Sebaceous cyst (epidermoid cyst)
Understanding Sebaceous Cysts (Epidermoid and Pilar Cysts)
Sebaceous cysts, more accurately termed epidermoid cysts or pilar cysts (trichilemmal cysts) depending on their origin, are common benign skin lesions that can affect people of all ages and both genders. The term "atheroma" is often used synonymously, particularly in older literature, to refer to these types of cysts. Understanding the nature of these common skin "lumps" is important for appropriate management.
What is a Sebaceous Cyst (Atheroma)?
Technically, a true sebaceous cyst arises from sebaceous glands and is relatively rare. More commonly, what are referred to as "sebaceous cysts" are actually:
- Epidermoid Cysts: These arise from the epidermis (the outermost layer of skin), specifically from the infundibulum of a hair follicle. They are lined by stratified squamous epithelium similar to the epidermis and are filled with keratin (a protein found in skin, hair, and nails), which appears as a thick, cheesy, yellowish-white material, often with an unpleasant odor.
- Pilar Cysts (Trichilemmal Cysts): These arise from the outer root sheath of the hair follicle, most commonly on the scalp. They are also filled with keratin but have a thicker wall and typically lack the central punctum seen in epidermoid cysts.
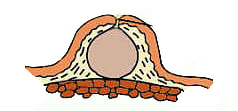
Both types are essentially sacs or "pouches" possessing a distinct capsule (wall) and containing keratinous debris. The formation is often attributed to the blockage of the excretory duct of a hair follicle or sebaceous gland by thickened sebum or keratin, leading to accumulation of these materials within the enclosed sac.
Common Locations and Formation
These cysts typically develop on areas of the skin rich in sebaceous glands or hair follicles, including:
- Scalp (pilar cysts are very common here)
- Face (cheeks, forehead, around the ears)
- Neck
- Back and chest
- Anterior abdominal wall
- Scrotum and labia
The blockage of the follicle opening prevents the normal shedding of skin cells and sebum, leading to the gradual enlargement of the cyst as these materials accumulate within the encapsulated "pouch."
Clinical Presentation and Diagnosis of Sebaceous Cysts
Typical Appearance and Characteristics
Clinically, an epidermoid or pilar cyst can be located in many areas of the body, as mentioned, with a higher prevalence on the face (e.g., cheek), scalp, torso, arms, and scrotum. Multiple cysts can occur, a condition sometimes referred to as steatocystoma multiplex or epidermoid cystosis, particularly on the scalp.
On examination, a typical cyst presents as:
- A well-defined, dome-shaped or round, tumor-like subcutaneous or intradermal formation.
- Soft, doughy, or rubbery consistency.
- Size can range from a few millimeters (e.g., 5 mm) to several centimeters (e.g., 40 mm or more).
- The overlying skin is usually normal in color and texture, though it may be stretched.
- A central, dark punctum (comedone-like opening) may be visible on the surface of epidermoid cysts, representing the blocked follicle opening. This is less common with pilar cysts.
- The cyst is typically mobile over deeper tissues but tethered to the overlying skin at the site of the punctum (if present).
- Generally painless unless inflamed or infected.
- It may remain stable in size for many years or gradually enlarge over time.
Differentiating from Lipomas
Epidermoid/pilar cysts and lipomas (benign fatty tumors) can appear very similar superficially, but a clinician can often distinguish them based on subtle evidence:
- Location: While both can occur widely, lipomas are generally found in areas with abundant subcutaneous fatty tissue. Epidermoid/pilar cysts are more tied to areas rich in hair follicles or sebaceous glands.
- Punctum: The presence of a central punctum is characteristic of an epidermoid cyst and absent in a lipoma.
- Attachment to Skin: Epidermoid/pilar cysts are often tethered to the skin, especially at the punctum. A lipoma is a subcutaneous formation that is typically not adherent to the overlying skin surface and feels more lobulated and softer.
- Consistency: Both can feel soft, but lipomas often have a more "slippery" or lobulated feel, while cysts may feel more tense or fluctuant if filled with liquid keratin.
Definitive differentiation often requires histological examination after removal, but clinical suspicion is usually high.
Potential Complications (Inflammation and Rupture)
Sometimes, an epidermoid or pilar cyst can communicate with the skin surface through a small opening, allowing for the intermittent discharge of its keratinous contents. More significant complications include:
- Inflammation/Infection: Cysts frequently become inflamed or secondarily infected by bacteria, leading to pain, redness, swelling, and tenderness. This can result in the formation of an abscess within or around the cyst, involving the surrounding soft tissues.
- Rupture: An inflamed or traumatized cyst may rupture, either externally onto the skin surface or internally into the subcutaneous tissue. Rupture can cause a significant foreign body inflammatory reaction to the keratin contents, leading to pain, swelling, and potential scarring.
If a cyst is small, asymptomatic, and not cosmetically bothersome to the patient, it may not require removal and can be observed. However, in cases of recurrent inflammation, infection, rupture, cosmetic concern, or if the diagnosis is uncertain, surgical treatment (excision) is indicated.
Surgical Treatment of Sebaceous Cysts
The definitive treatment for epidermoid and pilar cysts is complete surgical excision. This is typically an outpatient procedure performed under local anesthesia.
Indications for Removal and Anesthesia
Indications for removal include:
- Recurrent inflammation or infection.
- Pain or discomfort.
- Cosmetic concerns.
- Rapid increase in size.
- Uncertainty of diagnosis (though most are clinically obvious).
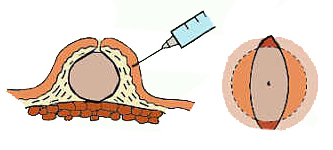
Local anesthesia, commonly with a 1-2% solution of lidocaine (often with epinephrine to reduce bleeding) or historically novocaine (procaine), is infiltrated around and beneath the cyst.
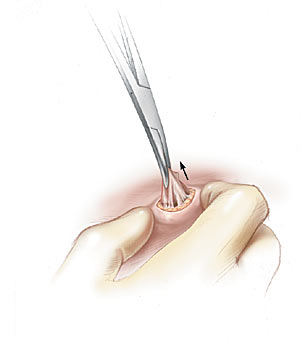
Surgical Removal Method #1: Incision and Expression/Curettage
This method is often used for acutely inflamed or infected cysts where complete excision of an intact capsule is difficult or risks spreading infection, or for very small cysts.
- A small incision is made over the most prominent or fluctuant part of the cyst.
- The keratinous or purulent contents of the cyst are expressed (squeezed out) onto a napkin or into a collection dish.
- After evacuation, the cyst cavity may be explored. Attempts are made to grasp and remove the cyst capsule (wall) with forceps, or the cavity is thoroughly scraped out (curetted) with a sharp spoon (curette) to remove as much of the lining as possible.
The disadvantage of this method is a higher risk of recurrence if the cyst capsule is not completely removed, as any remaining epithelial lining can regenerate the cyst.
Surgical Removal Method #2: Elliptical Excision with Intact Capsule (Ideal for Non-Inflamed Cysts)
This method aims for complete removal of the cyst with its capsule intact, which offers the lowest recurrence rate. It is best suited for non-inflamed cysts.
- An elliptical (oval-shaped) incision is carefully made through the skin overlying the cyst, ideally incorporating the central punctum if present. Care is taken not to rupture the cyst capsule.
- The skin edges are gently dissected away from the cyst capsule.
- Using blunt and sharp dissection, the cyst is carefully shelled out (exfoliated) from the surrounding subcutaneous tissue, keeping the capsule intact. Pressing the edges of the wound with fingers can sometimes help "pop out" or enucleate the cyst.
Surgical Removal Method #3: Excision with Minimal Incision (Often Preferred)
This method is frequently used and aims to remove the cyst intact or with minimal disruption through a relatively small incision.
- Two bordering incisions (often elliptical or fusiform) are made over the cyst, encompassing the central punctum (if present). The length of the incision is typically slightly less than or equal to the diameter of the cyst.
- The edges of the skin incision are grasped with clamps (e.g., skin hooks or fine forceps).
- By applying gentle traction on the skin edges, curved scissors (e.g., Metzenbaum or iris scissors) are introduced under the cyst.
- The cyst is then meticulously exfoliated (dissected free) from the surrounding tissues by carefully spreading and closing the scissor blades, staying close to the cyst wall to avoid rupturing it.
Bleeding with this method of surgery is usually minor, especially if epinephrine was used with the local anesthetic.
Wound Closure and Postoperative Care
After complete removal of the cyst and its capsule, meticulous hemostasis is ensured.
- Subcutaneous Sutures: If there is a significant dead space, separate absorbable sutures may be placed in the subcutaneous tissue to approximate deeper layers and reduce tension on the skin closure.
- Skin Closure: The skin incision is typically closed with fine, non-absorbable sutures (e.g., nylon, polypropylene) using an atraumatic needle. Vertical mattress sutures are sometimes used to evert the wound edges and promote a better cosmetic outcome by preventing the edges from in-rolling. Simple interrupted or running subcuticular sutures can also be used.
- Suture Removal: Skin sutures are usually removed after 7-14 days, depending on the location and tension on the wound. Sutures on the face may be removed earlier (e.g., 5-7 days).
- Dressing: A sterile dressing is applied over the wound.
- Postoperative Instructions: Patients are typically advised to keep the wound clean and dry, watch for signs of infection (redness, swelling, pain, pus), and follow up for suture removal.
If a cyst was acutely inflamed and drained, the wound might be packed open initially to allow for continued drainage and then closed later (delayed primary closure) or allowed to heal by secondary intention if small.
Differential Diagnosis of Superficial Skin Lumps
Epidermoid and pilar cysts need to be differentiated from other common superficial skin and subcutaneous lumps:
| Condition | Key Differentiating Features |
|---|---|
| Epidermoid Cyst | Dome-shaped, firm or fluctuant, often with a central punctum, filled with keratin. Tethered to skin. |
| Pilar Cyst (Trichilemmal Cyst) | Smooth, firm, mobile, most common on scalp (90%). No punctum typically. Thicker wall. Filled with keratin. |
| Lipoma | Soft, doughy, lobulated, mobile subcutaneous fatty tumor. Not attached to overlying skin. No punctum. |
| Dermatofibroma | Firm, often slightly raised or depressed papule/nodule, may be pigmented. "Dimple sign" (retracts with lateral pressure). |
| Neurofibroma | Soft, fleshy, often compressible ("buttonhole sign") papule or nodule. May be associated with neurofibromatosis. |
| Abscess | Painful, erythematous, warm, fluctuant collection of pus. Signs of acute inflammation. |
| Ganglion Cyst | Firm, smooth, often translucent cyst typically near a joint or tendon (e.g., wrist, fingers). Filled with viscous synovial-like fluid. |
| Hidradenitis Suppurativa (in axillae, groin) | Chronic inflammatory condition of apocrine glands leading to recurrent nodules, abscesses, sinus tracts, and scarring. |
| Basal Cell Carcinoma / Squamous Cell Carcinoma (Nodular types) | Malignant. Often pearly, ulcerated, or crusted. Persistent, may bleed. Typically in sun-exposed areas. Biopsy for diagnosis. |
Prevention and When to Seek Medical Attention
There is no specific way to prevent epidermoid or pilar cysts from forming, as they often arise spontaneously. However, maintaining good skin hygiene and avoiding squeezing or traumatizing existing lesions may reduce the risk of inflammation or infection.
Medical attention should be sought from a dermatologist or surgeon if a cyst:
- Becomes painful, red, swollen, or warm (signs of inflammation or infection).
- Ruptures or drains pus or foul-smelling material.
- Grows rapidly in size.
- Is located in an area that causes functional impairment or discomfort.
- Is cosmetically bothersome.
- The diagnosis is uncertain, and other conditions need to be ruled out.
Attempting to squeeze or drain a cyst at home can lead to incomplete removal, inflammation, infection, and scarring, and is generally not recommended.
References
- Weedon D. Weedon's Skin Pathology. 3rd ed. Churchill Livingstone Elsevier; 2010. (Chapter on Cysts and Sinuses).
- Zuber TJ. Minimal excision technique for epidermoid (sebaceous) cysts. Am Fam Physician. 2002 Jun 1;65(11):2341-4.
- Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016. (Chapter on Benign Skin Tumors).
- Thomas VD, Snavely NR, Lee KK, Swanson NA. Benign epithelial tumors, hamartomas, and hyperplasias. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Elsevier; 2018:chap 111.
- Klin B, Ashkenazi H. Sebaceous cyst excision with minimal surgery. Am Fam Physician. 1990 May;41(5):1459-62.
- Nath AK, Kumari R, Thappa DM. Multiple epidermoid cysts. Indian J Dermatol Venereol Leprol. 2010 Nov-Dec;76(6):709.
- Frank E, Macias D. Pilar Cysts. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
See also
- Abscess
- Breast diseases (mastopathy, cyst, calcifications, fibroadenoma, intraductal papilloma, cancer)
- Bursitis
- Furuncle (boil)
- Ganglion cyst
- Hidradenitis suppurativa (HS)
- Ingrown toenail
- Lipoma (fatty tumor)
- Lymphostasis
- Paronychia, panaritium (whitlow or felon)
- Sebaceous cyst (epidermoid cyst)
- Tenosynovitis (infectious, stenosing)