Thorax (chest) CT scan
What is a Chest CT Scan?
A Computed Tomography (CT) scan of the chest (also called thorax CT) is a non-invasive diagnostic imaging test that uses specialized X-ray equipment and advanced computer processing to create detailed cross-sectional images (slices) of the structures within the chest cavity.
This technique provides highly detailed views of the lungs, airways (trachea and bronchi), heart, large blood vessels (aorta, pulmonary arteries/veins), esophagus, mediastinum (the space between the lungs containing the heart, major vessels, esophagus, trachea, and lymph nodes), and the bones of the chest wall (ribs, sternum, thoracic spine).
Chest CT is considered one of the best imaging methods for evaluating the soft tissues of the lungs, heart, and mediastinum, offering significantly more detail than a standard chest X-ray.
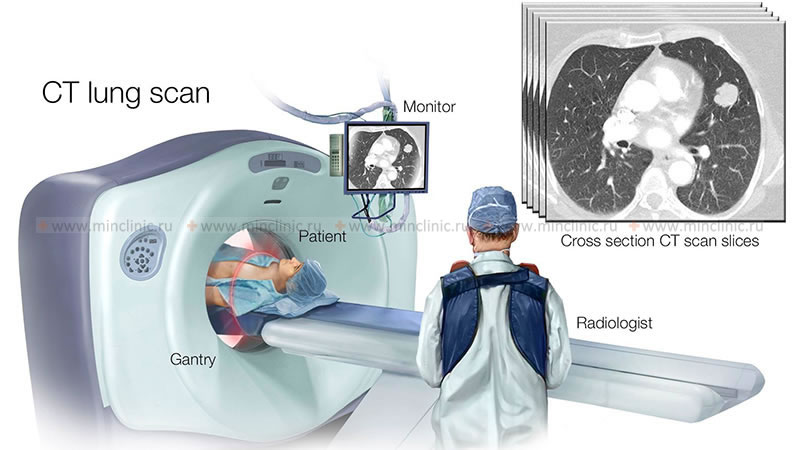
How Chest CT Works
The patient lies on a motorized table that moves into the center of the CT scanner's gantry (the large doughnut-shaped part). Inside the gantry, an X-ray tube rotates around the patient's chest, emitting X-ray beams.
Detectors positioned opposite the X-ray tube measure the amount of radiation that passes through the different tissues of the chest. The computer processes this vast amount of data, collected from multiple angles, to mathematically reconstruct detailed cross-sectional images (slices).
Modern multislice CT (MSCT) scanners acquire data in a continuous spiral (helical) fashion as the table moves, allowing for very rapid scanning of the entire chest, often in a single breath-hold. This speed is crucial for minimizing artifacts caused by breathing or heart motion.
The resulting image slices can be viewed on a monitor, printed, or stored electronically. The volumetric data acquired also allows for the creation of images in different planes (coronal, sagittal) and three-dimensional (3D) reconstructions of chest structures.
Use of Contrast Media
For many chest CT applications, particularly evaluating blood vessels (like for pulmonary embolism or aortic dissection), detecting tumors, or assessing inflammation/infection, an intravenous (IV) contrast agent (dye) is administered. This iodine-based liquid is injected into a vein, usually in the arm, shortly before or during the scan. The contrast highlights blood vessels and enhances the visibility of certain tissues and abnormalities.
Oral or rectal contrast is generally NOT used for standard chest CT scans.
Structures Visualized
A chest CT provides detailed views of:
- Lungs: Lung parenchyma (tissue), airways (trachea, bronchi), pulmonary arteries and veins.
- Pleura: The lining surrounding the lungs.
- Mediastinum: Heart, aorta, superior and inferior vena cava, pulmonary arteries/veins, trachea, esophagus, thymus gland, lymph nodes.
- Chest Wall: Ribs, sternum, thoracic spine, muscles, soft tissues.
- Upper Abdomen: Often includes the upper parts of the liver, spleen, adrenal glands, and kidneys, depending on the scan range.
Indications for Chest CT Scan
Chest CT scans are performed for a wide variety of reasons to diagnose, stage, or monitor conditions affecting the thorax:
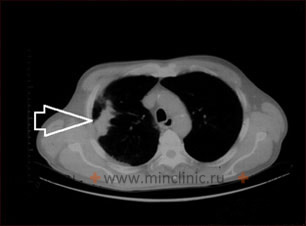
- Lung Nodule Evaluation: Detecting, characterizing, and following up on spots found on chest X-rays or previous CTs.
- Lung Cancer Screening: Low-dose CT scans are used to screen high-risk individuals (heavy smokers) for early-stage lung cancer.
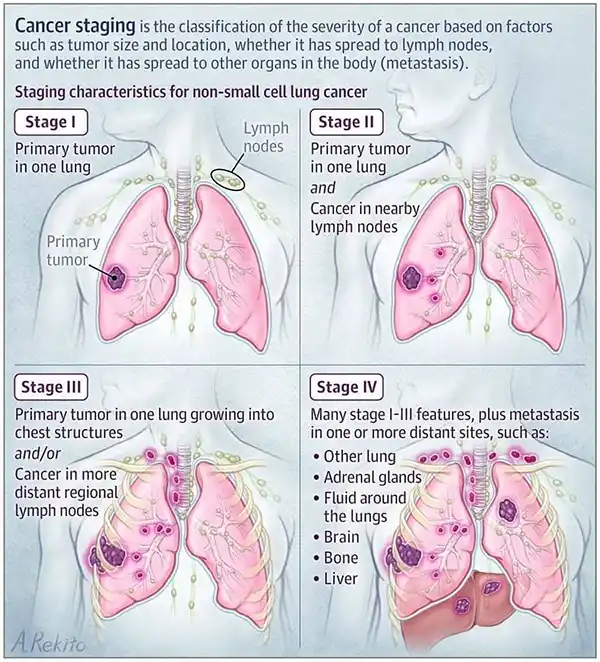
- Cancer Staging and Monitoring: Determining the extent of lung cancer or other cancers that may have spread to the chest (metastases), and monitoring response to treatment.
- Pneumonia and Infections: Diagnosing complex or suspected severe pneumonia, lung abscesses, empyema (pus in the pleural space), or opportunistic infections (e.g., in immunocompromised patients).
- Pulmonary Embolism (PE): CT Pulmonary Angiography (CTPA), a specialized chest CT with timed IV contrast, is the primary method for diagnosing blood clots in the pulmonary arteries.
- Aortic Disease: Detecting aortic aneurysms (widening) or aortic dissection (tear in the aortic wall) using CT Angiography (CTA) of the chest.
- Interstitial Lung Disease (ILD): Evaluating patterns of lung scarring and inflammation characteristic of various ILDs (e.g., idiopathic pulmonary fibrosis, sarcoidosis, asbestosis). High-Resolution CT (HRCT) protocols are often used.
- Airway Diseases: Assessing conditions like bronchiectasis (widening of airways), emphysema, or tracheal/bronchial stenosis.
- Mediastinal Abnormalities: Evaluating masses (e.g., thymoma, lymphoma), enlarged lymph nodes (lymphadenopathy), or vascular abnormalities within the mediastinum.
- Pleural Disease: Detecting pleural effusions (fluid around the lung), pleural thickening, or pleural tumors (e.g., mesothelioma).
- Chest Trauma: Evaluating injuries to the lungs (contusion, laceration), airways, heart, great vessels, esophagus, diaphragm, ribs, sternum, or spine after significant trauma. Detecting pneumothorax (collapsed lung) or hemothorax (blood in the chest cavity).
- Congenital Abnormalities: Assessing structural abnormalities of the heart, lungs, or great vessels present from birth.
- Guidance for Procedures: Used to guide needle biopsies of lung nodules or mediastinal masses, or placement of drainage tubes.
- Cardiac Evaluation: While specialized Cardiac CT exists, standard chest CT can provide information about heart size, pericardial effusion (fluid around the heart), and coronary artery calcification. (See specific cardiac conditions listed in original text like cardiomyopathy, tamponade, valve issues - though CT isn't primary for all).
Common Findings on Chest CT
Chest CT scans can reveal a wide array of normal and abnormal findings, including:
- Lung nodules or masses (potentially benign or malignant)
- Consolidation (indicating pneumonia or other airspace filling process)
- Ground-glass opacities (suggesting inflammation or fluid)
- Interstitial thickening (seen in ILD)
- Emphysema (destruction of air sacs)
- Bronchiectasis (permanent widening of airways)
- Atelectasis (collapsed lung tissue)
- Pneumothorax (air outside the lung in the pleural space)
- Pleural effusion (fluid in the pleural space)
- Pleural thickening or plaques (common with asbestos exposure)
- Enlarged lymph nodes (lymphadenopathy) in the mediastinum or hila
- Mediastinal masses (e.g., thymoma, lymphoma, teratoma)
- Aortic aneurysm or dissection
- Pulmonary embolism (clots in pulmonary arteries)
- Pericardial effusion (fluid around the heart)
- Coronary artery calcification
- Hiatal hernia
- Rib fractures or other bone lesions
Preparation for Chest CT Scan
Preparation varies depending on whether IV contrast will be used:
- Without Contrast (e.g., Lung Cancer Screening, HRCT): Usually no specific preparation is needed. You can typically eat, drink, and take medications as usual. Remove metal necklaces or clothing items with metal over the chest.
- With IV Contrast (e.g., PE study, cancer staging, aortic imaging):
- You may be asked to fast (no food or drink, except possibly water) for 4-6 hours before the scan.
- Inform your doctor and the CT staff about ALL allergies, especially previous reactions to iodine or contrast media. Premedication may be required for known allergies if contrast is necessary.
- Inform staff about kidney problems, diabetes (especially if taking metformin), thyroid disease, asthma, or multiple myeloma. Kidney function tests (creatinine level) may be checked beforehand.
- Remove metal objects from the chest area. You will likely wear a hospital gown.
- Pregnancy: Always inform your doctor and the technologist if there is any possibility you are pregnant.
- Weight Limits: Check with the facility regarding weight limits if applicable.
The Chest CT Procedure Experience
The actual scanning process is quick and painless:
- You'll lie on the CT table, typically on your back, often with arms raised above your head to keep them out of the chest images.
- The table moves you into the scanner opening.
- The technologist communicates via intercom, providing instructions, especially for breath-holding. Holding your breath steadily when asked is crucial for clear lung images.
- If IV contrast is given, you'll feel a needle prick for the IV insertion. During injection, the common sensations of warmth, metallic taste, or feeling like you need to urinate may occur briefly.
- You might hear whirring or clicking sounds from the scanner.
- Some people find the table slightly hard, but discomfort is usually minimal. The procedure itself takes only a few minutes, with the actual scan often completed in seconds.
Risks and Benefits
Benefits:
- Provides highly detailed images of the lungs, airways, blood vessels, heart, mediastinum, pleura, and chest wall.
- Fast, widely available, and essential for diagnosing many acute and chronic chest conditions.
- Critical tool for lung cancer detection, staging, and screening in high-risk populations.
- Gold standard for diagnosing pulmonary embolism (CTPA).
- Excellent for evaluating chest trauma.
- Can guide biopsies and drainages.
Risks:
- Ionizing Radiation: Chest CT involves radiation exposure. Doses are optimized (ALARA principle), especially for screening (low-dose CT). The small theoretical long-term risk is weighed against the immediate diagnostic benefit. Cumulative dose from repeat scans is a consideration.
- Contrast Media Risks (if IV contrast used):
- Allergic-like Reactions: Mild reactions occur occasionally; severe reactions are rare. Inform staff immediately of any adverse symptoms (e.g., trouble breathing). Prior history increases risk.
- Contrast-Induced Nephropathy (CIN): Risk of kidney function decline, primarily in patients with pre-existing severe kidney disease.
- Pregnancy: Generally avoided due to fetal radiation risk, unless the benefit clearly outweighs the risk. Alternative imaging (like MRI or ultrasound for some indications) might be considered.
- Incidental Findings: May reveal unexpected findings requiring further evaluation.
- Breast Tissue Radiation: Particularly relevant for younger women undergoing repeated chest CTs; dose reduction techniques are important.
Discuss any concerns about risks versus benefits with your doctor.
References
- Radiological Society of North America (RSNA) & American College of Radiology (ACR). (2022). Chest CT (Computed Tomography). RadiologyInfo.org. Retrieved from https://www.radiologyinfo.org/en/info/chestct
- Mayo Clinic Staff. (2022). CT scan. Mayo Clinic Patient Care & Health Information. Retrieved from https://www.mayoclinic.org/tests-procedures/ct-scan/about/pac-20393675
- National Lung Screening Trial Research Team. (2011). Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. *New England Journal of Medicine*, 365(5), 395–409. https://doi.org/10.1056/NEJMoa1102873
- American College of Radiology. (n.d.). ACR Appropriateness Criteria®. Retrieved from https://acsearch.acr.org/list (Search for specific chest conditions like "Acute Chest Pain - Suspected Pulmonary Embolism" or "Rib Fractures")
- Parker, M. S., Rosado-de-Christenson, M. L., & Abbott, G. F. (Eds.). (2018). *Chest Imaging Case Atlas* (2nd ed.). Thieme. [Note: Example case-based textbook]
- American College of Radiology. (2023). ACR Manual on Contrast Media. Retrieved from https://www.acr.org/Clinical-Resources/Contrast-Manual