Knee joint (ligaments and meniscus) injury
Knee Ligament and Meniscus Injuries: Overview & Causes
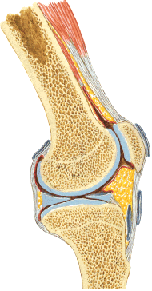
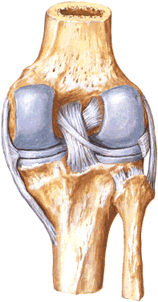
Injuries to the ligaments (sprains or tears) and menisci (cartilage tears) of the knee joint are extremely common, particularly in sports and daily activities [1]. The knee relies on a complex interplay of ligaments (ACL, PCL, MCL, LCL) and the menisci for stability and smooth function [2].
The most frequent mechanism involves indirect trauma, often a twisting force on a planted foot or a valgus/varus stress (force applied to the side of the knee) [1]. Common scenarios include:
- Twisting or pivoting maneuvers (common in soccer, basketball, skiing).
- Sudden stops or changes in direction.
- Landing awkwardly from a jump.
- Direct blows to the knee (less common for isolated ligament/meniscus tears, often causes fractures too).
- Falls, especially on slippery surfaces like ice ("podvertyvanie leg inwards or outwards" - twisting the leg inward or outward).
These forces can stretch or tear the stabilizing ligaments (collateral or cruciate) or pinch and tear the menisci between the femur and tibia [1].
Knee Ligament and Meniscus Injury: Diagnosis & Symptoms
Signs and symptoms suggesting injury to the knee ligaments or menisci include [1]:
- Localized Pain: Tenderness upon palpation over the specific ligament attachment points (e.g., medial/lateral joint line for collateral ligaments) or joint line (for meniscus).
- Pain Reproduction: Increased pain when stress is applied to the specific ligament (e.g., valgus stress for MCL, varus stress for LCL) or during maneuvers testing the meniscus (e.g., McMurray test).
- Swelling (Effusion): Accumulation of fluid within the joint. Rapid swelling with significant blood (hemarthrosis) often indicates a more severe injury like an ACL tear or peripheral meniscus tear. Gradual swelling suggests synovitis or smaller tears.
- Bruising (Ecchymosis): May develop around the knee.
- Instability: A feeling of the knee "giving way," buckling, or shifting, particularly with ligament tears (e.g., ACL, PCL).
- Mechanical Symptoms: Clicking, catching, or locking (inability to fully straighten or bend the knee) strongly suggest a meniscal tear, particularly a displaced bucket-handle tear.
- Audible "Pop" or "Crack": Often reported by patients at the time of significant ligament rupture (especially ACL).
Clinical examination involves specific tests to assess ligament integrity (Lachman, drawer tests, varus/valgus stress) and meniscal pathology (joint line tenderness, McMurray's, Thessaly tests) [1].
Imaging Diagnosis [1, 3]:
- X-rays: Primarily used to rule out fractures (e.g., tibial plateau, distal femur, patella, avulsion fractures like Segond fracture associated with ACL tears). Usually normal in isolated ligament/meniscus tears.
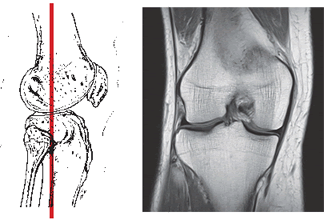
- MRI: The gold standard for visualizing soft tissues. Confirms ligament tears (partial or complete), meniscus tears (type and location), cartilage damage, and bone bruising (bone marrow edema).
- CT Scan: Less useful for soft tissues; primarily for evaluating complex fractures.
Bone marrow edema (BME) seen on MRI is fluid accumulation within the bone, often indicating microfractures (bone bruise) associated with acute trauma (ligament tears, impaction) or sometimes related to osteoarthritis or stress reactions [3]. Its presence can correlate with pain severity and associated structural damage.
Differential Diagnosis of Acute Knee Injury
| Condition | Key Features / Distinguishing Points | Typical Investigations / Findings |
|---|---|---|
| Ligament Sprain/Tear (ACL, PCL, MCL, LCL) | Specific mechanism (pivot, hyperextension, valgus/varus). Feeling of instability, "pop". Effusion (often large hemarthrosis with ACL). Pain localized to ligament. | Positive clinical stability tests (Lachman, drawer, varus/valgus). X-ray usually normal (may show avulsion). MRI confirms tear grade/location. |
| Meniscal Tear | Twisting injury often. Joint line pain, clicking, catching, locking, giving way. Effusion variable. | Joint line tenderness. Positive McMurray's/Thessaly tests. MRI confirms tear type/location. X-ray usually normal. |
| Tibiofemoral Dislocation | High-energy trauma. Gross deformity, severe instability. High risk of neurovascular injury. | X-ray shows dislocation. Urgent reduction & vascular assessment essential. MRI shows multi-ligament rupture. |
| Patellar Dislocation/Subluxation | Twisting injury or direct blow. Patella visibly displaced laterally (if not reduced). Feeling kneecap "popped out". Medial tenderness/swelling. Apprehension. | Clinical diagnosis/history. X-ray confirms position, rules out fracture. MRI assesses MPFL/cartilage. |
| Knee Fracture (Tibial Plateau, Distal Femur, Patella) | Significant trauma usually. Marked pain, swelling, hemarthrosis, inability to bear weight. Bony tenderness. | X-ray confirms fracture. CT often needed for articular involvement/surgical planning. |
| Patellar/Quadriceps Tendon Rupture | Sudden force (jump/fall). Inability to actively extend knee. Palpable tendon defect. Abnormal patellar position on X-ray. | Clinical exam. X-ray. Ultrasound/MRI confirms rupture. |
| Osteochondral Defect / Loose Body | Pain, swelling, catching, locking. May follow trauma or occur spontaneously (OCD). | X-ray may show loose body or defect. MRI confirms cartilage/bone lesion. |
Knee Joint (Ligaments and Meniscus) Injury: First Aid and Treatment
First Aid (Acute Phase): For suspected sprains or tears, immediate management follows the RICE principle [1]:
- Rest: Avoid weight-bearing (use crutches if necessary).
- Ice: Apply cold packs (wrapped in a towel) for 15-20 minutes every 2-3 hours to reduce pain and swelling.
- Compression: Use an elastic bandage to control swelling.
- Elevation: Keep the knee elevated above heart level.
Seeking prompt medical evaluation is important to rule out fractures and determine the severity of the injury.
Treatment: Varies based on the specific structure injured and the severity of the tear/sprain [1, 4].
- Mild Sprains (Grade I): Usually managed conservatively with RICE, bracing (knee holder/brace), pain control (NSAIDs), and early rehabilitation (therapeutic exercises, physiotherapy). Return to activity within weeks.
- Moderate-Severe Sprains/Tears (Grade II/III Ligaments, Significant Meniscus Tears):
- May require longer immobilization (brace, sometimes cast).
- Formal rehabilitation program is crucial.
- Aspiration of large hemarthrosis may be performed for comfort.
- Physiotherapy modalities (UHF, electrophoresis, heat/cold) can manage pain/swelling.
- Therapeutic injections (e.g., local anesthetic/corticosteroid block) might be used for persistent localized pain, but corticosteroids near ligaments/tendons require caution.
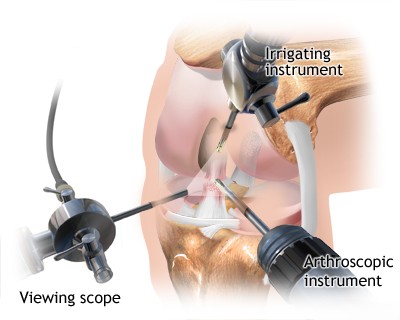
- Surgery (arthroscopy): Often indicated for complete ACL tears (especially in active individuals), displaced meniscus tears (causing locking), complex multi-ligament injuries, or injuries failing conservative management. Procedures include ligament reconstruction (using grafts) or meniscal repair/debridement.
Treatment for bone marrow edema (bone bruising) is typically conservative, focusing on protected weight-bearing and addressing the underlying cause (e.g., treating the associated ligament/meniscus injury). Weight loss is important if obesity is a factor [1].
References
- Skinner HB, McMahon PJ. Current Diagnosis & Treatment in Orthopedics. 5th ed. McGraw Hill; 2014. Chapter 7: Knee & Leg Trauma.
- Drake RL, Vogl W, Mitchell AWM. Gray's Anatomy for Students. 4th ed. Elsevier; 2019. Chapter 6: Lower Limb (Section on Knee Joint).
- Resnick D, Kransdorf MJ. Bone and Joint Imaging. 3rd ed. Elsevier Saunders; 2005. Chapter on Knee Imaging.
- Canale ST, Beaty JH. Campbell's Operative Orthopaedics. 13th ed. Elsevier; 2017. Sections on Knee Injuries, Ligament Reconstruction, Meniscal Surgery, Arthroscopy.
See also
- Achilles tendon inflammation (paratenonitis, ahillobursitis)
- Achilles tendon injury (sprain, rupture)
- Ankle and foot sprain
- Arthritis and arthrosis (osteoarthritis):
- Autoimmune connective tissue disease:
- Bunion (hallux valgus)
- Epicondylitis ("tennis elbow")
- Hygroma
- Joint ankylosis
- Joint contractures
- Joint dislocation:
- Knee joint (ligaments and meniscus) injury
- Metabolic bone disease:
- Myositis, fibromyalgia (muscle pain)
- Plantar fasciitis (heel spurs)
- Tenosynovitis (infectious, stenosing)
- Vitamin D and parathyroid hormone