the initial bleed [1, 2].
DCI due to vasospasm is a major cause of morbidity and mortality following SAH, affecting approximately 30% of patients who survive the initial aneurysm rupture [1, 2]. The onset of vasospasm typically occurs between day 4 and day 14 after the SAH, peaking around day 7-10 [1, 2]. Patients may initially improve or stabilize after the aneurysm rupture, only to develop new or worsening neurological deficits during this critical window [1].
Pathophysiology and Epidemiology
The exact pathophysiology of vasospasm is complex and not fully understood, but it is strongly linked to the presence and breakdown of clotted blood in the subarachnoid space surrounding the arteries [1, 2]. Hypotheses involve [1, 2]:
- Inflammatory Response: Breakdown products of hemoglobin (like oxyhemoglobin, bilirubin) released from the clot trigger inflammatory cascades and oxidative stress, leading to smooth muscle contraction and endothelial dysfunction in the arterial walls.
- Vasoactive Substances: Various substances implicated include endothelins, serotonin, prostaglandins, and catecholamines, though their exact roles and the prolonged nature of vasospasm remain debated.
- Structural Changes: Prolonged spasm may also involve structural changes in the arterial wall, contributing to sustained narrowing.
Clinical evidence strongly supports the correlation between the amount and location of subarachnoid blood on early brain imaging (CT or MRI) and the risk, severity, and location of subsequent vasospasm [1, 2, 3]. Large-volume hemorrhages, particularly thick clots in the basal cisterns and fissures (often assessed using the Fisher or modified Fisher scales), are predictive of higher vasospasm risk [3]. CT scans performed between 24 and 96 hours post-SAH are considered most predictive for assessing clot burden related to vasospasm risk, especially for the anterior circulation (anterior and middle cerebral arteries) [1]. Predicting posterior circulation vasospasm based on CT clot burden is often more difficult due to imaging limitations in the posterior fossa [1].
The prolonged interaction between the blood clot and the surrounding artery is thought to be key, potentially impairing normal vessel function and nutrient exchange (as intracranial arteries lack extensive vasa vasorum and rely partly on CSF for nourishment) [1].
Clinical Presentation: Symptomatic Vasospasm and DCI
The clinical diagnosis of symptomatic vasospasm, often leading to DCI, is made when a patient develops new focal neurological deficits, a decline in consciousness, or both, typically between days 4 and 14 post-SAH, after other causes (like rebleeding, hydrocephalus, seizures, metabolic disturbances, infection) have been reasonably excluded [1, 2].
The specific symptoms depend on the arterial territory affected by the reduced blood flow [1]:
- Middle Cerebral Artery (MCA) Territory: Contralateral hemiparesis (weakness, often face/arm > leg), contralateral hemisensory loss, aphasia (if dominant hemisphere), neglect or anosognosia (if non-dominant hemisphere).
- Anterior Cerebral Artery (ACA) Territory: Contralateral leg > arm weakness/sensory loss, abulia (lack of motivation, slowed responses, reduced speech output), incontinence.
- Posterior Cerebral Artery (PCA) Territory: Contralateral homonymous hemianopia (visual field defect), memory impairment, confusion.
- Vertebrobasilar Territory: Altered consciousness, cranial nerve palsies, ataxia, bilateral motor deficits (less common presentation for vasospasm-induced DCI compared to anterior circulation).
It's important to note that significant vasospasm detected on imaging (angiographic vasospasm) does not always cause clinical symptoms, likely due to adequate collateral circulation compensating for the reduced flow in the main spastic vessel [1]. Symptom onset can be gradual over hours to days or occur more abruptly [1].
Severe, widespread vasospasm, particularly involving major arteries like the MCA, can lead to large territorial infarcts [1]. The resulting cerebral edema can further increase intracranial pressure (ICP), potentially causing herniation and death [1]. Predicting which patients with large clot burdens will develop devastating edema remains challenging, but involvement of multiple vascular territories (e.g., ACA and MCA) increases the risk, as collateral supply is compromised [1].
Cerebral Vasospasm: Prevention and Treatment
Management focuses on prevention, monitoring, and treatment of symptomatic vasospasm/DCI [1, 2].
Prevention:
- Nimodipine: This calcium channel blocker is the only medication proven to improve neurological outcomes after SAH, although it doesn't consistently prevent or reverse angiographic vasospasm [1, 2]. It is thought to work potentially via neuroprotection or improving microcirculatory flow rather than solely large vessel dilation [1]. It is standard practice to administer oral nimodipine (e.g., 60mg every 4 hours) for 21 days to all patients with aneurysmal SAH [2].
- Maintaining Euvolemia: Avoiding dehydration and maintaining normal fluid balance is crucial [2].
- Early Aneurysm Securing: Treating the ruptured aneurysm promptly (clipping or coiling) allows for more aggressive management of vasospasm if it occurs, without the high risk of rebleeding associated with induced hypertension [1, 2].
Monitoring:
- Clinical Neurological Assessment: Frequent checks are essential to detect subtle changes indicating DCI onset [1, 2].
- Transcranial Doppler (TCD) Ultrasound: Non-invasive bedside tool used serially to monitor blood flow velocities in major intracranial arteries [1, 2]. Markedly increased velocities can indicate developing vasospasm, often before symptoms appear, prompting heightened vigilance or further investigation [1].
- CT Angiography (CTA) / CT Perfusion (CTP): Can visualize vessel narrowing (CTA) and assess cerebral blood flow/volume deficits (CTP), helping to confirm vasospasm and ischemia when clinical suspicion arises [2, 4].
- Digital Subtraction Angiography (DSA): Remains the gold standard for visualizing vasospasm severity and distribution, often performed if clinical deterioration occurs despite medical management or if endovascular treatment is contemplated [1, 4].
Differential Diagnosis of Delayed Neurological Deterioration After SAH [1, 2]
| Condition | Typical Onset Post-SAH | Key Features / Distinguishing Points | Typical Investigations / Findings |
|---|---|---|---|
| Delayed Cerebral Ischemia (DCI) due to Vasospasm | Days 4-14 (Peak 7-10) | New focal deficit (hemiparesis, aphasia) or decline in LOC. Often gradual/fluctuating. Correlates with clot burden. | CT head excludes rebleed/hydrocephalus. CTA/DSA confirms vasospasm. TCD shows high velocities. CT Perfusion/MRI shows ischemia. |
| Aneurysmal Rerupture | Highest risk first 24h, remains high until secured (first ~2 weeks). | Sudden, catastrophic decline in LOC, often severe headache increase, new deficits, potential cardiopulmonary arrest. | Repeat Head CT shows new/increased hemorrhage (SAH, IVH, ICH). Urgent angiography needed if unsecured. |
| Hydrocephalus (Acute or Chronic Communicating) | Acute: First few days. Chronic: Days to weeks later. | Acute: Decline in LOC. Chronic: Gait disturbance, cognitive decline, incontinence triad (NPH-like). | CT/MRI shows ventriculomegaly disproportionate to atrophy. LP may show high/normal pressure; response to CSF drainage supports diagnosis (chronic). |
| Seizures / Status Epilepticus | Can occur anytime post-SAH. | Clinical seizure activity or subtle signs (non-convulsive status). Post-ictal confusion/deficits. | EEG confirms seizure activity or post-ictal state. Imaging excludes new structural lesion. |
| Hyponatremia | Common complication (SIADH or CSW), usually within first 2 weeks. | Altered mental status, lethargy, seizures (if severe). | Low serum sodium. Urine/serum osmolality help differentiate SIADH vs CSW. Normal head imaging. |
| Systemic Infection / Sepsis | Can occur anytime (e.g., pneumonia, UTI). | Fever, altered mental status, signs of source infection. | Positive cultures (blood, urine, sputum). Elevated inflammatory markers. Normal head imaging usually. |
| Medication Effects (e.g., Sedation) | Decreased LOC related to administration or accumulation of sedative/analgesic medications. | Review medication record. Response to decreased sedation or reversal agents (if applicable). Normal imaging. |
Treatment of Symptomatic Vasospasm / DCI [1, 2]:
- Hemodynamic Therapy (Induced Hypertension and Euvolemia): This is a mainstay of medical management once symptomatic vasospasm/DCI is diagnosed (and the aneurysm is secured). The goal is to increase cerebral perfusion pressure (CPP) to overcome the resistance caused by narrowed arteries. This typically involves:
- Ensuring adequate hydration and central venous pressure (maintaining euvolemia).
- Inducing hypertension using vasopressor agents (e.g., norepinephrine, phenylephrine) to achieve specific target systolic or mean arterial pressure goals, guided by neurological response and monitoring (ICP, CPP if available).
- Requires intensive care unit (ICU) monitoring of cardiovascular status, fluid balance, and neurological condition.
- Endovascular Therapy: Used for medically refractory symptomatic vasospasm confirmed on angiography. Options include:
- Intra-arterial Vasodilator Infusion: Direct infusion of drugs like nicardipine, verapamil, or milrinone into the spastic arteries via catheter can temporarily relieve vasospasm. Often requires repeat treatments.
- Percutaneous Transluminal Angioplasty (PTA): Mechanical dilation of focal, proximal segments of spastic arteries using a balloon catheter. Can provide more durable dilation but carries risks of vessel rupture or dissection. Reserved for severe, accessible spasm unresponsive to other therapies.
- Management of Cerebral Edema / Increased ICP: If vasospasm leads to large infarcts and significant edema causing elevated ICP:
- Standard ICP management techniques: Head elevation, osmotic therapy (mannitol, hypertonic saline).
- In severe cases: Decompressive hemicraniectomy (surgical removal of part of the skull) may be life-saving.
Despite these interventions, cerebral vasospasm and DCI remain significant challenges. Ongoing research aims to better understand the pathophysiology and develop more effective targeted therapies, potentially including anti-inflammatory agents or novel vasodilators, and strategies like early clot removal [1, 2].
References
- Ropper AH, Samuels MA, Klein JP, Prasad S. Adams and Victor's Principles of Neurology. 11th ed. McGraw Hill; 2019. Chapter 34: Cerebrovascular Diseases (Section on Cerebral Vasospasm and Delayed Cerebral Ischemia).
- Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al; American Heart Association Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Clinical Cardiology. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012 Jun;43(6):1711-37.
- Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980 Jan;6(1):1-9. (Original Fisher scale paper).
- Osborn AG, Hedlund GL, Salzman KL. Osborn's Brain: Imaging, Pathology, and Anatomy. 2nd ed. Elsevier; 2017. Section on Subarachnoid Hemorrhage and Vasospasm.
- Diringer MN, Bleck TP, Claude Hemphill J 3rd, et al; Neurocritical Care Society. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the Neurocritical Care Society's Multidisciplinary Consensus Conference. Neurocrit Care. 2011 Sep;15(2):211-40.
- Bahra A, Matharu MS, Buchem MA, et al. Antifibrinolytic treatment for aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD001245. Review. Update in: Cochrane Database Syst Rev. 2013;8:CD001245. (Or more recent review on antifibrinolytics).
See also
- Ischemic stroke, cerebral ischemia
- Vertebrobasilar insufficiency (VBI) with vertigo symptom
- Somatoform autonomic dysfunction
- Dizziness, stuffiness in ear and tinnitus
- Ischemic brain disease:
- Atherosclerotic thrombosis
- Atherothrombotic occlusion of internal carotid artery
- Asymptomatic carotid bifurcation stenosis with noise
- Atherothrombotic occlusion of vertebrobasilar and posterior cerebral arteries
- Atherothrombotic occlusion of posterior cerebral artery
- Atherothrombotic occlusion of vertebral and posterior inferior cerebellar arteries (PICA)
- Atherothrombotic occlusion of basilar artery
- Small-vessel stroke (lacunar infarction)
- Other causes of ischemic stroke (cerebral infarction)
- Cerebral embolism
- Spontaneous intracranial (subarachnoid) and intracerebral hemorrhage:
- Arteriovenous malformations of the brain
- Hypertensive intracerebral hemorrhage
- Cerebral arteries inflammatory diseases (cerebral arteritis)
- Giant intracranial aneurysms
- Other causes of intracerebral hemorrhage
- Lobar intracerebral hemorrhage
- Saccular aneurysm and subarachnoid hemorrhage
- Mycotic intracranial aneurysms
- Repeated cerebral artery aneurysm rupture
- Communicating hydrocephalus after intracerebral hemorrhage with ruptured aneurysm
- Cerebral vasospasm
- Cerebrovascular diseases - ischemic stroke, transient ischemic attack (TIA):
- Transient ischemic attack (TIA)
- Sigmoid sinus suppurative thrombophlebitis with thrombosis