Giant intracranial aneurysms
Giant Intracranial Aneurysms Overview & Classification
Types of Cerebral Aneurysms (based on morphology and cause) [1, 2]:
- Saccular (Berry) Aneurysm – A pouch-like outpouching, typically at vessel bifurcations; this is the most common type and can become giant.
- Fusiform Aneurysm – A diffuse, circumferential widening or dilatation of a vessel segment; can also become giant.
- Dissecting Aneurysm (Pseudoaneurysm) – Forms due to a tear in the vessel wall, with blood collecting between layers; less commonly giant.
- Mycotic (Infectious) Aneurysm – Caused by infection weakening the vessel wall; usually smaller, rarely giant.
Classification by Aneurysm Size (maximum diameter) [1, 3]:
- ≤ 6 mm – Small Aneurysm
- 7 to 12 mm – Medium Aneurysm
- 13 to 24 mm – Large Aneurysm
- ≥ 25 mm (2.5 cm) – Giant Aneurysm
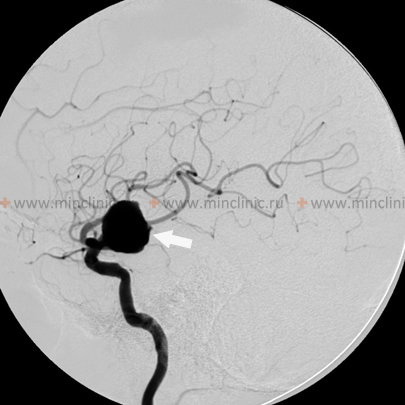
Giant intracranial aneurysms, defined conventionally as those with a maximum diameter greater than or equal to 25 mm, generally occur in the same locations along the cerebral circulation as smaller aneurysms, typically arising at vessel branching points or areas of hemodynamic stress [1, 3]. Common locations where giant cerebral aneurysms are found include the intracranial internal carotid artery (particularly at the origin of the posterior communicating artery, anterior choroidal artery, or the carotid terminus bifurcation), the middle cerebral artery (MCA) bifurcation or trifurcation, and the apex of the basilar artery [1, 3]. While rupture leading to subarachnoid hemorrhage is always a concern with any aneurysm, giant aneurysms often present with neurological symptoms primarily due to their significant mass effect – compression of adjacent cranial nerves, brainstem, or brain parenchyma – rather than solely through rupture [1, 3, 4].
Significant brain edema (swelling) can result from direct compression or potentially from altered hemodynamics related to a giant aneurysm [1]. If severe and progressive, this edema can become irreversible, leading to critical brain compression, increased intracranial pressure, herniation syndromes, and ultimately, patient death [1]. This risk of severe, life-threatening mass effect might be particularly high with certain giant aneurysms, such as those located at the middle cerebral artery bifurcation where they can compress large areas of the temporal or frontal lobes [1]. In situations with acute neurological deterioration due to mass effect from a giant aneurysm, urgent intervention (whether neurosurgical or endovascular) aimed at decompressing the aneurysm or reducing its mass may be the only viable treatment option [1, 5]. However, direct surgical clipping or endovascular treatment (coiling, flow diversion) of giant cerebral aneurysms is often technically challenging due to their size, wide necks, incorporation of vital branch origins, presence of intraluminal thrombus, and calcification of the aneurysm wall [1, 5]. Such complex interventions carry significant risks and can sometimes be complicated by issues like postoperative cerebral edema or incomplete aneurysm occlusion [1, 5].
Differential Diagnosis of Mass Lesions Mimicking Giant Aneurysms [1, 4, 6]
| Condition | Key Features / Distinguishing Points | Typical Imaging Findings |
|---|---|---|
| Giant Aneurysm (Saccular/Fusiform) | Well-defined vascular outpouching/dilatation ≥25mm. Often arises at bifurcation. May have mass effect (CN palsies, brain compression), headache, +/- rupture (SAH/ICH). | MRI: Often complex signal (flow voids, laminated thrombus). MRA/CTA shows direct connection to parent artery. DSA confirms diagnosis, details neck/flow. |
| Meningioma | Dural-based tumor. Slow growing. Headache, seizures, focal deficits due to compression. Often parasellar, CPA, convexity. | MRI: Isointense T1/T2, intense homogeneous enhancement, "dural tail" common. CT: Often hyperdense, may calcify or cause hyperostosis. No direct arterial connection. |
| Schwannoma (e.g., Vestibular) | Arises from nerve sheath. CPA common (CN VIII). Hearing loss, tinnitus, vertigo, facial numbness/weakness. | MRI: Often T1 hypo/iso, T2 hyper, avid enhancement. May show extension into internal auditory canal ("ice cream cone" sign). No direct arterial connection. |
| Pituitary Macroadenoma | Sellar/suprasellar mass. Visual field defects, headache, endocrine dysfunction (hormone excess or hypopituitarism). | MRI: Sellar mass extending suprasellar, often compresses chiasm. T1 iso/hypo, T2 variable. Usually enhances (less intensely than meningioma). |
| Craniopharyngioma | Suprasellar mass, often cystic/solid. Children/older adults. Visual loss, endocrine disturbance, headache. | MRI: Complex cystic/solid mass, enhances (solid/wall). CT: Calcification very common. |
| Chordoma / Chondrosarcoma | Skull base tumors (clivus typical). Bone destruction, CN palsies. | CT shows bone destruction. MRI: Enhancing mass, often T2 hyperintense (chordoma). |
| Epidermoid / Dermoid Cyst | Congenital inclusion cysts. Slow growing. Often off-midline (CPA, parasellar). | MRI: Epidermoid restricts diffusion (DWI bright). Dermoid shows fat signal. Usually minimal/no enhancement. |
| Metastasis | Known primary cancer. Can occur anywhere, including skull base/parasellar. | MRI: Enhancing lesion(s), often with surrounding edema. Search for primary. |
| Granulomatous Disease (e.g., TB, Sarcoidosis) | Can form mass lesions or cause basal meningitis/pachymeningitis mimicking aneurysm complications. | MRI: Enhancing lesions or dural thickening. CSF analysis/systemic workup helpful. Biopsy may be needed. |
References
- Greenberg MS. Handbook of Neurosurgery. 9th ed. Thieme; 2019. Chapter 37: Intracranial Aneurysms.
- Ropper AH, Samuels MA, Klein JP, Prasad S. Adams and Victor's Principles of Neurology. 11th ed. McGraw Hill; 2019. Chapter 34: Cerebrovascular Diseases (Section on Intracranial Aneurysms).
- Winn HR. Youmans and Winn Neurological Surgery. 7th ed. Elsevier; 2017. Volume 4, Chapter 368: Giant Intracranial Aneurysms.
- Osborn AG, Hedlund GL, Salzman KL. Osborn's Brain: Imaging, Pathology, and Anatomy. 2nd ed. Elsevier; 2017. Section on Aneurysms.
- Thompson BG, Brown RD Jr, Amin-Hanjani S, et al; American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, Council on Functional Genomics and Translational Biology, and Council on Hypertension. Guidelines for the Management of Patients With Unruptured Intracranial Aneurysms: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2015 Aug;46(8):2368-400. (Includes discussion of giant aneurysms).
- Osborn AG, Hedlund GL, Salzman KL. Osborn's Brain: Imaging, Pathology, and Anatomy. 2nd ed. Elsevier; 2017. Section on Neoplasms and Tumorlike Conditions (for differential diagnosis).
See also
- Ischemic stroke, cerebral ischemia
- Vertebrobasilar insufficiency (VBI) with vertigo symptom
- Somatoform autonomic dysfunction
- Dizziness, stuffiness in ear and tinnitus
- Ischemic brain disease:
- Atherosclerotic thrombosis
- Atherothrombotic occlusion of internal carotid artery
- Asymptomatic carotid bifurcation stenosis with noise
- Atherothrombotic occlusion of vertebrobasilar and posterior cerebral arteries
- Atherothrombotic occlusion of posterior cerebral artery
- Atherothrombotic occlusion of vertebral and posterior inferior cerebellar arteries (PICA)
- Atherothrombotic occlusion of basilar artery
- Small-vessel stroke (lacunar infarction)
- Other causes of ischemic stroke (cerebral infarction)
- Cerebral embolism
- Spontaneous intracranial (subarachnoid) and intracerebral hemorrhage:
- Arteriovenous malformations of the brain
- Hypertensive intracerebral hemorrhage
- Cerebral arteries inflammatory diseases (cerebral arteritis)
- Giant intracranial aneurysms
- Other causes of intracerebral hemorrhage
- Lobar intracerebral hemorrhage
- Saccular aneurysm and subarachnoid hemorrhage
- Mycotic intracranial aneurysms
- Repeated cerebral artery aneurysm rupture
- Communicating hydrocephalus after intracerebral hemorrhage with ruptured aneurysm
- Cerebral vasospasm
- Cerebrovascular diseases - ischemic stroke, transient ischemic attack (TIA):
- Transient ischemic attack (TIA)
- Sigmoid sinus suppurative thrombophlebitis with thrombosis