Tenosynovitis (infectious, stenosing)
What is Tenosynovitis?
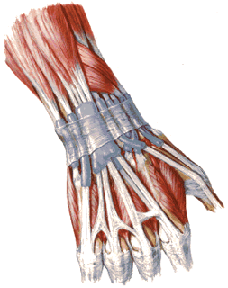
Tenosynovitis is the inflammation of the fluid-filled sheath (the synovium) that surrounds a tendon (1, 2). Tendons are cords of tissue that connect muscles to bones, and the synovial sheath produces fluid to help the tendon glide smoothly during movement. When this sheath becomes inflamed, it can cause pain, swelling, and difficulty moving the associated joint or limb.
Tenosynovitis commonly affects the tendons around the wrist, hand, fingers, ankle, and foot (1). While the term is sometimes used broadly, specific types exist based on the cause and presentation.
Types of Tenosynovitis
Tenosynovitis can be broadly categorized based on its cause and characteristics:
Infectious Tenosynovitis
This is a serious condition caused by bacteria entering the tendon sheath, often through a puncture wound, cut, bite, or spread from a nearby infection (e.g., felon, paronychia) (3, 4). It most commonly affects the flexor tendons of the hand.
- Symptoms: Rapid onset of severe pain, uniform swelling along the affected finger/tendon path, significant pain with passive extension of the digit, and the finger held in a slightly flexed position (Kanavel's signs) (3, 4). Fever and signs of systemic illness may be present.
- Importance: This is a surgical emergency requiring prompt diagnosis and treatment to prevent tendon necrosis, adhesion formation, and permanent loss of function (3).
Non-Infectious Inflammatory Tenosynovitis
This type occurs as part of a systemic inflammatory condition, such as (1):
- Rheumatoid Arthritis (RA)
- Psoriatic Arthritis
- Gout
- Other connective tissue diseases
Inflammation is driven by the underlying autoimmune or inflammatory process. Symptoms often include pain, swelling, stiffness, and sometimes warmth over the affected tendon sheaths, often occurring symmetrically or in multiple locations.
Stenosing Tenosynovitis
This category involves a mechanical issue where the tendon cannot glide smoothly within its sheath due to thickening of the tendon, the sheath, or a nearby ligamentous structure (retinaculum) creating constriction (1, 5). It's often related to repetitive use or anatomical factors. Key examples include:
- De Quervain's Tenosynovitis: Affects the tendons on the thumb side of the wrist (abductor pollicis longus and extensor pollicis brevis within the first dorsal compartment). Causes pain and tenderness at the radial styloid, worsened by thumb and wrist movements (5).
- Trigger Finger/Thumb (Stenosing Flexor Tenosynovitis): Affects the flexor tendons of the fingers or thumb as they pass through a pulley system (typically the A1 pulley) at the base of the digit. The tendon or pulley thickens, causing catching, locking, or snapping (triggering) during finger flexion/extension, often accompanied by pain (1, 5).
Crepitating Tenosynovitis
Also known as acute non-specific or friction tenosynovitis, this type is typically caused by acute overuse or repetitive friction between a tendon and its sheath, often without significant underlying constriction (1). It commonly affects the extensor tendons of the forearm, particularly near the wrist.
- Symptoms: Characterized by pain, swelling, and a distinctive palpable or audible grating sensation (crepitus) with tendon movement (1).
- Cause: Often seen in individuals starting new, repetitive tasks (e.g., typing, manual labor, sports like rowing).
Causes and Risk Factors
Specific causes vary by type:
- Infectious: Bacterial inoculation (Staphylococcus aureus and Streptococcus species are common) via trauma (3, 4).
- Inflammatory: Underlying systemic autoimmune/inflammatory disease (1).
- Stenosing/Crepitating: Repetitive strain, overuse, awkward postures, direct trauma, hormonal changes (e.g., pregnancy/postpartum for De Quervain's), diabetes (increases risk of trigger finger) (1, 5).
Symptoms
Common symptoms across types include (1, 2):
- Pain along the affected tendon, worsened by movement.
- Swelling and tenderness over the tendon sheath.
- Difficulty moving the affected joint or digit.
- Redness and warmth (especially in infectious or acute inflammatory types).
- Specific signs:
- Infectious: Kanavel signs (flexed posture, fusiform swelling, tenderness along sheath, pain on passive extension) (3, 4).
- Crepitating: Palpable/audible crepitus or grating with movement (1).
- Stenosing (Trigger Finger): Catching, locking, popping, palpable nodule (1, 5).
- Stenosing (De Quervain's): Pain at radial wrist, positive Finkelstein's test (5).
Diagnosis
Diagnosis relies heavily on clinical history and physical examination, supplemented by investigations as needed (1, 2):
- History: Onset of symptoms, location/character of pain, aggravating/relieving factors, presence of trauma/infection risk, occupational/recreational activities, history of inflammatory diseases.
- Physical Examination:
- Inspection: Looking for swelling, redness, deformity, posture of digits.
- Palpation: Identifying precise areas of tenderness, warmth, swelling, crepitus, or nodules.
- Range of Motion: Assessing active and passive movement, pain reproduction, specific provocative tests (e.g., Finkelstein's test for De Quervain's, checking for triggering in trigger finger, pain on passive extension for infectious) (3, 5).
- Neurological/Vascular assessment: Especially important in infectious cases or if nerve involvement is suspected.
- Laboratory Tests:
- For suspected infectious tenosynovitis: Complete blood count (CBC), inflammatory markers (ESR, CRP), blood cultures. Fluid aspirated from the sheath should be sent for Gram stain, culture, and sensitivity (3).
- For suspected inflammatory tenosynovitis: Tests related to underlying conditions (e.g., RF, anti-CCP, ANA, uric acid).
- Imaging Studies:
- Ultrasound: Often very useful for non-infectious types. Can show sheath thickening, fluid accumulation (effusion), hyperemia (increased blood flow on Doppler), tendon thickening/tears, and dynamic assessment of tendon gliding or triggering (1, 6). Can guide injections.
- X-rays: Primarily used to rule out fractures, foreign bodies, or bone/joint involvement (e.g., arthritis, osteomyelitis).
- MRI: Can provide detailed images of tendons, sheaths, and surrounding structures but is less commonly needed than ultrasound unless diagnosis is unclear or complications are suspected (1).
Treatment
Treatment depends heavily on the specific type and severity of tenosynovitis.
Infectious Tenosynovitis Treatment
This requires urgent management (3, 4):
- Hospital Admission: Usually required.
- Antibiotics: Broad-spectrum intravenous (IV) antibiotics initially, tailored based on culture results.
- Surgical Drainage and Irrigation: Prompt surgical intervention is often necessary to drain pus and irrigate the tendon sheath thoroughly.
- Immobilization: Splinting the affected hand/limb in a safe position.
- Elevation: To reduce swelling.
- Hand Therapy: Early controlled motion exercises after infection control to prevent adhesions and stiffness.
Prevention includes proper wound care and early treatment of local infections (e.g., paronychia, felon).
Non-Infectious / Crepitating Tenosynovitis Treatment
Focuses on reducing inflammation and friction (1, 2):
- Rest/Activity Modification: Avoiding aggravating activities.
- Immobilization: Splinting the affected area (e.g., wrist brace, ankle brace) to allow the tendon sheath to rest.
- NSAIDs: Oral or topical anti-inflammatory medications.
- Ice Application: To reduce pain and swelling.
- Physical Therapy (Physiotherapy): Modalities like ultrasound or iontophoresis may be used initially. Later, focus on gentle stretching and gradual strengthening. Ergonomic assessment and modification may be beneficial.
- Corticosteroid Injection: Occasionally used for persistent inflammation, but often less effective for purely friction-based types than for stenosing or inflammatory types.
Stenosing Tenosynovitis Treatment
Aimed at relieving the constriction (1, 5):
- Activity Modification/Splinting: Reducing repetitive motions, using thumb spica splints for De Quervain's or avoiding gripping for trigger finger.
- NSAIDs: May provide some pain relief but don't address the mechanical issue effectively.
- Corticosteroid Injection: Often the first-line treatment for both De Quervain's and trigger finger. Injection into the affected tendon sheath/compartment can reduce inflammation and thickening, often providing significant relief. May need repeating.
- Surgical Release: If conservative measures and injections fail, surgery to release the constricted compartment (De Quervain's) or the A1 pulley (trigger finger) is highly effective.
Late or inadequate treatment of non-infectious types, especially stenosing forms, can lead to persistent pain, reduced function, and sometimes tendon degeneration or rupture.
Differential Diagnosis
Conditions that can mimic tenosynovitis include (1, 2):
| Condition | Key Differentiating Features |
|---|---|
| Tendinopathy/Tendinitis | Inflammation or degeneration within the tendon substance itself, not primarily the sheath. Pain is localized to the tendon. Swelling may be less diffuse than tenosynovitis. |
| Arthritis | Inflammation within the joint itself. Pain and swelling localized to the joint line, restricted joint motion (not just tendon glide). X-rays may show joint changes. |
| Nerve Entrapment | (e.g., Carpal Tunnel Syndrome, Tarsal Tunnel Syndrome). Pain often described as burning, tingling, numbness. Symptoms follow nerve distribution. May have positive provocative tests (Phalen's, Tinel's). |
| Ganglion Cyst | Fluid-filled sac arising from a joint capsule or tendon sheath. Usually presents as a distinct, palpable lump, often near the wrist. Can sometimes cause dull ache or nerve compression. |
| Cellulitis/Abscess | Superficial skin infection or localized collection of pus. Presents with redness, warmth, swelling, tenderness more localized to skin/subcutaneous tissue than along a tendon sheath. May have fever. Different from deep infectious tenosynovitis. |
| Bursitis | Inflammation of a bursa (fluid sac cushioning joints/tendons). Localized pain and swelling over the bursa (e.g., olecranon, prepatellar, retrocalcaneal). |
References
- Abrams RA, Brown RA, Botte MJ. The pathogenesis and treatment of tendinitis and tenosynovitis. Instr Course Lect. 1999;48:275-286. (General overview)
- Cluett J. Overview of Tenosynovitis. Verywell Health. Updated November 08, 2023. (Patient-level resource example, check date/accuracy) - *Replace with more robust medical source if possible.*
- Pang HN, Teoh LC, Yam AK, Lee JY, Puhaindran ME, Tan AB. Factors affecting the prognosis of pyogenic flexor tenosynovitis. J Bone Joint Surg Br. 2007;89(12):1742-1745. doi:10.1302/0301-620X.89B12.19847
- Kennedy CD, Lauder AS, Pribaz JR, Kennedy SA. Infectious Flexor Tenosynovitis. Hand Clin. 2017;33(3):445-454. doi:10.1016/j.hcl.2017.04.004
- Ryzewicz M, Wolf JM. Trigger digits: principles, management, and complications. J Hand Surg Am. 2006;31(1):135-146. doi:10.1016/j.jhsa.2005.09.009 (Covers Trigger Finger and De Quervain's mentioned within)
- Grassi W, Filippucci E, Farina A, Cervini C. Sonography of the wrist and hand. Semin Musculoskelet Radiol. 2001;5(2):173-186. doi:10.1055/s-2001-15692 (Covers ultrasound utility)
See also
- Achilles tendon inflammation (paratenonitis, ahillobursitis)
- Achilles tendon injury (sprain, rupture)
- Ankle and foot sprain
- Arthritis and arthrosis (osteoarthritis):
- Autoimmune connective tissue disease:
- Bunion (hallux valgus)
- Epicondylitis ("tennis elbow")
- Hygroma
- Joint ankylosis
- Joint contractures
- Joint dislocation:
- Knee joint (ligaments and meniscus) injury
- Metabolic bone disease:
- Myositis, fibromyalgia (muscle pain)
- Plantar fasciitis (heel spurs)
- Tenosynovitis (infectious, stenosing)
- Vitamin D and parathyroid hormone