Vitamin D and parathyroid hormone
Overview: Calcium Homeostasis
Maintaining stable levels of calcium and phosphate in the blood (calcium and phosphate homeostasis) is vital for numerous physiological processes, including nerve function, muscle contraction, blood clotting, and particularly, bone health (mineralization and structure). This delicate balance is primarily regulated by the interplay between Vitamin D and Parathyroid Hormone (PTH), acting mainly on the intestines, kidneys, and bones (1, 2).
Vitamin D: Synthesis, Activation, and Function
Vitamin D is a group of fat-soluble secosteroids that functions as a hormone. The two major forms are:
- Vitamin D3 (cholecalciferol): Synthesized in the skin from 7-dehydrocholesterol upon exposure to ultraviolet B (UVB) sunlight. It is also obtained from dietary sources like fatty fish, egg yolks, and fortified foods (1, 3).
- Vitamin D2 (ergocalciferol): Primarily obtained from dietary sources, such as fortified foods and some plants/fungi (1).
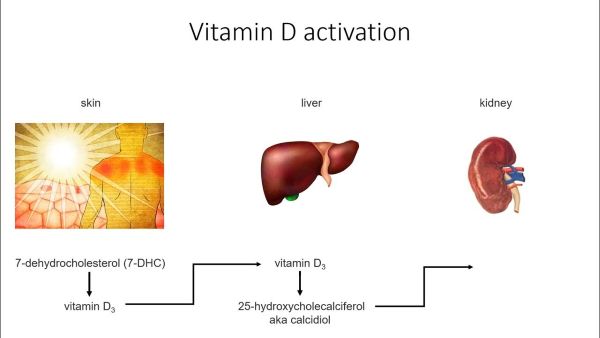
Both D2 and D3 are biologically inactive initially. They require two hydroxylation steps for activation (1, 3):
- First Hydroxylation (Liver): Vitamin D (D2 or D3) is transported to the liver and converted to 25-hydroxyvitamin D [25(OH)D] (calcifediol). This is the major circulating form of Vitamin D and the best indicator of overall Vitamin D status.
- Second Hydroxylation (Kidneys): 25(OH)D travels to the kidneys, where the enzyme 1-alpha-hydroxylase converts it to the biologically active form, 1,25-dihydroxyvitamin D [1,25(OH)2D] (calcitriol). This step is tightly regulated, primarily stimulated by PTH and low phosphate levels (1, 2).
Biological Functions of Active Vitamin D (Calcitriol):
- Increases Intestinal Calcium Absorption: Its primary role is to enhance the absorption of dietary calcium (and phosphate) from the small intestine (1, 2).
- Regulates Bone Metabolism: Promotes mineralization of the bone matrix (osteoid) by ensuring adequate calcium and phosphate supply. At high levels (often pharmacological or in severe deficiency states with secondary hyperparathyroidism), it can work with PTH to increase bone resorption, releasing calcium and phosphate into the blood (1).
- Influences Kidney Function: Works with PTH to modulate calcium and phosphate reabsorption in the kidney tubules (1).
- Other Roles: Involved in immune function, cell differentiation, and regulation of various other cellular processes (3).
Parathyroid Hormone (PTH): Synthesis and Function
Parathyroid Hormone (PTH), also known as parathormone, is a peptide hormone produced and secreted by the four small parathyroid glands located in the neck, usually behind the thyroid gland (2, 4).
Regulation of Secretion: The primary regulator of PTH secretion is the level of ionized calcium in the blood. Low calcium levels stimulate PTH release, while high calcium levels suppress it. Vitamin D (calcitriol) also provides negative feedback, suppressing PTH synthesis and secretion (1, 2, 4).
Biological Functions of PTH: PTH acts to increase blood calcium levels through its effects on target organs (2, 4):
- Kidneys:
- Increases calcium reabsorption in the distal tubules, reducing calcium loss in urine.
- Decreases phosphate reabsorption in the proximal tubules, increasing phosphate excretion in urine (phosphaturic effect).
- Stimulates the 1-alpha-hydroxylase enzyme, increasing the production of active Vitamin D (1,25(OH)2D) (1, 2).
- Bone:
- Stimulates bone resorption by increasing the activity and number of osteoclasts (cells that break down bone), releasing calcium and phosphate into the bloodstream (1, 4). While continuous high PTH leads to bone breakdown, intermittent low doses can paradoxically stimulate bone formation (basis for teriparatide therapy).
- Intestine (Indirect Effect): By stimulating the production of active Vitamin D, PTH indirectly increases intestinal calcium and phosphate absorption (1, 2).
The Vitamin D - PTH - Calcium Feedback Loop
These hormones function within a tightly regulated feedback system (1, 2):
- Low Blood Calcium: Detected by the parathyroid glands -> Increased PTH secretion.
- PTH Effects:
- Acts on kidneys -> Increases calcium reabsorption, increases phosphate excretion, stimulates 1-alpha-hydroxylase -> Increased active Vitamin D [1,25(OH)2D].
- Acts on bone -> Increases bone resorption -> Releases calcium and phosphate.
- Active Vitamin D Effects:
- Acts on intestines -> Increases calcium and phosphate absorption.
- Result: Blood calcium levels rise.
- Negative Feedback:
- Rising blood calcium -> Suppresses PTH secretion from parathyroid glands.
- Increased active Vitamin D -> Suppresses PTH synthesis/secretion and inhibits 1-alpha-hydroxylase activity in the kidney.
This intricate loop ensures that blood calcium levels are maintained within a narrow physiological range.
Measuring Vitamin D and PTH
- Vitamin D Status: Assessed by measuring serum 25-hydroxyvitamin D [25(OH)D] levels. This reflects Vitamin D obtained from both sun exposure and diet and has a relatively long half-life (1, 3). Measurement of the active form, 1,25(OH)2D, is usually reserved for specific clinical situations (e.g., suspected disorders of Vitamin D metabolism, chronic kidney disease).
- General consensus suggests levels <20 ng/mL (<50 nmol/L) indicate deficiency (1, 5).
- Levels between 20-29 ng/mL (50-74 nmol/L) may indicate insufficiency (1, 5).
- Levels ≥30 ng/mL (≥75 nmol/L) are often considered sufficient, though optimal levels are debated (1, 5).
- Levels >100 ng/mL (>250 nmol/L) may indicate potential toxicity (1).
- Parathyroid Hormone (PTH): Measured using immunoassays that typically detect the intact PTH molecule (iPTH) (4). Levels need to be interpreted in the context of simultaneous serum calcium levels (total and/or ionized).
Clinical Significance and Related Disorders
Vitamin D Deficiency/Insufficiency
- Causes: Inadequate sun exposure, insufficient dietary intake, malabsorption syndromes, certain medications, obesity, chronic kidney or liver disease (1, 3).
- Consequences: Impaired calcium absorption leads to low blood calcium -> stimulates PTH secretion (secondary hyperparathyroidism). Chronic high PTH increases bone turnover. In children, severe deficiency causes rickets (defective bone mineralization). In adults, it causes osteomalacia (softening of bones) and contributes to osteoporosis (reduced bone mass), increasing fracture risk (1, 3). Also linked to muscle weakness and potential non-skeletal health issues.
Hyperparathyroidism
- Primary Hyperparathyroidism: Inappropriate, excessive secretion of PTH, usually due to a parathyroid adenoma (benign tumor) or hyperplasia (gland enlargement). Leads to high blood calcium (hypercalcemia), low/normal phosphate, and potentially high urine calcium. Can cause bone pain, kidney stones, fatigue, constipation, depression, and osteoporosis (4, 6).
- Secondary Hyperparathyroidism: Appropriate physiological response to chronic low calcium or high phosphate levels, most commonly caused by Vitamin D deficiency or chronic kidney disease (CKD). PTH levels are elevated, but calcium is usually low or normal (until late stages of CKD) (1, 4). Treatment involves addressing the underlying cause (e.g., Vitamin D supplementation, phosphate binders in CKD).
- Tertiary Hyperparathyroidism: Occurs after prolonged secondary hyperparathyroidism (usually in severe CKD), where the parathyroid glands become autonomous and continue to secrete high levels of PTH even after the initial stimulus (like low calcium) is corrected (e.g., post-kidney transplant). Often results in persistent hypercalcemia (4).
Hypoparathyroidism
- Causes: Insufficient PTH secretion, most commonly due to accidental damage or removal of parathyroid glands during neck surgery (thyroidectomy, parathyroidectomy). Can also be autoimmune or genetic (4).
- Consequences: Low blood calcium (hypocalcemia) and high blood phosphate. Symptoms include tingling, muscle cramps (tetany), seizures, and cardiac arrhythmias (4). Requires treatment with calcium and active Vitamin D (calcitriol) or synthetic PTH.
Vitamin D Toxicity
- Causes: Rare, usually due to excessive intake of Vitamin D supplements (typically requires very high doses over prolonged periods) (1).
- Consequences: Leads to hypercalcemia (high blood calcium) due to increased intestinal absorption and bone resorption. Symptoms include nausea, vomiting, constipation, weakness, confusion, kidney stones, and potential kidney damage (1). Characterized by very high 25(OH)D levels (>100-150 ng/mL) and suppressed PTH.
Differential Diagnosis of Abnormal Levels
Interpreting PTH and Vitamin D levels requires considering serum calcium and phosphate:
- High PTH, High Calcium: Suggests Primary Hyperparathyroidism (or possibly tertiary).
- High PTH, Low/Normal Calcium: Suggests Secondary Hyperparathyroidism (check Vitamin D, kidney function).
- Low PTH, High Calcium: Suggests Hypercalcemia of Malignancy, Vitamin D toxicity, granulomatous disease (e.g., sarcoidosis), or other non-PTH mediated causes.
- Low PTH, Low Calcium: Suggests Hypoparathyroidism.
- Normal PTH, High Calcium: May occur in mild primary hyperparathyroidism or Familial Hypocalciuric Hypercalcemia (FHH).
- Normal PTH, Low Calcium: May suggest early Vitamin D deficiency or magnesium deficiency.
References
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281. doi:10.1056/NEJMra070553
- Goltzman D. Physiology of Parathyroid Hormone. Endocrinol Metab Clin North Am. 2018;47(4):743-758. doi:10.1016/j.ecl.2018.07.003
- Norman AW. From vitamin D to hormone D: fundamentals of the vitamin D endocrine system essential for good health. Am J Clin Nutr. 2008;88(2):491S-499S. doi:10.1093/ajcn/88.2.491S
- Potts JT Jr. Diseases of the parathyroid glands. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020:chap 29.
- Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Ross AC, Taylor CL, Yaktine AL, Del Valle HB, eds. Dietary Reference Intakes for Calcium and Vitamin D. National Academies Press (US); 2011. Available from: https://www.ncbi.nlm.nih.gov/books/NBK56070/
- Bilezikian JP, Brandi ML, Eastell R, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3561-3569. doi:10.1210/jc.2014-1413
See also
- Achilles tendon inflammation (paratenonitis, ahillobursitis)
- Achilles tendon injury (sprain, rupture)
- Ankle and foot sprain
- Arthritis and arthrosis (osteoarthritis):
- Autoimmune connective tissue disease:
- Bunion (hallux valgus)
- Epicondylitis ("tennis elbow")
- Hygroma
- Joint ankylosis
- Joint contractures
- Joint dislocation:
- Knee joint (ligaments and meniscus) injury
- Metabolic bone disease:
- Myositis, fibromyalgia (muscle pain)
- Plantar fasciitis (heel spurs)
- Tenosynovitis (infectious, stenosing)
- Vitamin D and parathyroid hormone