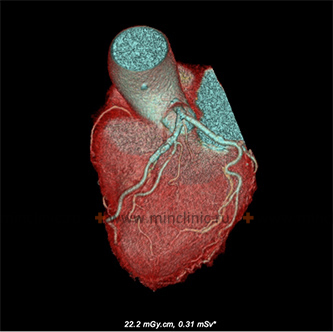
Coronary CT-angiography and computed tomography of the heart
Cardiac CT and Coronary CTA Overview
Coronary Computed Tomography Angiography (CCTA or Coronary CTA) is a specialized type of Cardiac CT scan that provides detailed, non-invasive visualization of the coronary arteries – the vessels supplying blood to the heart muscle (myocardium). It allows clinicians to reliably determine the presence, location, nature, and extent of narrowing (stenosis) or blockages within these arteries.
While Computed Tomography (CT) is a cornerstone of modern medical imaging, its application to the heart was historically limited by the heart's constant motion. Early CT scanners had scan times longer than a single heartbeat, resulting in blurry images. Electron-Beam Tomography (EBT), introduced in the 1980s, offered faster imaging suitable for cardiac applications, particularly calcium scoring, but remained relatively uncommon.
The advent of Multislice CT (MSCT) technology, starting around 1998, revolutionized cardiac imaging. MSCT scanners acquire data much faster, allowing for high-resolution images of the heart and coronary arteries synchronized with the patient's heartbeat (ECG-gating) to minimize motion artifacts. The use of MSCT for cardiac and vascular imaging has grown rapidly since then.
A major application of MSCT is the non-invasive assessment of coronary arteries. Traditionally, invasive X-ray coronary angiography (cardiac catheterization) has been the "gold standard" for diagnosing coronary artery disease (CAD). While highly accurate, invasive angiography carries small risks and cannot be performed on every patient needing evaluation. CCTA offers a valuable non-invasive alternative or complementary tool.
Modern Cardiac CT techniques, particularly Coronary CTA, allow detailed assessment of coronary artery anatomy, plaque characteristics (calcified and non-calcified), and the patency of coronary artery bypass grafts (CABG) and stents.
There are no absolute contraindications specific to Cardiac CT itself. Relative contraindications are similar to general CT and include:
- Severe patient instability or inability to cooperate (hold breath for 10-20 seconds, remain still).
- Pregnancy (radiation exposure risk).
- Patient weight exceeding the scanner table limit.
- For CCTA (which requires contrast): Significant allergy to iodinated contrast media or severe renal impairment.
- Certain arrhythmias (like atrial fibrillation) can sometimes degrade image quality but are often not absolute contraindications with modern scanners.
Applications of Cardiac CT & Coronary CTA
Multislice Cardiac CT (including CCTA and calcium scoring) has several key clinical applications:
- Detection and Quantification of Coronary Artery Calcification (CAC): Using a non-contrast scan to measure the amount of calcified plaque, providing prognostic information about future cardiovascular risk. (See Coronary Calcium Scoring below).
- Non-invasive Coronary Angiography (CCTA): Detailed visualization of the coronary arteries using intravenous contrast to detect stenosis (narrowing), non-calcified plaque, and anomalies. (See Coronary CT Angiography Details below and related invasive procedure Cardiac Catheterization).
- Assessment of Coronary Artery Bypass Grafts (CABG) and Stents: Evaluating the patency (openness) of bypass grafts and assessing for in-stent restenosis.
- Evaluation of Cardiac Anatomy and Function: Assessing heart chamber size, wall thickness, ejection fraction (heart pump function), and identifying congenital or acquired heart disease (e.g., cardiomyopathies, valve issues - though echocardiography and MRI are often primary for function/valves).
- Assessment of the Aorta and Pulmonary Arteries: Evaluation for aneurysms, dissection, pulmonary embolism, often performed as part of a chest CT protocol but can utilize cardiac gating.
- Planning Cardiac Procedures: Providing anatomical roadmaps before valve replacement (e.g., TAVR/TAVI), electrophysiology procedures (e.g., ablation), or complex congenital heart surgery.
Coronary Calcium Scoring
Coronary Artery Calcium (CAC) scoring, performed with non-contrast Cardiac CT, is used for cardiovascular risk stratification, particularly in asymptomatic individuals:
- Screening Asymptomatic Individuals: Primarily used for individuals at intermediate risk (based on traditional risk factors like age, cholesterol, blood pressure, smoking, diabetes) to refine risk assessment for future heart attacks or strokes. Recommended age ranges often target men 45-65 and women 55-75 without known heart disease.
- Clarifying Risk in Specific Cases: Can be useful when risk assessment is uncertain after initial evaluation or stress testing.
- Differential Diagnosis: May help differentiate causes of symptoms like chest pain (a score of zero makes significant obstructive CAD less likely) or heart failure (ischemic vs. non-ischemic origin).
A higher calcium score indicates a greater amount of atherosclerotic plaque and correlates with a higher risk of future cardiovascular events. However, calcium scoring does not show the degree of narrowing (stenosis); CCTA is required for that.
Coronary CTA (with contrast) is superior to calcium scoring for directly visualizing stenosis, assessing non-calcified ("soft") plaque, evaluating bypass graft/stent patency, and studying cardiac anatomy.
While CCTA is a powerful non-invasive tool, its diagnostic accuracy compared to invasive angiography can be influenced by factors like heart rate, rhythm, amount of calcification, and stent presence.
Coronary CT Angiography (CCTA) Details
Coronary CTA is particularly valuable for:
- Diagnosing Coronary Artery Disease (CAD): Detecting and quantifying the severity of stenosis in native coronary arteries, especially in patients with stable or acute chest pain and intermediate likelihood of CAD.
- Evaluating Coronary Anomalies: Identifying variations in the origin or course of coronary arteries.
- Assessing Coronary Aneurysms: Visualizing dilatations of the coronary arteries (e.g., in Kawasaki disease).
- Evaluating Stent Patency: Assessing for re-narrowing within previously placed coronary stents (in-stent restenosis). While challenging due to metal artifacts, newer scanners and reconstruction techniques have improved visualization.
- Assessing Bypass Graft Patency: Clearly visualizing coronary artery bypass grafts (both venous and arterial) to check if they are open and functioning.
CT angiography can also assess larger vessels, like the aorta after stent placement (example shown). Similar principles apply to visualizing coronary bypass grafts.
The rapid technological evolution of MSCT means that 3D imaging and advanced processing are now standard for Cardiac CT. Key factors determining image quality include scanner capabilities (number of detector rows, rotation speed, X-ray tube power) and sophisticated data acquisition and reconstruction algorithms synchronized with the patient's ECG.
The choice between Cardiac CT and Cardiac MRI depends on the specific clinical question. CT excels at visualizing coronary arteries and calcification, while MRI is often superior for assessing heart muscle viability, function, and characterizing tissue without ionizing radiation. The best approach depends on equipment availability, personnel expertise, and the specific diagnostic goals.
Preparation for the Scan
Preparation for a Cardiac CT or CCTA scan is important for obtaining high-quality images:
- Heart Rate Control: A slow and steady heart rate (ideally below 60-65 beats per minute) is crucial. You may be asked to avoid caffeine or stimulants for 12-24 hours beforehand. Medications like beta-blockers may be prescribed by your doctor or given by the medical team shortly before the scan to achieve the target heart rate.
- Nitroglycerin: Sublingual (under the tongue) nitroglycerin may be administered just before the scan to temporarily widen the coronary arteries for better visualization, unless there are medical reasons not to use it (e.g., very low blood pressure, use of certain other medications).
- Fasting: You may be asked not to eat for about 4 hours before the scan, especially since IV contrast is typically used for CCTA. Drinking water is usually allowed.
- Clothing and Metal Objects: Wear comfortable clothing without metal buttons or zippers on the upper body. You will need to remove necklaces or other metal items from the chest area.
- Medications: Inform the staff about all medications you take, including prescription, over-the-counter, and herbal supplements. Pay special attention to heart medications, metformin (for diabetes), and erectile dysfunction medications (which can interact with nitroglycerin). List any allergies, especially to iodine or previous contrast material reactions.
- Medical History: Notify the team about any history of kidney problems, diabetes, asthma, thyroid conditions, previous heart procedures, or if you might be pregnant.
The CT Procedure
During the Cardiac CT / CCTA scan:
- ECG Leads: Small sticky patches (ECG electrodes) will be placed on your chest. Wires connect these to the CT scanner to monitor your heart's electrical activity and synchronize the scan with your heartbeat, minimizing motion blur.
- Positioning: You will lie flat on your back on the CT scanner table, which will slide into the large, ring-shaped opening of the scanner. You will likely be asked to raise your arms above your head.
- IV Line: An intravenous (IV) catheter will be inserted into a vein, usually in your arm or hand. This is necessary for injecting the contrast material during CCTA (not used for calcium scoring).
- Breath-Holding Instructions: The technologist will guide you through breath-holding instructions via an intercom. You will need to hold your breath for short periods (usually 5-15 seconds) while the scanner acquires images. It is very important to hold completely still during these times.
- Contrast Injection (for CCTA): If performing CCTA, the iodinated contrast material will be rapidly injected through the IV line. As it circulates, you might feel a temporary warm sensation throughout your body, a metallic taste in your mouth, or an urge to urinate. These are common, expected side effects that pass quickly.
- Scanning: The scanner table moves through the ring while the X-ray tube and detectors rotate around you. The process is painless.
- Duration: While the actual image acquisition is very fast (often just a few seconds per breath-hold), the entire appointment time, including preparation, IV placement, potential medication administration, and instructions, might take 30 minutes to an hour or more.
Use of Contrast Material
Intravenous (IV) iodinated contrast material is essential for Coronary CT Angiography (CCTA) but is not used for Coronary Calcium Scoring.
- Purpose in CCTA: The contrast agent temporarily makes the blood flowing within the coronary arteries and heart chambers appear bright (radiopaque) on the CT images. This allows clear delineation of the vessel lumen (the inside channel) from the vessel wall and surrounding tissues.
- What it Shows: It enables the detection and assessment of:
- Luminal narrowing (stenosis) caused by plaque buildup.
- Characteristics of the plaque itself (calcified vs. non-calcified/soft).
- Coronary artery anomalies or aneurysms.
- Patency of bypass grafts and stents.
- Heart chamber anatomy and sometimes function.
- Administration: A power injector delivers the contrast rapidly through the IV line at a precise rate, timed carefully with the CT scan acquisition to capture the phase when the coronary arteries are best filled with contrast.
Risks and Benefits
Benefits:
- Non-Invasive: Provides detailed anatomical information without requiring arterial catheterization, unlike traditional angiography.
- High Negative Predictive Value: A normal CCTA scan is very effective at ruling out significant obstructive coronary artery disease, potentially avoiding the need for invasive testing.
- Comprehensive Assessment: Can visualize coronary arteries, heart chambers, pericardium, great vessels, and even parts of the lungs in a single scan.
- Plaque Characterization: Can identify both calcified and potentially higher-risk non-calcified plaque.
- Risk Stratification: Calcium scoring provides valuable prognostic information for asymptomatic individuals.
- Speed: The scan itself is very fast, making it suitable for emergency department evaluation of acute chest pain in selected patients.
Risks:
- Radiation Exposure: Cardiac CT uses ionizing radiation. Modern scanners employ dose-reduction techniques (like prospective ECG-gating), but cumulative exposure from multiple scans is a consideration. The diagnostic benefit must be weighed against this potential risk.
- Contrast Media Risks (for CCTA):
- Allergic-like Reactions: Mild reactions (itching, hives) occur occasionally; severe, life-threatening reactions (anaphylaxis) are rare. Prior reaction increases risk.
- Contrast-Induced Nephropathy (CIN): Potential worsening of kidney function, primarily a risk in patients with pre-existing significant renal impairment. Kidney function is often checked beforehand in at-risk individuals.
- Extravasation: Leakage of contrast from the vein into surrounding tissue at the IV site, causing local pain/swelling (uncommon with careful technique).
- Medication Side Effects: Potential side effects from beta-blockers (e.g., fatigue, low blood pressure/heart rate) or nitroglycerin (e.g., headache, dizziness).
- Arrhythmias: Rarely, the procedure or contrast might trigger heart rhythm disturbances.
- Limitations: Image quality can be reduced by very high or irregular heart rates, extensive calcification ("blooming artifact"), obesity, or motion/breathing artifacts. Accuracy for in-stent restenosis can be limited.
- Incidental Findings: May detect unexpected abnormalities in the lungs or other chest structures requiring further evaluation.
References
- Radiological Society of North America (RSNA) & American College of Radiology (ACR). (2023). Cardiac CT for Calcium Scoring. RadiologyInfo.org. Retrieved from https://www.radiologyinfo.org/en/info/ct_calcium
- Radiological Society of North America (RSNA) & American College of Radiology (ACR). (2023). Coronary CTA. RadiologyInfo.org. Retrieved from https://www.radiologyinfo.org/en/info/ct_coronary
- Mayo Clinic Staff. (2023). Coronary CT angiogram (CCTA). Mayo Clinic Patient Care & Health Information. Retrieved from https://www.mayoclinic.org/tests-procedures/coronary-ct-angiogram/about/pac-20468707
- Budoff, M. J., Nakazato, R., Mancini, G. B. J., Gransar, H., & Leipsic, J. A. (2018). SCCT guideline on the use of coronary artery calcium scoring. *Journal of Cardiovascular Computed Tomography*, 12(6), 469–478. https://doi.org/10.1016/j.jcct.2018.08.006
- Villines, T. C., Blankstein, R., Budoff, M. J., Hsia, J., Liu, K., Lloyd-Jones, D. M., Miedema, M. D., Pletcher, M. J., Shaw, L. J., & Polonsky, T. S. (2021). Coronary Artery Calcium Screening: A Scientific Statement From the American Heart Association. *Circulation*, 144(10), e168–e179. https://doi.org/10.1161/CIR.0000000000001009
- American College of Radiology. (2023). ACR Manual on Contrast Media. Retrieved from https://www.acr.org/Clinical-Resources/Contrast-Manual