Magnetic Resonance Angiography (MRA) of Cerebral Vessels
- Understanding Magnetic Resonance Angiography (MRA) of Cerebral Vessels
- Clinical Indications for Cerebral MRA
- MRA Techniques and Contrast Enhancement
- Benefits and Limitations of Cerebral MRA
- Patient Preparation and Procedure
- Comparison with Other Cerebrovascular Imaging Modalities
- Role in Diagnosis and Treatment Planning
- References
Understanding Magnetic Resonance Angiography (MRA) of Cerebral Vessels
Magnetic Resonance Angiography (MRA) of the cerebral vessels is a specialized type of Magnetic Resonance Imaging (MRI) designed to visualize the arteries and veins of the brain and neck. It stands as one of the most promising and rapidly advancing methods in modern diagnostics of the vascular bed, offering detailed insights without requiring direct arterial puncture, as is necessary with conventional catheter angiography.
Principles and Advantages
MRA utilizes the principles of MRI—powerful magnetic fields, radiofrequency pulses, and computer processing—to generate images of blood flow. Different MRA techniques exploit the inherent motion of blood or use contrast agents to highlight vascular structures. A significant advantage of MRA is its non-invasive nature (or minimally invasive if contrast is used) and its ability to provide detailed anatomical and functional information about the cerebral vasculature without exposing the patient to ionizing radiation (X-rays).
With MRA of the brain vessels, physicians can investigate structural abnormalities and pathological changes within the vascular system of the brain tissue. Furthermore, MRA can be combined with standard MRI sequences to concurrently evaluate physicochemical and pathophysiological processes occurring in the entire brain parenchyma and its coverings (meninges), or within specific brain structures.
Video illustrating the general procedure and patient experience during a Magnetic Resonance Angiography (MRA) of the brain vessels.
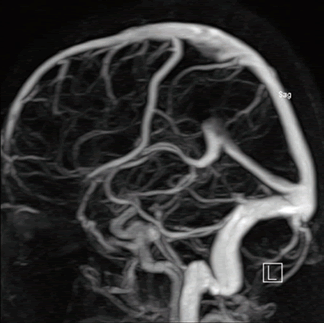
Imaging Capabilities and Reconstruction
MRA of cerebral vessels allows for the acquisition of a series of thin cross-sectional images. These images can then be processed using specialized software to create three-dimensional (3D) reconstructions of the vasculature within the area under study. This powerful tool enables clinicians to visualize the complex network of arteries and veins from various angles, isolate individual nerve trunks and vessels as they pass through specific parts of the brain, and assess their relationship to surrounding brain tissue.
Such detailed 3D reconstructions derived from cerebral MRA provide invaluable assistance to physicians in:
- Accurate diagnosis of vascular pathologies.
- Comprehensive treatment planning (e.g., for surgical intervention, endovascular procedures, or radiation therapy).
- Subsequent monitoring of treatment effectiveness and disease progression during patient therapy.
Early and precise diagnosis using MRA of the brain vessels allows for timely initiation of appropriate treatment, which can significantly improve patient outcomes. The ability of MRA to simultaneously demonstrate the vessel itself and the surrounding soft tissues over a large area—often without introducing contrast agents directly into the vessel lumen and without using ionizing radiation—is a major advantage. It is highly effective for determining the localization and size of critical pathologies such as aneurysms, hematomas, blood clots (thrombi or emboli), and abnormal vascular connections like arteriovenous malformations (AVMs) or fistulas.
Currently, Magnetic Resonance Angiography (MRA) of cerebral vessels has emerged as a leading diagnostic modality for many vascular diseases of the brain, often relegating older methods such as conventional X-ray angiography (which requires arterial puncture) and, in some specific vascular indications, standard computed tomography (CT) scans, to secondary or complementary roles.
Clinical Indications for Cerebral MRA
An MRA of the cerebral vessels may be prescribed by a doctor in various clinical situations to diagnose or evaluate conditions affecting the brain's blood supply. Common indications include:
- Suspicion or known Arteriovenous Malformations (AVMs) of the brain or other vascular anomalies.
- Evaluation of cerebral and spinal adhesive arachnoiditis if vascular involvement or complications are suspected.
- Assessment of encephalopathy where a vascular cause (e.g., chronic ischemia, vasculitis) is considered.
- Investigation of persistent or atypical headache or migraine, especially if concerning features suggest underlying vascular pathology.
- Evaluation of conditions associated with increased intracranial pressure and hydrocephalus to assess venous outflow or related vascular issues.
- Diagnosis and monitoring of ischemic brain disease (cerebrovascular disease), including assessment of arterial stenosis or occlusion.
- Acute evaluation in ischemic stroke or transient ischemic attack (TIA) to identify occluded vessels (e.g., carotid artery, middle cerebral artery) and assess cerebral ischemia.
- Investigation of unexplained nosebleeds (epistaxis) if a vascular anomaly within the head (e.g., carotid-cavernous fistula, aneurysm) is suspected as a rare cause.
- As part of the workup for certain neurological conditions like Parkinson's disease if vascular parkinsonism is in the differential, or to rule out vascular lesions mimicking symptoms.
- Assessment of vascular supply or compression in cases of pituitary microadenoma, macroadenoma, nonfunctioning pituitary adenomas (NFPAs), or hyperprolactinemia syndrome.
- Screening for, diagnosis of, and follow-up of saccular aneurysms (berry aneurysms) and assessment after subarachnoid hemorrhage.
- Evaluation of symptoms suggestive of somatoform autonomic dysfunction if vascular dysregulation is considered, though MRA is not primary for this.
- Following traumatic brain injury (TBI) (concussion, contusion, brain hemorrhage, axonal shearing lesions) to assess for vascular injury such as dissection, pseudoaneurysm, or traumatic occlusion.
- Diagnosis of vertebrobasilar insufficiency (VBI) presenting with vertigo, to evaluate the posterior circulation arteries (vertebral and basilar arteries).
- Detection of dural venous sinus thrombosis.
- Evaluation of vasculitis affecting cerebral vessels.
MRA Techniques and Contrast Enhancement
Several MRA techniques can be employed to visualize cerebral vessels, some of which do not require intravenous contrast agents, while others utilize them for enhanced detail.
Time-of-Flight (TOF) MRA
TOF MRA is a common non-contrast technique that relies on the principle of flow-related enhancement. It distinguishes flowing blood from stationary tissue by exploiting the unsaturated spins of protons in fresh blood entering the imaging slice, which appear bright compared to the saturated spins of static tissue. 2D TOF is often used for larger areas like the carotid arteries, while 3D TOF provides higher resolution for intracranial vessels.
Phase-Contrast (PC) MRA
PC MRA is another non-contrast technique that uses differences in the phase of proton spins induced by blood flow along magnetic field gradients. It can provide quantitative information about blood flow velocity and direction, in addition to anatomical images. It is particularly useful for imaging venous structures or assessing flow dynamics.
Contrast-Enhanced (CE) MRA
In CE-MRA, a gadolinium-based contrast agent (e.g., Omniscan, though specific agents used vary) is injected intravenously. The contrast agent shortens the T1 relaxation time of blood, making vessels appear bright on T1-weighted images. This technique provides excellent vessel delineation, is less susceptible to flow artifacts than TOF MRA, and allows for imaging over larger areas with faster acquisition times. It is often used for evaluating extracranial carotid and vertebral arteries, venous sinuses, or when non-contrast techniques are suboptimal.
High-field MRI scanners, such as those with a magnetic field strength of 3.0 T (Tesla), offer improved signal-to-noise ratio and spatial resolution for all MRA techniques, potentially enhancing the visualization of smaller vessels and subtle pathologies. It's also possible to combine MRA with standard MRI sequences using intravenous contrast to increase the visual difference between healthy brain tissue and tumors or areas of inflammation.
Patient weight limitations (e.g., up to 200 kg) are a practical consideration for any MRI procedure, including MRA.
Benefits and Limitations of Cerebral MRA
Benefits:
- Non-invasive or Minimally Invasive: Many MRA techniques (TOF, PC) do not require contrast injection or arterial puncture. CE-MRA involves only an IV injection.
- No Ionizing Radiation: Unlike CT Angiography (CTA) or Digital Subtraction Angiography (DSA).
- Excellent Soft Tissue Detail: Can be combined with standard MRI to evaluate brain parenchyma simultaneously.
- Good Visualization of Arteries and Veins: Including their course and relationship to other structures.
- 3D Reconstruction Capabilities: Allows for comprehensive assessment from multiple angles.
- Flow Information (with PC-MRA): Can quantify blood flow.
Limitations:
- Susceptibility to Motion Artifacts: Patient movement can degrade image quality.
- Overestimation of Stenosis: Non-contrast TOF MRA can sometimes overestimate the degree of arterial narrowing due to turbulent or slow flow artifacts.
- Limited Resolution for Very Small Vessels: Compared to DSA, which remains the gold standard for fine vascular detail.
- Contraindications to MRI: Certain metallic implants (e.g., older pacemakers, some aneurysm clips), claustrophobia.
- Contrast Agent Risks (for CE-MRA): Though rare, allergic reactions or NSF (in patients with severe renal impairment) are potential risks with gadolinium.
- Longer Scan Times: Compared to CTA.
- Cost: Generally more expensive than CTA or ultrasound.
Patient Preparation and Procedure
Preparation for an MRA of cerebral vessels is similar to a standard brain MRI:
- Screening: Patients are screened for any contraindications to MRI (e.g., metallic implants, claustrophobia, pregnancy).
- Metal Objects: All metallic items must be removed.
- Fasting: Usually not required for non-contrast MRA. If contrast is planned, fasting for a few hours might be requested, especially if sedation is a possibility.
- Contrast Information: If CE-MRA is performed, an IV line will be placed. Patients should inform staff of any allergies or kidney problems.
During the procedure, the patient lies on a table that slides into the MRI scanner. They will hear loud noises and must remain still. The scan typically takes 30-60 minutes.
Comparison with Other Cerebrovascular Imaging Modalities
| Modality | Principle | Invasiveness | Radiation | Contrast | Strengths | Weaknesses |
|---|---|---|---|---|---|---|
| MRA (Cerebral) | Magnetic fields, radio waves, blood flow | Non-invasive (TOF, PC) or Minimally invasive (CE-MRA via IV) | No | Often none (TOF, PC); Gadolinium (CE-MRA) | Good vessel detail, no radiation, soft tissue imaging, 3D. | Motion artifacts, overestimation of stenosis (TOF), longer scan, cost, MRI contraindications. |
| CT Angiography (CTA - Cerebral) | X-rays with IV iodinated contrast | Minimally invasive (IV contrast) | Yes | Iodinated (IV) | Fast, excellent for acute stroke/hemorrhage, good for stenosis/aneurysms, widely available. | Radiation, contrast risks (allergy, nephropathy), less soft tissue detail than MRI. |
| Digital Subtraction Angiography (DSA - Catheter Angiography) | X-rays with intra-arterial iodinated contrast | Invasive (arterial puncture/catheterization) | Yes | Iodinated (intra-arterial) | Gold standard for vascular detail, allows for intervention (e.g., coiling, stenting). | Invasive risks (bleeding, stroke, vessel injury), radiation, contrast risks. |
| Carotid/Transcranial Doppler Ultrasound | Sound waves, Doppler effect | Non-invasive | No | None | Real-time flow assessment, portable, inexpensive. Good for carotid stenosis screening. | Operator dependent, limited intracranial window (especially TCD), bone artifact. |
Role in Diagnosis and Treatment Planning
Cerebral MRA plays a vital role in the non-invasive evaluation of a wide spectrum of cerebrovascular diseases. Its ability to depict arteries and veins, identify abnormalities like aneurysms, AVMs, stenosis, or occlusion, and be combined with conventional MRI for brain tissue assessment makes it an indispensable tool in neurology, neurosurgery, and neuroradiology for diagnosis, guiding therapeutic decisions, and monitoring treatment outcomes.
References
- Edelman RR, Hesselink JR, Zlatkin MB, Crues JV. Clinical Magnetic Resonance Imaging. 3rd ed. Saunders Elsevier; 2006. Chapter on MR Angiography.
- Westbrook C, Roth C, Talbot J. MRI in Practice. 5th ed. Wiley-Blackwell; 2018. Chapter on Angiography.
- Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF. Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics. 2006 Oct;26 Suppl 1:S19-41; discussion S42-3.
- Wardlaw JM, Chappell FM, Stevenson M, et al. Accurate, practical and cost-effective assessment of carotid stenosis in the UK. Health Technol Assess. 2006 Sep;10(30):iii-iv, ix-x, 1-182. (Compares MRA with other modalities for carotid stenosis)
- Wintermark M, Sesay M, Barbier E, et al. Comparative overview of brain perfusion imaging techniques. J Neuroradiol. 2005 Dec;32(5):294-314. (Context for vascular imaging)
- Parker DL, Roberts JA, Watanabe Y, et al. Advances in MRA: flow and motion. J Magn Reson Imaging. 1999 Sep;10(3):339-53.
- Provenzale JM, актуальный Sorensen AG. MR angiography: principles and clinical applications. AJR Am J Roentgenol. 1995 Sep;165(3):499-509.
- American College of Radiology. ACR–ASNR–SPR Practice Parameter for the Performance of Magnetic Resonance Angiography (MRA). Revised 2022.
See also
- Magnetic Resonance Imaging (MRI)
- Magnetic Resonance Angiography (MRA) of the Cerebral Vessels
- Magnetic Resonance Imaging (MRI) of the Abdomen
- Magnetic Resonance Imaging (MRI) of the Brain
- Magnetic Resonance Imaging (MRI) of the Cervical Spine
- Magnetic Resonance Imaging (MRI) of the Hip Joint
- Magnetic Resonance Imaging (MRI) of the Knee Joint
- Magnetic Resonance Imaging (MRI) of the Lumbar Spine
- Magnetic Resonance Imaging (MRI) of the Pelvic Organs
- Magnetic Resonance Imaging (MRI) of the Pituitary Gland (Hypophysis)
- Magnetic Resonance Imaging (MRI) of the Shoulder Joint
- Magnetic Resonance Imaging (MRI) of the Thoracic Cavity Organs
- Magnetic Resonance Imaging (MRI) of the Thoracic Spine
- Magnetic Resonance Imaging (MRI) Study Principle
- Whole-Body Magnetic Resonance Imaging (MRI)