Ischemic brain disease, cerebrovascular thrombosis and embolism
Ischemic Brain Disease: Cerebrovascular Thrombosis and Embolism Overview
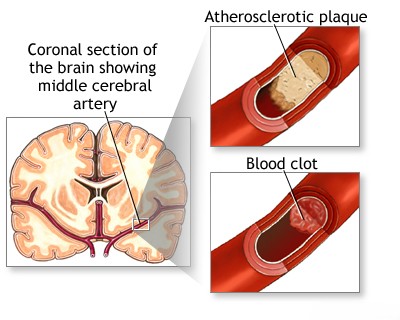
Ischemic brain disease develops when blood flow to the brain is insufficient, usually because the arteries supplying it become narrowed (stenosis) or blocked [1, 2]. Blockages are typically caused by either thrombosis (a blood clot forming locally, often at a site of underlying vessel wall disease) or embolism (obstruction by a clot or debris that traveled from another part of the body) [1, 2]. This section delves into cerebral vessel thrombosis, exploring the diverse pathological processes that lead to its formation.
Clinically, cerebral embolism often presents with symptoms very similar to those of thrombosis [1]. Specific differentiating factors are detailed in the section covering embolism of the neck and brain arteries.
Common types of thrombotic and embolic events leading to ischemic brain disease include:
- Atherosclerotic thrombosis
- Atherothrombotic occlusion of the internal carotid artery
- Asymptomatic carotid bifurcation stenosis with bruit
- Atherothrombotic occlusion of vertebrobasilar and posterior cerebral arteries
- Atherothrombotic occlusion of the posterior cerebral artery
- Atherothrombotic occlusion of vertebral and posterior inferior cerebellar arteries (PICA)
- Atherothrombotic occlusion of the basilar artery
- Small-vessel stroke (lacunar infarction)
- Other causes of ischemic stroke (cerebral infarction)
- Cerebral embolism
Differential Diagnosis of Symptoms Suggesting Ischemic Brain Disease [1, 3]
| Condition | Key Features / Distinguishing Points | Typical Investigations / Findings |
|---|---|---|
| Ischemic Stroke / TIA (Thrombotic/Embolic) | Sudden onset focal neurological deficit corresponding to vascular territory. Risk factors often present. TIA resolves completely (<24h, often <1h). | CT head excludes hemorrhage. MRI (DWI) confirms ischemia early. Vascular imaging (US, CTA, MRA) identifies cause (stenosis, occlusion, embolism source). |
| Intracerebral Hemorrhage (ICH) | Sudden onset focal deficit, often with headache, vomiting, decreased consciousness, severe hypertension. | Non-contrast CT head shows hemorrhage. |
| Seizure with Todd's Paralysis | Post-ictal focal weakness mimicking stroke. History of seizure. Transient (resolves <48h). | History. EEG may show abnormalities. Imaging usually normal unless underlying lesion. Transient nature. |
| Migraine with Aura (esp. Hemiplegic) | Transient neurological symptoms (often spreading gradually) followed by/accompanying headache. History of similar episodes. Full recovery. | Clinical diagnosis. Normal exam between attacks. Imaging usually normal. |
| Hypoglycemia | Can cause focal neurological deficits, confusion, seizures. History of diabetes relevant. | Low blood glucose. Symptoms improve with glucose. |
| Brain Tumor | Can present acutely with hemorrhage/seizure causing focal signs, but often progressive symptoms precede. | MRI with contrast shows mass lesion. |
| Subdural Hematoma | Can cause focal signs due to compression. Headache, altered mental status. History of trauma (may be minor). | CT/MRI shows subdural collection. |
| Metabolic Encephalopathy | Diffuse dysfunction (confusion, lethargy). Focal signs uncommon unless superimposed issue. Identifiable systemic cause. | Specific lab abnormalities. Imaging non-specific. |
| Peripheral Vertigo (e.g., Labyrinthitis) | Acute vertigo, nausea, vomiting. No other brainstem/cerebellar signs usually. Can mimic posterior circulation TIA/stroke. | Clinical exam (HINTS). Normal brain imaging. |
| Syncope | Brief loss of consciousness due to global hypoperfusion. Often prodrome. Rapid recovery. Can mimic TIA if brief focal symptoms occur. | History. Cardiac evaluation (ECG, Holter), orthostatic vitals. Normal neurological exam post-event. |
| Functional Neurological Disorder | Symptoms inconsistent with organic patterns. Positive clinical signs. | Diagnosis of exclusion. Normal imaging/labs. |
References
- Ropper AH, Samuels MA, Klein JP, Prasad S. Adams and Victor's Principles of Neurology. 11th ed. McGraw Hill; 2019. Chapter 34: Cerebrovascular Diseases.
- Grotta JC, Albers GW, Broderick JP, et al. Stroke: Pathophysiology, Diagnosis, and Management. 7th ed. Elsevier; 2021. Chapter on Mechanisms of Ischemic Stroke.
- Caplan LR. Stroke Mimics. Semin Neurol. 2016 Apr;36(2):203-12. (Or relevant chapter in Adams/Victor or Grotta).
See also
- Ischemic stroke, cerebral ischemia
- Vertebrobasilar insufficiency (VBI) with vertigo symptom
- Somatoform autonomic dysfunction
- Dizziness, stuffiness in ear and tinnitus
- Ischemic brain disease:
- Atherosclerotic thrombosis
- Atherothrombotic occlusion of internal carotid artery
- Asymptomatic carotid bifurcation stenosis with noise
- Atherothrombotic occlusion of vertebrobasilar and posterior cerebral arteries
- Atherothrombotic occlusion of posterior cerebral artery
- Atherothrombotic occlusion of vertebral and posterior inferior cerebellar arteries (PICA)
- Atherothrombotic occlusion of basilar artery
- Small-vessel stroke (lacunar infarction)
- Other causes of ischemic stroke (cerebral infarction)
- Cerebral embolism
- Spontaneous intracranial (subarachnoid) and intracerebral hemorrhage:
- Arteriovenous malformations of the brain
- Hypertensive intracerebral hemorrhage
- Cerebral arteries inflammatory diseases (cerebral arteritis)
- Giant intracranial aneurysms
- Other causes of intracerebral hemorrhage
- Lobar intracerebral hemorrhage
- Saccular aneurysm and subarachnoid hemorrhage
- Mycotic intracranial aneurysms
- Repeated cerebral artery aneurysm rupture
- Communicating hydrocephalus after intracerebral hemorrhage with ruptured aneurysm
- Cerebral vasospasm
- Cerebrovascular diseases - ischemic stroke, transient ischemic attack (TIA):
- Transient ischemic attack (TIA)
- Sigmoid sinus suppurative thrombophlebitis with thrombosis