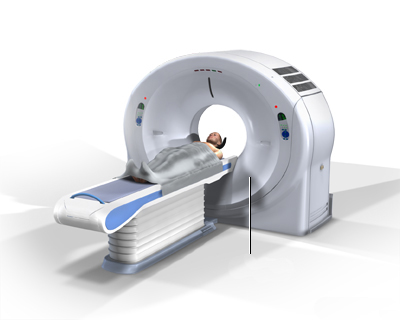
CT scan of the pelvic region (bones, organs)
What is a Pelvic CT Scan?
A Computed Tomography (CT) scan of the pelvis is a medical imaging technique that utilizes specialized X-ray equipment and computer processing to create detailed cross-sectional images (slices) of the pelvic region – the area located between the hip bones.
This examination allows doctors to visualize the bones, organs, blood vessels, and soft tissues within the pelvic cavity with high clarity. It is a valuable tool for diagnosing a wide range of conditions affecting this complex anatomical area.
What Structures are Seen?
A pelvic CT scan provides detailed views of structures including:
- Pelvic Bones: Hip bones (ilium, ischium, pubis), sacrum, and coccyx.
- Urinary System: Bladder, distal ureters.
- Reproductive Organs:
- Female: Uterus, cervix, ovaries, fallopian tubes.
- Male: Prostate gland, seminal vesicles.
- Lower Gastrointestinal Tract: Rectum, sigmoid colon, appendix (if located low), loops of small bowel.
- Muscles: Pelvic floor muscles, muscles around the hip joint.
- Blood Vessels: Iliac arteries and veins, other smaller pelvic vessels.
- Lymph Nodes: Pelvic and inguinal lymph nodes.
- Soft Tissues: Fat and connective tissues within the pelvis.
Pelvic CT scans are often performed in conjunction with an abdominal CT scan (CT Abdomen/Pelvis) to provide a more comprehensive evaluation of the entire abdominopelvic region.
Like all CT scans, pelvic CT uses ionizing radiation. While the risk from a single scan is low, the cumulative dose from multiple scans over time carries a small theoretical increase in cancer risk. This potential risk must always be weighed against the significant benefit of obtaining an accurate diagnosis.
The detailed images (slices) obtained can be viewed on a computer monitor, printed, or stored electronically. They can also be used to create three-dimensional (3D) reconstructions of the pelvic anatomy.
How the Pelvic CT Scan is Performed
The pelvic CT scan is typically performed in a hospital radiology department or an outpatient imaging center.
- You will be asked to lie flat on your back (supine position) on the CT scanner table. Your head might rest in a cradle for comfort.
- The table will then move slowly through the large, ring-shaped opening (gantry) of the CT scanner.
- As the table moves, the X-ray tube and detectors inside the gantry rotate around your pelvic region, acquiring the image data.
- The technologist operates the scanner from an adjacent control room but can see, hear, and speak with you via an intercom system throughout the procedure.
- It is crucial to remain very still during the scan, as movement can blur the images. You may be asked to hold your breath for brief periods (usually 5-15 seconds) during image acquisition.
- The entire procedure, including positioning and scanning, typically takes less than 30 minutes, with the actual scan time often being much shorter (under a minute with modern scanners).
Use of Contrast Media
Depending on the reason for the scan, contrast media may be used to enhance visualization:
- Intravenous (IV) Contrast: An iodine-based liquid injected into a vein (usually in the arm). It highlights blood vessels, vascular organs (like kidneys which extend near the pelvis), inflammation, and many types of tumors.
- Oral Contrast: A liquid swallowed by the patient starting 1-2 hours before the scan. It coats the inside of the bowel (small intestine, colon) helping to distinguish it from other structures and identify bowel abnormalities.
- Rectal Contrast: Sometimes administered via an enema immediately before the scan to better visualize the rectum and sigmoid colon.
If IV contrast is used, temporary sensations like warmth, a metallic taste, or feeling the need to urinate are common and quickly resolve. Oral contrast may have a chalky or slightly sweet taste.
Indications for Pelvic CT Scan
Pelvic CT scans are valuable diagnostic tools for a wide range of conditions. Common indications include:
- Evaluation of Pelvic Pain: Investigating causes of acute or chronic pelvic pain, such as appendicitis (if low-lying), diverticulitis, pelvic inflammatory disease (PID), ovarian cysts, or other sources.
- Trauma Assessment: Detecting pelvic bone fractures, sacroiliac joint injuries, bladder or bowel injuries, and internal bleeding (hemorrhage) after accidents or injuries.
- Cancer Detection and Staging: Identifying, characterizing, and determining the extent (staging) of cancers originating in or spreading to the pelvis, including cancers of the bladder, prostate, uterus, cervix, ovaries, rectum, and bone. Also used to monitor treatment response.
- Infection and Inflammation: Diagnosing abscesses (collections of pus), diverticulitis, appendicitis, inflammatory bowel disease affecting the distal bowel, and other inflammatory conditions.
- Vascular Issues: Evaluating pelvic blood vessels for aneurysms, clots, or other abnormalities (often using CT Angiography technique).
- Guidance for Procedures: Assisting physicians in accurately guiding needles for biopsies or draining fluid collections (e.g., abscess drainage).
- Surgical Planning: Providing detailed anatomical information before surgery (e.g., complex pelvic fracture repair, tumor removal, organ transplants).
- Radiation Therapy Planning: Helping radiation oncologists precisely target tumors while minimizing radiation exposure to surrounding healthy organs.
Interpreting Pelvic CT Scan Results
A qualified radiologist interprets the images obtained from the pelvic CT scan. The report will describe the appearance of the visualized pelvic bones, organs, blood vessels, lymph nodes, and soft tissues.
The interpretation focuses on identifying any deviations from normal anatomy or findings suggestive of pathology. Key findings that can be ascertained include:
- Normal Findings: Organs and structures appear normal in size, shape, density, and position, with no evidence of masses, inflammation, fluid collections, or injury.
- Abnormal Findings Indicating Pathology:
- Masses/Tumors: Presence of abnormal growths in organs (bladder, prostate, uterus, ovaries, rectum), bones, or soft tissues, suggestive of benign or malignant (cancerous) conditions. Contrast enhancement patterns can help characterize tumors.
- Inflammation/Infection: Signs like bowel wall thickening (e.g., diverticulitis, appendicitis), fat stranding (haziness in the fat), abscess formation (distinct fluid collections, often with enhancing walls), or organ enlargement.
- Trauma: Detection of pelvic bone fractures, joint dislocations, hematomas (collections of blood), or injury to organs like the bladder or bowel.
- Fluid Collections: Abnormal accumulations of fluid, such as abscesses, hematomas, lymphoceles, or ascites.
- Stones: Calcifications within the bladder or distal ureters (kidney stones).
- Vascular Abnormalities: Aneurysms, blood clots (thrombosis), or signs of vascular injury.
- Bone Abnormalities: Fractures, arthritis, bone lesions (tumors, infections).
- Lymph Node Enlargement: Suggestive of infection, inflammation, or cancer spread.
The radiologist's report provides a detailed description of the findings and a diagnostic impression, which your referring doctor will use in conjunction with your clinical history and other test results to determine the diagnosis and appropriate management.
How to Prepare for the Pelvic CT Scan
Preparation instructions vary depending on whether contrast media will be used:
- Contrast Instructions:
- IV Contrast: If intravenous contrast is planned, you will likely be asked not to eat or drink anything (except possibly clear liquids or water) for 4 to 6 hours before the scan.
- Oral Contrast: If oral contrast is needed to visualize the bowel, you will be given specific instructions on when and how much to drink, typically starting 1-2 hours before the scan time.
- Rectal Contrast: If needed, this is usually administered by the technologist just before the scan.
- Medications: Inform your doctor about all medications you are taking. If you take metformin (Glucophage) for diabetes and are receiving IV contrast, specific instructions are needed as it may need to be temporarily stopped.
- Allergies: Crucially, inform your doctor and the CT staff if you have ANY allergies, especially a known allergy to iodine or a previous reaction to CT contrast dye. Premedication might be necessary.
- Kidney Function: Inform your doctor if you have any history of kidney problems, as IV contrast may not be suitable or may require extra precautions (like hydration). Blood tests to check kidney function might be done beforehand.
- Clothing and Jewelry: Wear comfortable clothing and remove all metal jewelry, belts, or clothing with metal fasteners from the pelvic area before the scan. You will likely change into a hospital gown.
- Pregnancy: Inform your doctor immediately if there is any possibility you could be pregnant.
- Weight Limit: While less common with modern scanners, verify if the specific CT machine has a weight limit if you have significant obesity.
Risks and Benefits
Benefits:
- Provides detailed cross-sectional images of pelvic bones, organs, and soft tissues.
- Fast, widely available, and generally non-invasive (except for IV contrast injection).
- Excellent for evaluating acute conditions like trauma, appendicitis, diverticulitis, and obstruction.
- Crucial for cancer staging, surgical planning, and radiation therapy planning.
- Can detect a wide range of abnormalities including fractures, infections, tumors, and bleeding.
Risks:
- Radiation Exposure: Uses ionizing radiation, carrying a small cumulative risk over many scans. The diagnostic benefit generally outweighs this risk for indicated studies.
- Contrast Media Reactions (Iodine-Based IV Contrast):
- Allergic-like Reactions: Most reactions are mild (e.g., itching, hives, nausea, sneezing). Severe, life-threatening anaphylactic reactions are rare but possible. Inform staff immediately if you experience difficulty breathing, swelling, or severe symptoms during or after contrast injection. Prior significant reaction is a major risk factor; premedication may be used if contrast is essential.
- Contrast-Induced Nephropathy (CIN): Potential temporary or, rarely, permanent worsening of kidney function, primarily in patients with pre-existing significant kidney disease or dehydration. Adequate hydration and kidney function screening are important precautions.
- Pregnancy: CT scans are generally avoided due to radiation risk to the fetus unless absolutely necessary.
- Incidental Findings: May reveal unrelated findings that require further investigation.
References
- Radiological Society of North America (RSNA) & American College of Radiology (ACR). (2023). Body CT (Abdomen and Pelvis). RadiologyInfo.org. Retrieved from https://www.radiologyinfo.org/en/info/bodyct
- Mayo Clinic Staff. (2022). CT scan. Mayo Clinic Patient Care & Health Information. Retrieved from https://www.mayoclinic.org/tests-procedures/ct-scan/about/pac-20393675
- American College of Obstetricians and Gynecologists (ACOG). (2017). Committee Opinion No. 723: Guidelines for Diagnostic Imaging During Pregnancy and Lactation. *Obstetrics & Gynecology*, 130(4), e210-e216.
- American College of Radiology. (2023). ACR Manual on Contrast Media. Retrieved from https://www.acr.org/Clinical-Resources/Contrast-Manual
- Webb, W. R., Brant, W. E., & Major, N. M. (Eds.). (2019). *Fundamentals of Body CT* (5th ed.). Elsevier. [Note: Example textbook reference]