Joint dislocation
- Joint Dislocation Overview
- Traumatic Joint Dislocations
- Diagnosis and Symptoms of Joint Dislocation
- Clinical Manifestations and Outcomes of Joint Dislocation
- Traumatic Joint Dislocation Treatment
- Recurrent or Habitual Joint Dislocation
- Congenital Joint Dislocation
- Paralytic Joint Dislocation
- Pathological Joint Dislocation
- Differential Diagnosis of Joint Injury
Joint Dislocation Overview
Joint dislocation (Latin: luxatio) refers to the complete separation of the articular surfaces of bones that normally form a joint [1]. This typically involves damage, such as rupture, to the surrounding joint capsule and ligaments [1]. An incomplete dislocation, where the articular surfaces are only partially separated or shifted, is termed a subluxation [1]. If joint movement exceeds its normal physiological range, straining the capsule and ligaments, but the joint surfaces remain essentially in contact, it might be considered a severe sprain or momentary displacement rather than a true dislocation [1].
While the term "dislocation" can sometimes refer to the displacement of soft tissues like nerves or tendons, it usually implies the disruption of a bony articulation [1].
Joint dislocations are broadly classified based on their cause [1]:
Traumatic Joint Dislocations
Traumatic dislocations result from external forces exceeding the joint's normal structural limits [1]. Several factors predispose individuals to these injuries [1]:
- Gender & Activity: Men experience dislocations 4-5 times more often than women (except for jaw dislocations), likely due to higher participation in physical labor and contact sports.
- Age: Dislocations are most common between ages 20 and 60. Similar forces in individuals younger than 20 often result in epiphyseal separations (growth plate injuries), while in older adults, they more commonly cause fractures near the joint.
- Anatomy: Joints with inherent weaknesses (e.g., parts of the capsule not reinforced by ligaments or muscles) are more susceptible. Ball-and-socket joints like the shoulder, which allow extensive movement, are particularly prone to dislocation.
Joint dislocations are significantly less frequent than fractures overall (occurring roughly 1/9th as often) [1]. This highlights the relative stability of joints in the spine and lower limbs, which are adapted for weight-bearing. Conversely, the upper limbs, adapted for mobility rather than stability, account for over 90% of dislocations, often resulting from falls onto the hand [1].
The mechanism of traumatic dislocation typically involves three components [1]:
- External Force: Usually indirect (e.g., falling on an outstretched hand causing a shoulder dislocation). The force levers the bone beyond its normal range, impacting bony prominences or stretching ligaments until the capsule tears. The bone end then displaces through the capsular tear. Direct forces (a blow or push) can also cause dislocation, especially if directed towards a weak point, but are more likely to cause fractures.
- Leverage: The bones act as levers, with fulcrums created at bony edges or tight ligaments, forcing the joint apart.
- Muscle Contraction: Following the initial displacement, reflex muscle spasms pull on the displaced bone, often locking it into a characteristic abnormal position (typical dislocation). This muscle force is significant; reproducing dislocations on cadavers (lacking muscle tone) is much harder. In atypical dislocations, extensive capsular tearing allows variable muscle pulls to place the bone in unusual positions. Severe muscle contractions alone (e.g., during epileptic seizures) can sometimes cause dislocations.
Muscle action can also contribute to associated injuries, such as avulsion fractures where a tendon or ligament pulls off a piece of bone (e.g., greater tuberosity fracture with shoulder dislocation) [1].
Complications: Besides capsular and ligament tears, dislocations can be complicated by [1, 2]:
- Damage to surrounding muscles and tendons.
- Neurovascular Injury: Compression or tearing of nearby nerves (causing pain, numbness, tingling - traumatic neuropathy; or weakness/paralysis) and blood vessels (causing swelling, hematoma, or potentially limb-threatening ischemia).
- Open Dislocation: The displaced bone end penetrates the skin, creating an open wound and increasing infection risk.
- Associated Fractures (Fracture-Dislocation): Fractures of the articular surfaces or nearby bone structures can occur concurrently.
Diagnosis and Symptoms of Joint Dislocation
The diagnosis of a joint dislocation is often based on characteristic clinical findings [1, 2]:
- Pain: Usually severe at the time of injury, though ongoing pain might be less intense than a fracture unless movement is attempted.
- Deformity: The joint appears visibly out of shape, with abnormal positioning of the limb. Bony landmarks may be in unusual positions.
- Loss of Function: Inability to move the joint normally.
- Fixed Position: The limb is often held rigidly in an unnatural position due to muscle spasm and mechanical blockage.
- Springy Resistance: Attempts at passive movement meet with a characteristic elastic or springy resistance, distinguishing it from the crepitus (grating) or free mobility often found with fractures.
- Swelling & Bruising: While swelling occurs, significant bruising (hemorrhage) may be less pronounced than with fractures unless major vessels or associated fractures are present, as the intact (though torn) capsule can somewhat contain bleeding.
- Changes in Limb Length or Axis: The dislocated limb may appear shorter or longer, or angled abnormally, depending on the direction of displacement.
Radiographs (X-rays) are essential to confirm the diagnosis, determine the direction of dislocation, and rule out associated fractures [1, 2]. Multiple views are usually required.
Clinical Manifestations and Outcomes of Joint Dislocation
After successful reduction (realignment) of an uncomplicated dislocation, healing generally occurs well, similar to other soft tissue injuries [1]. Minor synovitis (joint inflammation) and effusion typically resolve within 2-3 weeks [1].
However, potential complications and long-term consequences exist [1, 2]:
- Recurrent (Habitual) Dislocation: If the joint capsule and ligaments heal in a stretched or weakened state (often due to inadequate immobilization or premature return to strenuous activity), the joint may become unstable and prone to redislocation with minimal force. Nerve damage leading to muscle weakness can also contribute.
- Chronic Dislocation: If a dislocation remains unreduced, the body may attempt to form a false joint (neoarthrosis) around the displaced bone end, with fibrous tissue filling the original joint socket. This may provide some limited, often painful, function.
- Stiffness/Restricted Motion: Prolonged immobilization or significant soft tissue damage can lead to joint stiffness (arthrofibrosis).
- Post-Traumatic Arthritis: Damage to the articular cartilage during the dislocation or subsequent instability can lead to premature degenerative arthritis.
- Avascular Necrosis (AVN): Disruption of blood supply to the bone end (especially in hip or talus dislocations) can cause bone death.
- Persistent Neuropathy: Nerve damage may not fully recover.
The prognosis for a fresh, uncomplicated dislocation treated promptly is generally favorable [1]. However, complications like associated fractures, significant ligamentous damage, nerve injury, or delayed treatment significantly worsen the outlook regarding return to full function and long-term joint health [1, 2]. Open dislocations carry the added risk of infection [1].
Traumatic Joint Dislocation Treatment
The primary treatment for an acute traumatic dislocation is urgent reduction (returning the bones to their normal alignment), followed by immobilization and subsequent rehabilitation [1, 2].
- Reduction (Repositioning):
- Timing: Should be performed as soon as possible. Delays increase muscle spasm, swelling, and difficulty, potentially compromising neurovascular structures. While some dislocations can be reduced after weeks, success rates decrease significantly over time (especially for lower limb & complex joints).
- Method: Specific techniques vary depending on the joint involved. The general principle is to reverse the mechanism of injury by applying traction and manipulative maneuvers to disengage the bone ends and guide them back into place. Gentle, steady movements are preferred over brute force.
- Anesthesia/Analgesia: Adequate pain relief and muscle relaxation (using procedural sedation, regional blocks, or general anesthesia) are crucial for successful and less traumatic reduction.
- Post-Reduction Assessment: After reduction, clinical stability, neurovascular status, and radiographic confirmation (X-rays) are essential.
- Immobilization: After reduction, the joint is immobilized (e.g., with a sling, splint, cast, or brace) to allow the torn capsule and ligaments to heal. Duration varies:
- Simple, stable dislocations: Often 1-3 weeks.
- More complex or unstable dislocations: May require 3-6 weeks or longer.
- Rehabilitation: Essential for restoring function and preventing complications. Begins after the immobilization period (or earlier with controlled motion braces). Includes:
- Progressive range-of-motion exercises.
- Strengthening exercises for surrounding muscles.
- Proprioceptive training (improving joint position sense).
- Therapeutic modalities (e.g., heat, ice).
- Physiotherapy: Modalities like Ultrasound (UHF), Shortwave Diathermy (SWD), Electrical Stimulation (SMT - Sinusoidal Modulated Currents) may be used to manage pain, swelling, and promote healing.
- Therapeutic Massage: Can help manage muscle soreness and stiffness during recovery.
Return to full activity, especially sports or heavy labor, should be gradual and only after sufficient healing and rehabilitation, typically taking several weeks to months [1]. Premature return increases the risk of re-injury and habitual dislocation [1].
Chronic/Irreducible Dislocations: Attempts at closed reduction may still be warranted for dislocations up to 1-2 months old, often requiring vigorous (but careful) manipulation under anesthesia to break adhesions [1]. If closed reduction fails, or if a functional neoarthrosis does not form, surgery may be considered [1]. Options include open reduction, osteotomy (bone cutting/realignment), or arthrodesis (joint fusion), depending on the joint and patient factors [1]. Surgery for chronic dislocations carries higher risks [1].
Complicated Dislocations: Associated fractures may require surgical fixation (ORIF) [1, 2]. Open dislocations require thorough debridement and antibiotic treatment [1]. Significant neurovascular injuries may necessitate specific surgical repair [1, 2].
Recurrent or Habitual Joint Dislocation
Habitual dislocations occur when a joint becomes unstable and repeatedly dislocates with minimal or no trauma [1]. This typically follows an initial traumatic dislocation where the capsule and ligaments healed insufficiently, remaining stretched or torn [1]. Contributing factors include inadequate initial immobilization, premature return to activity, inherent ligamentous laxity, or associated injuries like nerve damage causing muscle weakness (e.g., axillary nerve injury after shoulder dislocation) [1].
General factors like serious infections or poor nutrition might also weaken tissues and predispose to instability [1]. Habitual dislocations are most common in the shoulder, patella, thumb MCP joint, and occasionally the jaw [1].
Treatment often requires surgical intervention to restore stability by repairing or tightening the damaged ligaments and capsule (e.g., Bankart repair for shoulder, MPFL reconstruction for patella) [1, 2].
Congenital Joint Dislocation
Congenital dislocations are present at birth, resulting from abnormal joint development during gestation, distinct from dislocations caused by birth trauma [1]. Developmental Dysplasia of the Hip (DDH) is the most common example, occurring much more frequently in girls [1]. It involves inadequate formation of the acetabulum (hip socket) and/or femoral head [1].
Symptoms of DDH often become apparent when the child begins walking [1]:
- Limb length discrepancy (affected leg appears shorter).
- Asymmetric skin folds in the thigh or buttock.
- Limited hip abduction (difficulty spreading the legs).
- Waddling gait ("duck gait"), especially if bilateral.
- Positive Trendelenburg sign: When standing on the affected leg, the pelvis drops on the opposite side due to gluteal muscle insufficiency resulting from the abnormal hip mechanics.
- Increased lumbar lordosis (swayback) may develop as compensation.
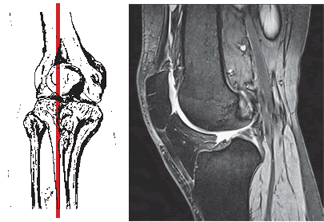
Diagnosis involves clinical examination (Ortolani, Barlow maneuvers in infants) and imaging (ultrasound in early infancy, X-rays after ~4-6 months) [1]. Early treatment (e.g., Pavlik harness) aims to achieve non-surgical reduction and allow normal joint development [1]. Reduction becomes more difficult with age as secondary changes occur (capsule constriction, muscle shortening) [1]. Closed or open reduction and casting (spica cast) may be needed in older infants or toddlers [1]. Untreated DDH leads to significant gait abnormalities, pain, and early arthritis [1].
Congenital dislocations can rarely affect other joints like the knee or shoulder, sometimes associated with birth injuries to nerves like the brachial plexus [1].
Paralytic Joint Dislocation
Paralytic dislocations occur when muscle paralysis around a joint leads to loss of dynamic stability [1]. The joint capsule stretches over time due to gravity and unopposed forces from remaining muscles, allowing the bones to displace [1]. This is most common in joints with wide ranges of motion like the shoulder and hip, often seen in conditions like poliomyelitis, stroke, or spinal cord injury [1].
Treatment focuses on managing the underlying neurological condition, bracing for support, and sometimes surgical procedures like tendon transfers or arthrodesis (joint fusion) to provide stability [1].
Pathological Joint Dislocation
Pathological dislocations result from weakening or destruction of the joint structures (bone, cartilage, capsule, ligaments) by an underlying disease process, such as [1]:
- Infection: Septic arthritis (bacterial infection) or tuberculosis can destroy articular cartilage and bone.
- Inflammatory Arthritis: Severe rheumatoid arthritis can erode bone and ligaments.
- Tumors: Bone tumors near the joint can weaken the bone structure.
- Neuropathic Arthropathy (Charcot Joint): Loss of sensation leads to repetitive trauma and joint destruction.
Muscle imbalance and contractures often contribute to the direction of displacement [1]. For example, in hip joint destruction (e.g., from infection or severe arthritis), muscle pull can cause superior migration of the femoral head [1]. In the knee, hamstring contractures can overpower weak quadriceps, leading to posterior subluxation of the tibia [1].
Diagnosis involves clinical assessment combined with imaging (X-ray, CT, MRI) to evaluate bone destruction and joint alignment [1]. Treatment primarily focuses on managing the underlying disease process [1]. Reduction maneuvers (redressation), traction, or bracing may be used to improve alignment, but stability is often compromised [1]. Definitive treatment might involve joint replacement (arthroplasty) or fusion (arthrodesis) once the underlying condition is controlled [1].
Differential Diagnosis of Acute Joint Injury
| Condition | Key Features / Distinguishing Points | Typical Investigations / Findings |
|---|---|---|
| Joint Dislocation | Obvious deformity, loss of normal joint contour, inability to move joint, severe pain, limb held in fixed/abnormal position. History of significant trauma. Springy block on passive motion. | X-ray confirms complete loss of contact between articular surfaces. Check neurovascular status. CT for associated fractures. |
| Joint Subluxation | Partial displacement of joint surfaces. Feeling of instability, "giving way", or "popping". May reduce spontaneously. Pain, swelling, limited motion. Deformity less obvious than dislocation. | Clinical exam shows laxity with stress testing. X-rays may be normal or show slight malalignment. Stress views or MRI can confirm instability/ligament injury. |
| Fracture (Intra-articular or Peri-articular) | Localized bony tenderness, pain, swelling, deformity, inability to bear weight/use limb. Crepitus (grating) may be present. Joint alignment may be preserved (unless fracture-dislocation). | X-ray shows fracture line. CT provides detail of fracture pattern, especially articular involvement. |
| Severe Ligament Sprain/Rupture | Significant pain, swelling, bruising, tenderness over ligament. Instability on stress testing. May have felt a "pop". No gross bony deformity. | Clinical exam is key. X-rays usually normal (may show avulsion). MRI confirms ligament tear and grade. |
| Tendon Rupture (e.g., Achilles, Biceps, Patellar) | Sudden pain, often feeling of being "hit" or "pop". Weakness/inability to perform specific movement associated with that tendon. Palpable defect in tendon. | Clinical exam demonstrates specific functional loss. Ultrasound or MRI confirms tendon rupture. X-ray may show related avulsion. |
| Septic Arthritis | Acute onset severe joint pain, swelling, warmth, redness, fever, chills. Marked limitation of active and passive motion due to pain. | Joint aspiration is diagnostic (high WBC count, positive Gram stain/culture). Elevated blood inflammatory markers (WBC, ESR, CRP). X-ray may show effusion/later joint space narrowing. |
| Acute Gout / Pseudogout | Sudden onset severe joint pain, swelling, redness, warmth (often MTP joint of big toe for gout). Resembles infection. | Joint aspiration shows crystals (urate for gout, CPPD for pseudogout). Serum uric acid may be high (gout). |
References
- Skinner HB, McMahon PJ. Current Diagnosis & Treatment in Orthopedics. 5th ed. McGraw Hill; 2014. Chapter 3: General Considerations of Musculoskeletal Trauma & Chapter on specific joint dislocations.
- Roberts DM, Khasriya R, Malone-Lee J. Joint Dislocations. BMJ Clin Evid. 2011;2011:1109. (General overview).
- Rockwood CA, Green DP, Bucholz RW, Heckman JD. Rockwood and Green's Fractures in Adults. 8th ed. Lippincott Williams & Wilkins; 2014. Relevant chapters on specific joint dislocations and fractures.
See also
- Achilles tendon inflammation (paratenonitis, ahillobursitis)
- Achilles tendon injury (sprain, rupture)
- Ankle and foot sprain
- Arthritis and arthrosis (osteoarthritis):
- Autoimmune connective tissue disease:
- Bunion (hallux valgus)
- Epicondylitis ("tennis elbow")
- Hygroma
- Joint ankylosis
- Joint contractures
- Joint dislocation:
- Knee joint (ligaments and meniscus) injury
- Metabolic bone disease:
- Myositis, fibromyalgia (muscle pain)
- Plantar fasciitis (heel spurs)
- Tenosynovitis (infectious, stenosing)
- Vitamin D and parathyroid hormone