Ganglion cyst
Understanding Ganglion Cysts
Definition and Common Locations
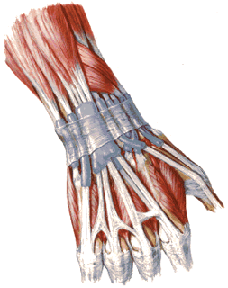
A ganglion cyst is a benign (non-cancerous), fluid-filled cystic formation that arises from the capsule of a joint or the sheath of a tendon. These cysts are filled with a thick, clear, gelatinous, mucoid material, similar in consistency to synovial fluid but usually more viscous. They are the most common soft tissue tumors of the hand and wrist but can occur near other joints as well.
The most frequent locations for ganglion cysts include:
- Dorsum of the Wrist: This is the most common site, typically arising from the scapholunate joint or other carpal joints, often visible between the extensor tendons of the hand.
- Volar (Palmar) Aspect of the Wrist: Often near the radial artery or arising from flexor tendon sheaths.
- Dorsal Aspect of the Foot: Commonly found near the ankle joint or over the tarsal bones, such as near the cuboid bone.
- Fingers and Toes: Smaller ganglion cysts can occur at the base of fingers (flexor tendon sheath ganglia or "seed ganglia") or near the distal interphalangeal (DIP) joints (mucous cysts, often associated with osteoarthritis).
- Knee and Ankle: Less common, but can arise from joint capsules or tendon sheaths in these areas.
Causes and Pathogenesis of Ganglion Cysts
The exact cause and pathogenesis of ganglion cysts are not fully understood, but several theories exist. In some cases, a ganglion cyst appears for no apparent reason on the wrist, hand, foot, or ankle. In other instances, their formation is linked to:
- Trauma or Injury: A history of acute injury (e.g., a bruise or sprain) or chronic microtrauma to the joint or tendon sheath can precede the development of a ganglion cyst. Overload or stress on the joint may play a role.
- Repetitive Motion: Monotonous and frequently repetitive movements of the hand, wrist, or foot (e.g., in certain occupations or sports) are thought to facilitate the appearance of ganglion cysts by stressing the joint capsule or tendon sheath.
- Joint or Tendon Sheath Degeneration: It is believed that ganglion cysts may arise from myxoid degeneration of collagen and connective tissue within the joint capsule or tendon sheath. Small tears or weaknesses in these structures may allow synovial fluid to leak out and become encapsulated, forming the cyst. A one-way valve-like mechanism is often implicated, allowing fluid into the cyst but not back out.
- Anatomical Weakness: Some theories suggest an inherent anatomical weakness of the tissues in areas like the wrist or ankle could predispose individuals to ganglion formation.
- Connective Tissue Disorders: While not a primary cause, underlying joint laxity or connective tissue disorders might be a predisposing factor in some individuals.
Ganglion cysts are not true cysts in the sense of having an epithelial lining; their wall is composed of compressed collagen fibers and mesenchymal cells.
Clinical Presentation and Diagnosis of Ganglion Cysts
Diagnostic Approach
Clinically, a ganglion cyst typically presents as a:
- Visible Lump: A smooth, well-defined, tumor-like swelling of a round or oval shape.
- Consistency: Usually firm, tense, or rubbery to dense consistency, though some may feel softer if less fluid-filled.
- Skin: The overlying skin is generally normal in appearance and mobile over the cyst.
- Size: Diameter can range from small (0.5 cm) to relatively large (3 cm or more). The size can fluctuate, sometimes increasing with activity and decreasing with rest.
- Mobility: The cyst itself is often relatively mobile over deeper structures but is typically fixed at its base, connected by a stalk to the underlying joint capsule or tendon sheath.
- Symptoms:
- Many ganglion cysts are asymptomatic apart from their appearance.
- Pain or Discomfort: Local soreness or aching pain in the tissues around the ganglion cyst may be noted, especially with movement, pressure, or if the cyst compresses adjacent nerves or tendons.
- Weakness or Restricted Motion: Large cysts or those in critical locations can sometimes cause weakness or limit the range of motion of the affected joint.
- Sensory Changes: Rarely, if a cyst presses on a nerve, symptoms like tingling, numbness, or weakness in the distribution of that nerve can occur.
- Transillumination: Many ganglion cysts will transilluminate (light passes through them when a penlight is held against the skin), indicating their fluid-filled nature. Solid tumors will not transilluminate.
Diagnosis is often made based on clinical examination. However, imaging may be used if the diagnosis is uncertain or to evaluate the cyst's origin and relationship to surrounding structures:
- Ultrasound: Can confirm the cystic nature of the lesion, visualize its stalk connecting to a joint or tendon sheath, and rule out solid masses or vascular abnormalities.
- X-rays: Usually normal but can help rule out underlying bony pathology or arthritis.
- Magnetic Resonance Imaging (MRI): Provides detailed images of soft tissues and is useful for complex or deep-seated ganglia, or if other pathology is suspected.
Treatment Options for Ganglion Cysts
Treatment for ganglion cysts depends on the presence and severity of symptoms, the size and location of the cyst, and patient preference. Many asymptomatic ganglia do not require treatment and may resolve spontaneously over time, though this is unpredictable.
Conservative and Historical Approaches
- Observation: If the cyst is small, painless, and not causing functional impairment, a "watchful waiting" approach is often appropriate.
- Immobilization: Resting the affected joint and using a splint or brace can sometimes help reduce irritation and may lead to a decrease in cyst size, especially if related to overuse.
- Blunt Crushing (Historical): In the past, a common "treatment" was to forcefully crush or rupture the ganglion cyst by striking it with a heavy object (e.g., a book, hence the historical term "Bible cyst" or "Gideon's disease"). This method is painful, often provides only temporary resolution (as the cyst wall remains and can refill), and carries a risk of injury to surrounding tissues. It is not a recommended medical treatment today due to its ineffectiveness and potential for harm, with frequent relapses.
Aspiration
Puncture and aspiration of the ganglion cyst's contents involves inserting a needle into the cyst and withdrawing the thick, gelatinous fluid. This can decompress the cyst and relieve symptoms. It is a relatively simple office procedure.
- Procedure: After aspiration, an injection of a corticosteroid into the cyst cavity is sometimes performed to try to reduce inflammation and the likelihood of recurrence, though evidence for the benefit of steroid injection is mixed.
- Recurrence: Aspiration alone has a relatively high recurrence rate (reported as high as 50% or more) because the cyst wall and its connection to the joint or tendon sheath remain.
Surgical Excision (Ganglionectomy)
Surgical removal of the ganglion cyst (ganglionectomy) is the most definitive treatment and offers the lowest recurrence rate. It is typically considered for cysts that are persistently painful, cause functional impairment, are cosmetically unacceptable, or have recurred after aspiration.
- Procedure: The operation is usually performed under local, regional, or general anesthesia on an outpatient basis. The essence of the operation is to carefully dissect and exfoliate the entire ganglion cyst, including its stalk and its attachment to the joint capsule or tendon sheath. Complete removal of the stalk and a small portion of the adjacent capsule/sheath is crucial to minimize recurrence. The wound is then closed with sutures.
- Arthroscopic Excision: For some wrist ganglia, arthroscopic (keyhole) surgery can be used for removal.
Post-Treatment Care and Physiotherapy
Following treatment, particularly surgical excision or sometimes aspiration, a period of supportive care may be recommended:
- Immobilization: After surgical treatment, wearing a fixation splint or compressive bandage for a short period (e.g., a week, or 2-3 days after aspiration) may be advised to support the area and reduce swelling.
- Physiotherapy: A course of physiotherapy, such as UHF (Ultra-High Frequency) therapy or other modalities, may be prescribed to help reduce swelling, inflammation, and soreness, and to restore the full range of motion in the affected joint, particularly after surgery for wrist or hand ganglion cysts.
The specific therapeutic actions chosen depend on the size of the ganglion cyst and the severity of symptoms. Options range from observation for asymptomatic cysts to aspiration or surgical excision for symptomatic ones.
The application of physiotherapy modalities can accelerate the reduction of swelling, inflammation, and soreness, as well as help restore the range of motion in the wrist and hand area following treatment for a ganglion cyst.
A fixation splint may be applied to the wrist joint after surgical treatment of a ganglion cyst to provide support and limit movement during the initial healing phase. (Image illustrative of a splint, not specific to ganglion cyst).
Differential Diagnosis of Periarticular Lumps
A ganglion cyst needs to be differentiated from other conditions that can cause lumps or swelling around joints and tendons:
| Condition | Key Differentiating Features |
|---|---|
| Ganglion Cyst | Well-defined, firm or fluctuant, often transilluminates. Typically arises from joint capsule or tendon sheath. Common on wrist/hand/foot. Gelatinous contents on aspiration. |
| Lipoma | Soft, doughy, lobulated subcutaneous fatty tumor. Not attached to underlying joint/tendon. Does not transilluminate. |
| Epidermoid or Pilar Cyst (Sebaceous Cyst) | Dermal or subcutaneous cyst filled with keratin. Often has a central punctum (epidermoid). More attached to skin. |
| Tenosynovitis (Inflamed Tendon Sheath) | Swelling and tenderness along the course of a tendon. Pain with movement of that tendon. May be crepitus. Less discrete and well-rounded than a ganglion. |
| Bursitis | Inflammation of a bursa. Localized swelling, tenderness, pain with specific movements. Bursa is a distinct anatomical sac. |
| Rheumatoid Nodule | Firm, subcutaneous nodules, often over extensor surfaces or pressure points in patients with rheumatoid arthritis. |
| Gouty Tophus | Deposit of urate crystals in soft tissues, often near joints, in patients with chronic gout. Can be firm, may discharge chalky material. |
| Benign Soft Tissue Tumors (e.g., Fibroma, Neurofibroma, Giant Cell Tumor of Tendon Sheath) | Vary in consistency and location. Usually solid on ultrasound/MRI. Biopsy may be needed for diagnosis. |
| Malignant Soft Tissue Tumors (e.g., Sarcoma) | Rare. Often larger, rapidly growing, may be painful, fixed to deeper structures. Requires urgent evaluation and biopsy. |
| Aneurysm or Vascular Malformation | Pulsatile mass if arterial aneurysm. Vascular malformations can be soft and compressible. Doppler ultrasound or angiography for diagnosis. |
Potential Complications and Recurrence
While ganglion cysts are benign, potential issues include:
- Pain and Discomfort: Especially with activity or if pressing on nerves/tendons.
- Nerve Compression: Can cause sensory changes (numbness, tingling) or motor weakness if a nerve is significantly compressed (e.g., ulnar nerve compression by a ganglion at Guyon's canal in the wrist).
- Restricted Motion or Weakness: Large cysts can mechanically interfere with joint or tendon movement.
- Cosmetic Concerns.
- Recurrence: This is the most common "complication," especially after aspiration (up to 50% or higher). Surgical excision has a lower recurrence rate (typically 5-15%) if the cyst stalk and its origin are completely removed.
- Complications of Treatment:
- Aspiration: Infection (rare), pain, bruising, temporary nerve irritation.
- Surgery: Infection, bleeding, scar formation, nerve or tendon injury, joint stiffness, recurrence.
When to Seek Medical Attention
Medical evaluation by a primary care physician, orthopedist, or hand/foot specialist is recommended if a ganglion cyst:
- Causes significant pain or discomfort.
- Interferes with daily activities or joint function.
- Causes numbness, tingling, or weakness.
- Is rapidly increasing in size.
- Is cosmetically unacceptable to the patient.
- The diagnosis is uncertain, and other conditions need to be ruled out.
A healthcare professional can confirm the diagnosis and discuss appropriate management options.
References
- Gude W, Morelli V. Ganglion cysts: aetiology, clinical presentation, and management. Curr Rev Musculoskelet Med. 2008 Dec;1(3-4):205-11.
- Thornburg LE. Ganglions of the hand and wrist. J Am Acad Orthop Surg. 1999 Jul-Aug;7(4):231-8.
- Minotti P, Taras JS. Ganglion cysts of the wrist. J Am Soc Surg Hand. 2002;2(3):102-107.
- Seradge H, Kutz JA, Kleinert HE, Lister GD, Wolff TW, Atasoy E. Peritendinous fibrosis and the carpal tunnel syndrome. J Hand Surg Am. 1984 May;9(3):360-4. (Context for wrist soft tissue issues).
- Wright TW, Cooney WP 3rd, Stans AA. Treatment of ganglion cysts of the hand and wrist. J Am Acad Orthop Surg. 1994 Jan;2(1):32-40.
- Nahra ME, Bucchieri JS. Ganglion cysts and other tumor related conditions of the hand and wrist. Hand Clin. 2004 Aug;20(3):249-60, v.
- Ahn KS, Lee SW, Kim YJ, Lee YH. Outcome of Surgical Excision of Dorsal Wrist Ganglion and Analysis of Recurrence. J Hand Surg Asian Pac Vol. 2016 Sep;21(3):377-81.
See also
- Abscess
- Breast diseases (mastopathy, cyst, calcifications, fibroadenoma, intraductal papilloma, cancer)
- Bursitis
- Furuncle (boil)
- Ganglion cyst
- Hidradenitis suppurativa (HS)
- Ingrown toenail
- Lipoma (fatty tumor)
- Lymphostasis
- Paronychia, panaritium (whitlow or felon)
- Sebaceous cyst (epidermoid cyst)
- Tenosynovitis (infectious, stenosing)