Magnetic Resonance Imaging (MRI) of the Knee Joint
Understanding Magnetic Resonance Imaging (MRI) of the Knee Joint
Magnetic Resonance Imaging (MRI) of the knee joint is a highly advanced and non-invasive diagnostic imaging technique that utilizes strong magnetic fields, radiofrequency waves, and computer processing to create detailed, cross-sectional images of the knee's intricate structures. It is recognized as one of the most promising and rapidly improving methods in modern orthopedic and musculoskeletal diagnostics.
Principles and Diagnostic Capabilities
When performing an MRI of the knee joint, physicians gain the ability to thoroughly investigate not only structural abnormalities and pathological changes but also to evaluate certain physicochemical and pathophysiological processes within the entire knee joint or its specific components. This includes detailed visualization of:
- Menisci: The C-shaped cartilage discs that cushion the knee joint. MRI is highly sensitive for detecting meniscus tears, degeneration, and cysts.
- Ligaments: Including the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL). MRI can accurately diagnose sprains, partial tears, and complete ruptures.
- Articular Cartilage: The smooth hyaline cartilage covering the ends of the femur, tibia, and patella. MRI can detect cartilage thinning, defects, chondromalacia, and osteochondral lesions.
- Bones: Femur, tibia, fibula, and patella. MRI can identify bone bruises (contusions), stress fractures, osteonecrosis (avascular necrosis), tumors, and signs of osteoarthritis.
- Tendons: Such as the patellar tendon and quadriceps tendon, for tendinopathy or tears.
- Muscles: Surrounding the knee for strains or tears.
- Synovium and Joint Fluid: Detecting synovitis (inflammation of the joint lining) and joint effusions.
- Bursae: For bursitis (inflammation of the fluid-filled sacs around the joint).
- Nerves and Blood Vessels: In the vicinity of the knee joint.
Imaging Reconstruction and Surgical Planning
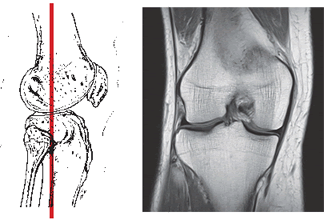
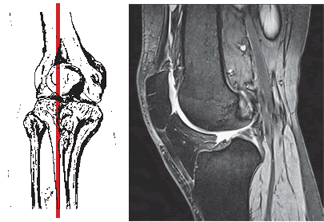
MRI of the knee joint allows for the acquisition of a series of thin slices in multiple planes (sagittal, coronal, axial). These images can then be processed to create three-dimensional (3D) reconstructions of the area under study. This capability also allows for highlighting the vasculature (though dedicated MR Angiography is more specific for vessels) and even tracing individual nerve trunks and vessels passing within the projection of the knee joint.
Such detailed reconstructions during MRI of the knee joint provide invaluable assistance to orthopedic surgeons and sports medicine physicians in precisely planning surgical interventions (e.g., arthroscopy, ligament reconstruction, meniscus repair) and for subsequent postoperative monitoring of the patient's condition and healing progress.
Video demonstrating the knee MRI procedure and what patients might experience.
Role in Early Diagnosis of Injuries
Early and accurate diagnosis with MRI of the knee is particularly crucial for common injuries such as knee ligament tears (e.g., ACL tear) or meniscus tears. These injuries often occur due to twisting mechanisms where the lower leg is tucked inward or outward, common in sports or accidents, especially in winter on slippery ice, ice-covered pitches, or steps. They can also occur from less forceful mechanisms like jumping from a low height or sudden deceleration. Prompt MRI diagnosis allows for the timely initiation of appropriate treatment, whether conservative or surgical, which can significantly improve outcomes and prevent long-term complications like chronic instability or osteoarthritis.
MRI of the knee joint allows for simultaneous demonstration of the joint itself (articular surfaces, menisci, ligaments) and the surrounding soft tissues (muscles, tendons, bursae) over a large area. This is typically achieved without the need for intra-articular contrast agent injection (though MR arthrography with contrast is used for specific indications like labral or subtle cartilage tears) and without using ionizing radiation, unlike X-rays or CT scans. MRI can effectively determine the localization and size of soft tissue tumors, assess the cartilaginous surfaces of the joints, and evaluate the integrity of muscles and tendons.
Currently, MRI has become a primary diagnostic tool for most diseases and injuries of the knee joint, often superseding or complementing other methods like X-rays (for bone alignment and fractures) and CT scans (for complex bony injuries).
Clinical Indications for Knee MRI
An MRI of the knee joint may be prescribed by a physician for various conditions and symptoms, including but not limited to:
- Traumatic Injuries to the Knee Joint:
- Suspected tears or sprains of ligaments (ACL, PCL, MCL, LCL).
- Suspected meniscus tears (medial or lateral).
- Articular cartilage injuries or osteochondral defects.
- Bone bruises or occult fractures not visible on X-rays.
- Tendon injuries (patellar tendon, quadriceps tendon).
- Muscle strains or tears around the knee.
- Dislocation or Instability of the Knee Joint: Including patellar dislocation or instability.
- Deforming Osteoarthritis (Arthrosis) of the Knee Joint (Gonarthrosis): To assess cartilage loss, bone spurs (osteophytes), subchondral bone changes, and meniscal degeneration.
- Inflammatory Conditions: Arthritis (e.g., rheumatoid arthritis, gout), synovitis, bursitis.
- Tumors in the Area of the Knee Joint: To detect, characterize, and stage bone or soft tissue tumors. Intravenous contrast may be used for better tumor delineation.
- Infections: Osteomyelitis (bone infection), septic arthritis (joint infection), or soft tissue abscesses.
- Osteonecrosis (Avascular Necrosis): Death of bone tissue due to lack of blood supply, often affecting the femoral condyles.
- Persistent Knee Pain, Swelling, or Mechanical Symptoms (locking, catching, giving way) of unclear etiology after initial clinical assessment and X-rays.
- Preoperative Planning and Postoperative Evaluation.
High-field MRI scanners (e.g., 3.0 T) are often preferred for knee imaging as they provide superior image quality and detail. Intravenous contrast (e.g., gadolinium-based agents like Omniscan) may be used to enhance the visual difference between healthy tissue and pathological processes like tumors or inflammation. Patient weight restrictions (e.g., up to 200 kg) are applicable.
MRI Techniques and Contrast Enhancement for Knee Imaging
Knee MRI protocols typically employ a combination of different pulse sequences to highlight various anatomical structures and pathologies:
- Proton Density (PD) Weighted Images: Excellent for visualizing menisci, ligaments, and cartilage detail. Often acquired with and without fat suppression.
- T1-Weighted Images (T1W): Provide good anatomical overview, useful for assessing bone marrow and fat.
- T2-Weighted Images (T2W) with Fat Suppression (e.g., STIR or fat-saturated T2): Highly sensitive for detecting fluid, edema, inflammation, and bone bruises, which appear bright.
- Gradient Echo (GRE) Sequences: Can be useful for cartilage assessment and detecting hemosiderin (blood products) or loose bodies.
- Sagittal, Coronal, and Axial Planes: Images are acquired in all three orthogonal planes for comprehensive evaluation.
- MR Arthrography: Involves injecting dilute gadolinium contrast directly into the knee joint before the MRI scan. This distends the joint capsule and allows contrast to seep into subtle tears of the menisci, ligaments, or cartilage, improving their detection. It is often used when high suspicion for an internal derangement exists but non-arthrographic MRI is equivocal.
- Intravenous Contrast (Gadolinium): Used if synovitis, infection, tumor, or inflammatory arthritis is suspected, to highlight areas of increased vascularity or inflammation.
Patient Preparation and Procedure
Preparation for a knee MRI is usually minimal:
- Screening: Patients complete a safety questionnaire regarding metallic implants, pacemakers, claustrophobia, pregnancy, and allergies (if contrast is planned).
- Metal Objects: All removable metallic items (jewelry, watches, etc.) must be removed.
- Clothing: Patients may be asked to change into a hospital gown.
- Fasting: Not typically required for a standard knee MRI without sedation. If IV contrast or MR arthrography is planned, specific instructions will be given.
During the procedure, the patient lies on the MRI table, and the knee is positioned within a specialized knee coil (a device that improves image quality). The table then slides into the MRI scanner. The patient must remain very still during the scan, which usually takes 30-60 minutes. Loud sounds are normal, and ear protection is provided.
Advantages and Limitations of Knee MRI
Advantages:
- Excellent visualization of soft tissues (menisci, ligaments, cartilage, tendons, muscles).
- No ionizing radiation.
- Multiplanar imaging capability.
- Highly sensitive for detecting a wide range of knee pathologies, including subtle injuries.
- Can guide treatment decisions and surgical planning.
Limitations:
- Higher cost compared to X-ray or ultrasound.
- Longer scan times, susceptible to motion artifacts.
- Less sensitive than X-ray or CT for evaluating acute bone fractures (though excellent for bone bruises and stress fractures).
- Contraindicated in patients with certain incompatible metallic implants.
- Can be challenging for claustrophobic patients.
- Findings may not always correlate with clinical symptoms (e.g., asymptomatic meniscus tears are common in certain age groups).
- Interpretation requires expertise in musculoskeletal radiology.
Comparison with Other Knee Imaging Modalities
| Modality | Principle | Radiation | Primary Strengths for Knee Imaging | Primary Weaknesses for Knee Imaging |
|---|---|---|---|---|
| Knee MRI | Magnetic fields, radio waves | No | Menisci, ligaments, cartilage, tendons, bone marrow edema, soft tissue masses. Comprehensive evaluation. | Cost, scan time, motion sensitivity, less detail for cortical bone fractures than X-ray/CT. |
| Knee X-ray (Radiography) | X-rays | Yes (low dose) | Bone fractures, dislocations, alignment, arthritis (joint space narrowing, osteophytes), loose bodies (if calcified). Inexpensive, fast, widely available. | Poor visualization of soft tissues (menisci, ligaments, cartilage). |
| Knee CT Scan | X-rays | Yes (higher dose) | Complex bone fractures, loose bodies, bony alignment, pre-operative planning for some bone procedures. Faster than MRI. | Radiation, poorer soft tissue contrast than MRI. Iodinated contrast risks if used. |
| Knee Ultrasound | Sound waves | No | Superficial soft tissues (tendons, ligaments like MCL/LCL, bursae, cysts like Baker's cyst), joint effusions, dynamic assessment. Guiding aspirations/injections. Inexpensive, portable. | Operator dependent, limited view of intra-articular structures (ACL, PCL, deep menisci, cartilage), cannot see through bone. |
| Arthroscopy (Surgical) | Direct visualization via camera | N/A (surgical procedure) | Gold standard for direct visualization and simultaneous treatment of many intra-articular pathologies. | Invasive, risks of surgery/anesthesia, diagnostic only if therapeutic intervention not planned. |
The Importance of MRI in Knee Pathology Management
MRI of the knee joint has revolutionized the diagnosis and management of knee disorders. Its ability to provide detailed anatomical information about both soft tissue and bony structures allows for accurate diagnosis, which is crucial for appropriate treatment selection (conservative vs. surgical), precise surgical planning when needed, and monitoring of healing and treatment outcomes. Early and accurate MRI diagnosis can lead to more effective interventions and better long-term prognoses for patients with knee injuries and diseases.
References
- Stoller DW. Magnetic Resonance Imaging in Orthopaedics and Sports Medicine. 3rd ed. Lippincott Williams & Wilkins; 2007.
- Resnick D, Kang HS, Pretterklieber ML. Internal Derangements of Joints. 2nd ed. Saunders Elsevier; 2007. Chapter on Knee.
- Crues JV 3rd, Ryu R. MRI of the knee. Part I. Radiographics. 1989 Mar;9(2):327-43.
- Rubin DA, Kneeland JB, Listerud J, et al. MR diagnosis of meniscal tears of the knee: value of fast spin-echo imaging. AJR Am J Roentgenol. 1994 May;162(5):1131-5.
- Kaplan PA, Helms CA, Dussault R, Anderson MW. Musculoskeletal MRI. 2nd ed. Saunders; 2001.
- American College of Radiology. ACR Appropriateness Criteria® Acute Knee Pain. Last review date: 2020.
- Mohana-Borges AV, Chung CB, Resnick D. MR imaging of the knee: an update. Radiol Clin North Am. 2004 Jul;42(4):631-47.
- Steinbach LS. MRI of the knee. Semin Roentgenol. 2004 Jul;39(3):273-98.
See also
- Magnetic Resonance Imaging (MRI)
- Magnetic Resonance Angiography (MRA) of the Cerebral Vessels
- Magnetic Resonance Imaging (MRI) of the Abdomen
- Magnetic Resonance Imaging (MRI) of the Brain
- Magnetic Resonance Imaging (MRI) of the Cervical Spine
- Magnetic Resonance Imaging (MRI) of the Hip Joint
- Magnetic Resonance Imaging (MRI) of the Knee Joint
- Magnetic Resonance Imaging (MRI) of the Lumbar Spine
- Magnetic Resonance Imaging (MRI) of the Pelvic Organs
- Magnetic Resonance Imaging (MRI) of the Pituitary Gland (Hypophysis)
- Magnetic Resonance Imaging (MRI) of the Shoulder Joint
- Magnetic Resonance Imaging (MRI) of the Thoracic Cavity Organs
- Magnetic Resonance Imaging (MRI) of the Thoracic Spine
- Magnetic Resonance Imaging (MRI) Study Principle
- Whole-Body Magnetic Resonance Imaging (MRI)