Magnetic Resonance Imaging (MRI) of the Chest Organs
- Understanding MRI of the Chest Organs
- The MRI Procedure for Chest Organs
- Patient Preparation for Chest MRI
- Patient Experience and Tolerability of Chest MRI
- Clinical Indications for Chest MRI
- Common Pathologies Detected by Chest MRI
- Potential Risks, Complications, and Limitations of Chest MRI
- Interpreting Chest MRI Results
- Comparison with Other Chest Imaging Modalities
- References
Understanding Magnetic Resonance Imaging (MRI) of the Chest Organs
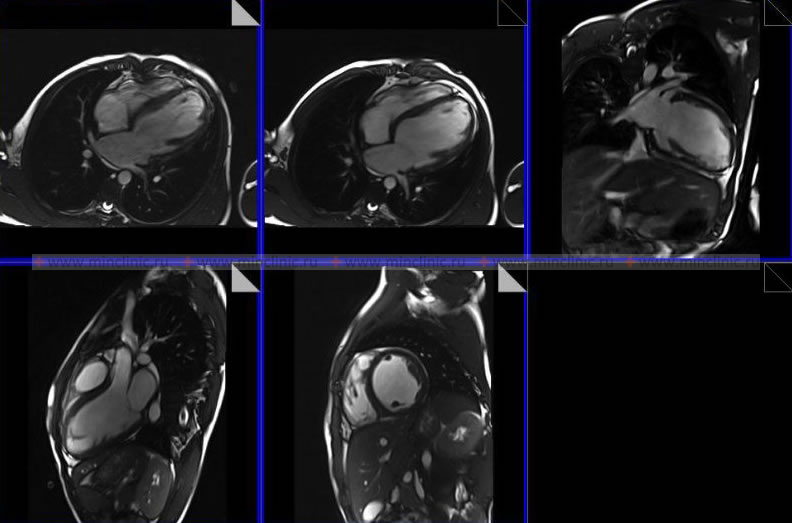
Magnetic Resonance Imaging (MRI) of the chest organs (often referred to as thoracic MRI when focused on non-spinal structures) is an advanced diagnostic imaging technique. It utilizes a powerful magnet, radiofrequency waves, and sophisticated computer algorithms to generate detailed cross-sectional images of the organs and tissues within the chest cavity. This includes structures such as the heart, major blood vessels (aorta, pulmonary arteries and veins), lungs (though with some limitations for lung parenchyma), mediastinum (the space between the lungs containing the heart, esophagus, trachea, and lymph nodes), pleura, and chest wall.
Basic Principles and Safety
The fundamental principle of MRI involves aligning hydrogen protons within the body's tissues using a strong magnetic field. Radiofrequency pulses are then applied, temporarily disturbing this alignment. As the protons relax back, they emit radio signals that are detected by the MRI scanner and processed by a computer to create images. A key advantage of MRI is its safety profile: during an MRI of the chest organs, the patient does not receive any ionizing radiation exposure, unlike CT scans or X-rays.
The MRI Procedure for Chest Organs
Patient Positioning and Scan Process
When undergoing an MRI of the chest organs, the patient is typically positioned lying supine (on their back) on a motorized table that slides into the center of the large, cylindrical MRI scanner. Specialized coils (antennae that transmit and receive radiofrequency signals) may be placed around the chest to optimize image quality for this specific region.
Video illustrating the general MRI procedure, applicable to chest organ imaging.
The radiologist and MRI technologist operate the scanner from an adjacent control room, maintaining visual contact through a window and verbal communication via an intercom system. The duration of a chest MRI examination typically ranges from 30 to 60 minutes, but can be longer depending on the specific protocols used, the number of sequences required, and whether contrast material is administered.
Role of Contrast Agents
Some types of MRI of the chest organs necessitate the use of a special intravenous contrast agent, usually gadolinium-based. This contrast material is administered to the patient through a vein, typically in the elbow or hand. The contrast, by accumulating in tissues with altered vascularity or inflammation, enhances the resulting image, making pathological areas more conspicuous. This provides the radiologist with a more detailed picture of the state of the organ or tissue being examined, aiding in the differentiation of various disease processes. Intravenous Gadolinium Contrast is a non-ionic paramagnetic agent whose properties cause signal enhancement on MRI. This increased signal from affected tissues provides greater informational content compared to non-contrast MRI data for certain pathologies.
Patient Preparation for a Chest Magnetic Resonance Imaging Procedure
General Guidelines and Claustrophobia Management
Before the scheduled examination, patients are often asked not to eat or drink fluids for 4-6 hours before the start of the chest MRI procedure, particularly if contrast or sedation is planned. However, specific instructions may vary.
It is crucial to clarify in advance if the patient referred for an MRI examination experiences claustrophobia (fear of enclosed spaces). In such instances, the patient might need to take a prescribed sedative beforehand to induce slight drowsiness and alleviate anxiety. Some facilities offer "open" type MRI machines ("open MRI" or "open-bore MRI"), which have more free space on the sides and can be less intimidating for claustrophobic patients. Modern scanners with wider bores (e.g., 70 cm aperture) also tend to reduce the number of patients requiring preliminary sedation during chest examinations.
Screening for Contraindications (Metal Implants)
Before an MRI procedure of the chest organs (or any MRI), it is imperative to exclude the presence of certain metallic implants or foreign bodies in the patient. MRI is generally not possible or not safe if the patient has:
- Certain types of clips for cerebral aneurysms (older ferromagnetic ones).
- Some intravascular stents (many modern ones are MRI-conditional).
- Certain artificial metal heart valves.
- Cardiac defibrillators and most pacemakers (unless specifically designated as MRI-conditional and scanned under strict safety protocols).
- Neurostimulators for the brain or spinal cord.
- Cochlear implants in the inner ear.
- Metal fragments in the body from accidents, explosions, or injuries (e.g., shrapnel, particularly near vital organs or eyes).
- Some artificial joints (though most modern ones are MRI-compatible).
The presence of ferromagnetic metal can cause severe image artifacts (blurring) and, more critically, poses a risk of displacement (migration) or heating of the implants within the body due to the powerful magnetic field. Medical device manufacturers have increasingly started producing implantable components using special non-ferromagnetic alloys (e.g., titanium) that are not significantly affected by the MRI machine's magnetic field. The manufacturer explicitly indicates the MRI compatibility (e.g., "MRI Safe," "MRI Conditional," "MRI Unsafe") of their device in the accompanying documentation, which must be verified.
Patients must also inform staff about any history of kidney disease or if they are on dialysis, as this is important if intravenous contrast is considered (due to the risk of NSF with certain agents in severe renal impairment).
All external metallic items must be removed from the patient and from anyone entering the MRI scan room. These include:
- Fountain pens, pocket knives, metal-rimmed glasses.
- Metal jewelry (rings, watches, necklaces, earrings), bank credit cards and passes (magnetic strips can be erased), hearing aids.
- Metal hairpins, safety pins, clasps, and zippers on clothing.
- Removable dentures with metal components (should be removed before the tomography).
Technology and Scanner Considerations
High-field MRI scanners, for example, those with a magnetic field strength of 3.0 T (Tesla), are often preferred for their ability to produce higher resolution images. Intravenous contrast agents (e.g., Omniscan, though specific agents vary) can be used to increase the visual difference between healthy tissue and pathological tissue like tumors or areas of inflammation. Patient weight restrictions (e.g., up to 200 kg) are a practical consideration for the MRI scanner table.
Patient Experience and Tolerability of the Procedure of Magnetic Resonance Imaging of the Chest Organs by Patients
The MRI procedure itself is painless and does not cause any direct physical discomfort. However, patients need to lie still for an extended period within the confines of the MRI scanner, which can be challenging for some.
If a patient (especially children or anxious individuals) cannot lie still or is nervous during the examination, a short-acting sedative drug may be administered to help them calm down and relax during the procedure. Any movement of the patient's body during the MRI scan of the chest organs will cause motion artifacts, which can degrade the quality of the images received by the apparatus and potentially lead to errors in diagnosis.
The surface of the MRI scanner table might feel cool or hard for some patients. They can usually be covered with a blanket for warmth, and a pillow may be placed under their head or knees for support, provided this does not interfere with the main examination area or the placement of imaging coils.
An intercom system integrated into the MRI machine allows the patient to communicate with the medical staff located in the adjacent control room throughout the diagnostic procedure. Some MRI scanners are also equipped with built-in video monitors or headphones, enabling the patient to watch a movie or listen to music. This can serve as a distraction and make the experience more tolerable while they are inside the scanner during the image acquisition process.
After the completion of the chest MRI procedure, the patient can typically resume their normal life and activities immediately. There are generally no restrictions on diet or physical activity, except in cases where sedation was administered. If sedated, the patient will need assistance to get home and should avoid activities requiring full alertness until the sedative effects have fully worn off.
Indications for Magnetic Resonance Imaging of the Chest
MRI of the chest allows specialists to obtain detailed images of the organs located within the thoracic cavity (such as the heart, bronchi, lungs, major blood vessels, esophagus, thymus, and lymph nodes) to assess their functional state or identify organic (structural) changes.
MRI of the chest organs is performed in patients in various clinical situations, including:
- Cardiovascular Evaluation:
- Assessment of cardiac anatomy, function, viability, and perfusion (Cardiac MRI).
- Diagnosis of congenital heart disease.
- Evaluation of cardiomyopathies, pericardial diseases (pericarditis, effusion).
- Detection of cardiac tumors (e.g., atrial myxoma).
- Assessment of aortic diseases (e.g., aneurysm, dissection, coarctation) using MR Angiography (MRA).
- Evaluation of pulmonary vasculature (e.g., for pulmonary embolism with MRA, though CTPA is often preferred acutely).
- Mediastinal Evaluation:
- Detection, characterization, and staging of mediastinal masses (e.g., thymoma or tumor of the thymus gland, lymphoma, germ cell tumors, neurogenic tumors).
- Assessment of lymph node involvement (metastases, lymphoma, sarcoidosis).
- Evaluation of esophageal tumors or abnormalities.
- Pulmonary and Pleural Evaluation (Specific Indications):
- Characterization of certain lung tumors or nodules, especially if contrast with CT is contraindicated or if soft tissue invasion is questioned.
- Assessment of pleural diseases (e.g., thickening with pleurisy, effusion, mesothelioma).
- While CT is generally superior for lung parenchyma, MRI can be useful for chest wall invasion by lung cancer or for specific conditions like cystic lung damage if CT is inconclusive or contraindicated.
- General Oncological Staging: Detecting the stage of cancer, including the spread of a tumor from chest organs to other parts of the body (metastases), or metastatic spread to the chest from other primary sites. Determining the stage of cancer development allows for the selection of an adequate method of treatment and helps in making a prognosis for the patient.
- Alternative to CT Angiography: To avoid radiation exposure or iodinated contrast, MRA can be used to assess thoracic vasculature.
- Clarification of Findings from Other Imaging: To further evaluate abnormalities detected on previous radiography (X-ray) or computed tomography (CT).
- Assessment of Congenital Anomalies: Developmental anomalies of the heart, great vessels, or other thoracic structures.
Common Pathologies Detected by Chest MRI
An MRI of the chest can reveal a wide range of abnormalities affecting the heart, lungs, mediastinum, and chest wall. Some examples include:
- Developmental anomalies and acquired pathologies of the great vessels of the chest (e.g., aortic aneurysm, dissection, coarctation, pulmonary artery anomalies).
- Pathologies of the lymph nodes within the chest (e.g., lymphoma, metastatic disease, sarcoidosis).
- Stenosis (narrowing) or obstruction (blockage of the lumen) of major vessels like the aorta or superior vena cava.
- Cardiac tumors (e.g., atrial myxoma) or pericardial diseases (pericarditis, pericardial effusion, constrictive pericarditis - "armored heart").
- Valvular heart disease (e.g., mitral regurgitation, mitral valve prolapse - though echocardiography is primary).
- Cardiomyopathies (e.g., ischemic, restrictive, hypertrophic).
- Developmental anomalies and acquired pathologies of the bronchi.
- Cardiac tamponade (blood or pericardial effusion compressing the heart).
- Chronic Obstructive Pulmonary Disease (COPD) - MRI is not primary for COPD diagnosis but can show complications or associated findings.
- Cystic lung damage or diseases (though CT is often preferred for lung parenchyma).
- tumors of the esophagus.
- Pulmonary edema (fluid in the lungs - usually diagnosed clinically and by X-ray/CT, but MRI can show it).
- Lung tumors (lung cancer) - MRI can be used for staging, especially assessing chest wall, mediastinal, or vascular invasion.
- Pathological masses and tumors within the chest cavity.
- Pathological changes in the pleura, such as thickening due to pleurisy or effusion in the pleural cavity.
- Thymoma or other tumors of the thymus gland.
- tumors of the sternum or chest wall.
Potential Risks, Complications, and Limitations of Chest Magnetic Resonance Imaging
Safety Profile
The MRI machine does not use X-rays (ionizing radiation) in its operation, unlike CT tomographs or conventional radiography. To date, there have been no established widespread reports in medical literature of direct, harmful side effects on the body from exposure to the magnetic fields and radio waves used in standard diagnostic MRI procedures when appropriate safety protocols are meticulously followed.
Risks with Contrast Media
Most types of MRI contrast media contain gadolinium. Intravenous gadolinium-based contrast agents (GBCAs) are generally considered safe for chest MRI when used appropriately. Allergic reactions to GBCAs administered through a vein are extremely rare. However, gadolinium can be harmful to patients with significantly impaired kidney function (severe chronic kidney disease or those on dialysis) due to the risk of Nephrogenic Systemic Fibrosis (NSF), a rare but serious sclerosing condition. Therefore, if a patient has known renal insufficiency, caution must be exercised when prescribing MRI studies of the chest organs (or any region) that require contrast enhancement, and renal function should be assessed beforehand.
Magnetic Field Concerns
The strong magnetic field generated by the MRI machine can damage or cause malfunction of certain implanted electronic devices (e.g., pacemakers, ICDs, cochlear implants, neurostimulators) unless they are specifically MRI-conditional. Ferromagnetic metal fragments or plates in the body can also be affected, potentially moving, shifting, or heating up, leading to injury or image artifact.
Limitations for Lung Parenchyma and Practical Considerations
At the current stage in the development of medical technology, MRI is not typically the most valuable primary tool for detecting or monitoring subtle or diffuse changes in lung tissue (parenchyma). The lungs contain a large amount of air and are subject to respiratory and cardiac motion, which makes high-quality MRI visualization of fine lung detail inherently difficult. CT scans are generally superior for evaluating lung nodules, interstitial lung disease, emphysema, and acute pulmonary conditions.
Examining the chest organs on an MRI machine may not always be the optimal first choice for several reasons:
- High Research Cost: MRI is generally more expensive than chest X-ray or CT.
- Long Duration of the Scanning Process: Chest MRI can take a significant amount of time, requiring patient cooperation to remain still.
- High Sensitivity to Motion: Movement of internal organs (breathing, heartbeat) and the whole body during tomography can degrade image quality more than in CT. Specialized techniques like respiratory gating or breath-holding are used to mitigate this but add to scan time and complexity.
- Limited Lung Parenchymal Detail: As mentioned, air in the lungs provides low signal on MRI, making it less ideal for detailed lung tissue assessment compared to CT.
However, MRI excels in specific chest applications such as cardiac imaging, mediastinal mass characterization, chest wall assessment, and vascular imaging with MRA.
Interpreting Chest MRI Results
If an MRI of the chest organs is normal, no pathological changes will be revealed. The data obtained from the MRI results, especially if visible changes are present, are further analyzed by the patient's attending physician. This analysis, in conjunction with clinical findings and other diagnostic tests, helps the physician to develop a plan for any necessary additional examinations and to formulate an appropriate treatment strategy.
Comparison with Other Chest Imaging Modalities
| Modality | Principle | Radiation | Primary Strengths for Chest Imaging | Primary Weaknesses for Chest Imaging |
|---|---|---|---|---|
| Chest MRI | Magnetic fields, radio waves | No | Cardiac anatomy/function, mediastinal masses, chest wall lesions, vascular structures (MRA), assessing tumor invasion. Excellent soft tissue contrast. | Poor for lung parenchyma detail/nodules, motion artifacts, long scan time, cost, MRI contraindications. |
| Chest CT Scan | X-rays | Yes | Excellent for lung parenchyma (nodules, interstitial disease, emphysema), pulmonary embolism (CTA), acute aortic syndromes, trauma, bone detail. Fast. | Radiation exposure, poorer soft tissue contrast than MRI for some applications. Iodinated contrast risks. |
| Chest X-ray (Radiography) | X-rays | Yes (low dose) | Initial assessment of lungs (pneumonia, effusion, pneumothorax, gross masses), heart size/shape, bone fractures. Inexpensive, fast, widely available. | Limited detail, superimposition of structures, poor for subtle lesions or soft tissues. |
| Echocardiography (Ultrasound of Heart) | Sound waves | No | Real-time cardiac structure and function, valvular disease, pericardial effusion. Portable, inexpensive. | Operator dependent, limited by patient habitus/lung interference, less anatomical detail than cardiac MRI for some aspects. |
| PET-CT | Radiotracer (PET) + X-rays (CT) | Yes | Detecting metabolically active tumors (cancer staging, recurrence, treatment response), characterizing indeterminate pulmonary nodules. | Radiation, cost, availability, lower anatomical resolution than dedicated CT/MRI for some structures. |
References
- Webb WR, Higgins CB. Thoracic Imaging: Pulmonary and Cardiovascular Radiology. 2nd ed. Lippincott Williams & Wilkins; 2010.
- Westbrook C, Roth C, Talbot J. MRI in Practice. 5th ed. Wiley-Blackwell; 2018. Chapter on Thoracic and Cardiac Imaging.
- Kuhlman JE, Fishman EK, Wang KP, Siegelman SS. Mediastinal masses: CT and MR imaging. Radiographics. 1989 Sep;9(5):869-91.
- Pennell DJ, Sechtem UP, Higgins CB, et al. Clinical indications for cardiovascular magnetic resonance (CMR): Consensus Panel report. Eur Heart J. 2004 Dec;25(23):2087-103. (Older but foundational for CMR)
- American College of Radiology. ACR Appropriateness Criteria® Noninvasive Clinical Staging of Primary Lung Cancer. Last review date: 2022.
- Kauczor HU, Ley-Zaporozhan J, Ley S. Imaging of the Elderly Chest. Radiol Clin North Am. 2017 Jul;55(4):799-813. (General context for chest imaging).
- Hatabu H, Ohno Y, Gefter WB, et al. ACR-STR Practice Parameter for the Performance of Thoracic Magnetic Resonance Imaging (MRI). Revised 2016.
- Batra K, Sunkaraneni V, Bhargava P, et al. MRI of the lungs and pleura. AJR Am J Roentgenol. 2015 Sep;205(3):W259-71.
See also
- Magnetic Resonance Imaging (MRI)
- Magnetic Resonance Angiography (MRA) of the Cerebral Vessels
- Magnetic Resonance Imaging (MRI) of the Abdomen
- Magnetic Resonance Imaging (MRI) of the Brain
- Magnetic Resonance Imaging (MRI) of the Cervical Spine
- Magnetic Resonance Imaging (MRI) of the Hip Joint
- Magnetic Resonance Imaging (MRI) of the Knee Joint
- Magnetic Resonance Imaging (MRI) of the Lumbar Spine
- Magnetic Resonance Imaging (MRI) of the Pelvic Organs
- Magnetic Resonance Imaging (MRI) of the Pituitary Gland (Hypophysis)
- Magnetic Resonance Imaging (MRI) of the Shoulder Joint
- Magnetic Resonance Imaging (MRI) of the Thoracic Cavity Organs
- Magnetic Resonance Imaging (MRI) of the Thoracic Spine
- Magnetic Resonance Imaging (MRI) Study Principle
- Whole-Body Magnetic Resonance Imaging (MRI)