Whole-Body Magnetic Resonance Imaging (MRI)
- Introduction to Whole-Body Magnetic Resonance Imaging (WB-MRI)
- Historical Context and Recent Trends in Radiology
- The Diagnostic Procedure for Whole-Body MRI
- Clinical Indications and Results of Whole-Body MRI
- Patient Preparation, Procedure, and Safety
- Advantages and Limitations of WB-MRI
- Comparison with Other Whole-Body Imaging Modalities
- Conclusion: The Expanding Role of WB-MRI
- References
Introduction to Whole-Body Magnetic Resonance Imaging (WB-MRI)
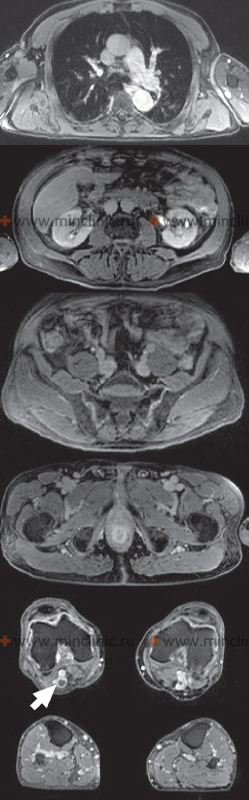
Whole-Body Magnetic Resonance Imaging (WB-MRI) represents a significant advancement in diagnostic radiology, offering a non-invasive method to image large portions or the entirety of the human body in a single examination session. This article discusses recent progress in WB-MRI technology and highlights key clinical indications for its use.
Evolution and Technological Prerequisites
The feasibility of WB-MRI is a direct result of substantial hardware and software improvements in MRI technology. These include stronger and more homogeneous magnets, faster gradient systems, advanced coil designs (surface coils that can cover large anatomical areas or move with the patient table), and sophisticated image acquisition and reconstruction algorithms. These developments have enabled the acquisition of high-quality images over extensive body regions within clinically acceptable timeframes.
Key Applications: Vascular Imaging and Oncology
Two major areas where WB-MRI has shown considerable promise are vascular imaging and oncology:
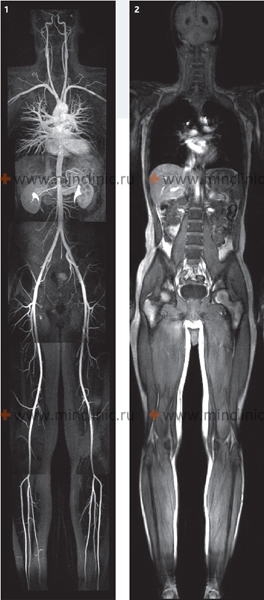
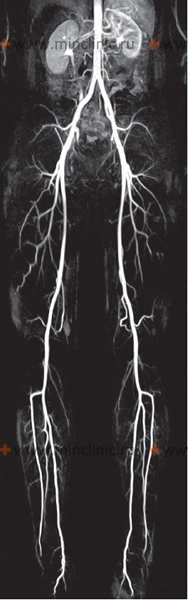
- Whole-Body Magnetic Resonance Angiography (WB-MRA): This technique facilitates the visualization of nearly the entire arterial system, from the intracranial vessels down to the arteries of the lower extremities, in a single study. It typically excludes detailed imaging of the coronary arteries of the heart, which require specialized cardiac MRI techniques. WB-MRA is invaluable for assessing systemic atherosclerotic disease, vasculitis, or other widespread vascular pathologies.
- Oncological Applications: WB-MRI can serve as an alternative to skeletal scintigraphy (bone scan) for the detection of bone metastases. It exploits the high fluid sensitivity of certain MRI sequences (like STIR or DWI) to detect marrow infiltration by tumor cells. Furthermore, the administration of intravenous contrast media can enhance the detection of both primary tumors and metastatic disease in various organs and soft tissues throughout the body.
Video providing an overview of the Whole-Body MRI scanning process.
Challenges and Future Directions
One of the inherent challenges that imaging physicians must be prepared for when interpreting WB-MRI studies is the significant increase in the volume of data generated per examination. This large dataset requires meticulous review and can potentially increase the likelihood of incidental findings and, if not carefully managed, the number of false negatives (missed pathologies) or false positives in the studied patient population.
The ongoing development of WB-MRI is focused on several key areas: improving image contrast and spatial resolution, enhancing coil technology for faster data acquisition, reducing scan times, and ultimately, making the examination more cost-effective and accessible for patients. Advanced techniques like diffusion-weighted whole-body imaging with background body signal suppression (DWIBS) are also expanding its utility, particularly in oncology.
Historical Context and Recent Trends in Radiology
Whole-Body Magnetic Resonance Imaging (WB-MRI) has evolved as a significant alternative diagnostic method in relation to other imaging techniques for assessing widespread or systemic pathological organic changes. It's important to recall that the term "whole-body magnetic resonance imaging" was initially introduced around 1980. At that time, it often referred to the study of body regions *other than* the brain, spinal cord, and associated spinal structures—primarily encompassing organs of the chest, abdomen, and extremities.
Only a few years ago, technological limitations meant that only one limited part of a patient's body could be examined within a reasonable timeframe using MRI. Today, however, advancements in WB-MRI technology allow for comprehensive imaging of the entire body, effectively "from head to toe," in a single, albeit often lengthy, procedure.
The first truly whole-body applications of MRI often involved angiography. **Whole-Body Magnetic Resonance Angiography (WB-MRA)** provided images of the arterial bed from the head down to the feet, typically acquired in one study session after a single bolus injection of an intravenous contrast agent. Shortly thereafter, the application of WB-MRI expanded to the detection of tumors and, notably, bone metastases, offering a radiation-free alternative to scintigraphy. Currently, the study and assessment of the muscular and skeletal systems, parenchymal organs (liver, spleen, kidneys, pancreas), blood vessels (arteries and veins), the heart, and even segments of the intestines have become feasible within a single comprehensive WB-MRI examination, though specific protocols are tailored to the clinical question.
The Diagnostic Procedure for Whole-Body MRI
Overcoming Limitations of Older MRI Systems
Different types of MRI scanners (tomographs) can visualize tissues of various organs with differing degrees of detail and efficiency. Unlike Computed Tomography (CT), which can rapidly scan large body sections, older MRI systems could typically examine only one specific area of the body in a single procedure, limited by the scanner's field of view (often around 40-50 cm). For an extended study of the patient, each part of their body (within sequential 40-50 cm segments) had to be examined separately, often requiring repositioning of the patient or the imaging coils. This limitation, along with a finite number of sensors (receiver channels) on the scanner table, sometimes necessitated scanning the patient either head-first or feet-first into the scanner bore, depending on the region of interest. It was also necessary to physically move and reposition surface coils to optimize signal from different body regions during the extended study.
If intravenous contrast was administered, the study might have been practically limited to one or two body regions to capture the optimal contrast enhancement phase. This is because the peak enhancement from gadolinium-based contrast agents typically occurs within the first few minutes after intravenous injection (timing depends on the type of pathological process and the tissue under study) and generally lasts for a useful diagnostic window of up to about 45 minutes. These limitations of older MRI machines led to prolonged examination times for patients undergoing multiple regional studies and could be a stressful experience.
Modern WB-MRI Technology
Recent technological advancements have largely overcome many of these limitations when performing WB-MRI scans. Modern WB-MRI systems often feature:
- Moving Table Technology: The patient table automatically moves through the scanner bore, allowing continuous data acquisition over long anatomical regions without needing to reposition the patient.
- Integrated Whole-Body Coils: Patients may be covered with extensive, integrated surface coil arrays from head to toe, eliminating the need to shift coils during the scan.
- High Field Strength Magnets: Scanners with magnetic field strengths of 1.5 Tesla (T) or, increasingly, 3.0 T are used, providing better signal-to-noise ratio and image resolution.
- Parallel Imaging Techniques: Allow for faster image acquisition.
- Advanced Sequences: Specialized sequences for WB-MRI (e.g., STIR for bone marrow, DWIBS for tumor detection, contrast-enhanced MRA for vasculature) are optimized for large field-of-view imaging.
These features allow for examination of patients with a large body habitus (e.g., weight limits up to 200 kg on some modern scanners) and facilitate more efficient and comprehensive whole-body evaluations.
Clinical Indications and Results of Whole-Body MRI
Atherosclerosis and Systemic Vascular Disease
WB-MRI research, particularly **Whole-Body Magnetic Resonance Angiography (WB-MRA)**, provides a unique opportunity to identify and assess possible disorders arising from atherosclerosis affecting the human arterial system comprehensively. For evaluating major arteries like the carotid arteries, renal arteries, or peripheral limb arteries, WB-MRA has become comparable in informational value to invasive imaging methods such as selective catheter-based angiography. A key advantage is that performing WB-MRA does not necessarily require an increase in examination time or the amount of injected contrast agent (contrast) compared to some extensive regional MRA protocols, especially with modern rapid acquisition techniques. This can significantly reduce the invasiveness and cost of comprehensive vascular diagnostics. Over time, further improvements in the detail and resolution of WB-MRA images are expected as the technical aspects of the MRI apparatus itself continue to advance.
Comprehensive Arterial System Examination (Whole-Body MRA)
Based on modern WB-MRA methods, it has become possible to visualize the vasculature of the brain, heart (though coronary arteries are still challenging and often require dedicated Cardiac MRA or CTCA), and peripheral arteries from the carotid arteries down to the lower leg arteries in a single examination. Modern WB-MRA techniques aim to optimize the dose of intravenous contrast agent administered to the patient during diagnosis, often utilizing timed bolus tracking or specialized contrast agents. As a result, it is often possible to obtain high-quality images of extensive arterial territories within a 45-60 minute examination, regardless of the specific organs being examined within that sweep. WB-MRA can identify not only macroscopic changes in the arterial bed (e.g., stenosis, occlusion, aneurysms, dissections, excluding detailed coronary vessel assessment) but also assess for potential end-organ damage resulting from conditions like infectious myocarditis (if cardiac sequences are included), stroke (with concurrent brain MRI/MRA), or microangiopathy affecting cerebral vessels.
Whole-Body MR Venography (MRV)
Historically, venous imaging (phlebography or venography) was primarily performed using X-ray techniques with iodinated contrast media. After the introduction of paramagnetic contrast agents for MRI into clinical practice in 1988, contrast-enhanced MR Venography (MRV) became available. Now, many specialized hospital departments (e.g., cardiology, intensive care, vascular surgery) utilize MRV for their patients. For instance, MRI angiography of the pulmonary artery (MRPA) to assess for pulmonary embolism can be supplemented with MRV of the lower extremities, abdominal cavity, and small pelvis to diagnose deep vein thrombosis (DVT) and search for a potential source of pulmonary emboli, all within a reasonably comprehensive examination. The high accuracy of MRV, comparable to classical X-ray phlebography, makes it a much safer diagnostic option for evaluating veins in pregnant women because it avoids radiation exposure to both the patient and the fetus. Another advantage of whole-body MRA/MRV is its utility in searching for arteriovenous malformations (AVMs) of the brain and various types of spinal cord vascular lesions like hemangiomas or AVMs.
Diagnosis of Tumors and Metastases
In clinical oncology, there is a wide range of situations where it is necessary to identify or exclude the presence of metastases in a cancer patient. This information is critical for accurate staging and determining the most appropriate treatment strategy (e.g., surgery, chemotherapy, radiation therapy, or a combination). Traditionally, the search for metastases involved multiple imaging modalities, such as skeletal scintigraphy (bone scan), computed tomography (CT) of the chest/abdomen/pelvis, ultrasound, and laboratory blood tests for tumor markers, depending on the primary tumor type.
Regional MRI has also been traditionally used for targeted diagnosis of metastases in various organs, such as:
- Metastases in regional lymph nodes.
- Liver metastases.
- Brain metastases.
- Spinal metastases.
Modern WB-MRI is now increasingly available and utilized as a single imaging modality to detect Stage M (metastatic) disease throughout the body. WB-MRI can effectively detect bone marrow infiltration by lymphoma, metastases from various primary cancers, and infections like osteomyelitis. This diagnostic method can also reveal damage to parenchymal organs. Thus, WB-MRI can, in many scenarios, replace or complement scintigraphy and CT for metastatic workup. Metastases to vertebral bodies are often more clearly distinguishable and characterized on MRI (especially with diffusion-weighted sequences) than on bone scintigraphy, which primarily detects osteoblastic activity.
The three-dimensional volumetric images obtained with WB-MRI, especially after the injection of contrast, often possess high resolution. They can characterize the degree of damage or involvement of an internal organ's parenchyma, bone, or soft tissue much more effectively than some other global techniques. With WB-MRI, it is possible to examine not only bones but also the lungs (though CT remains superior for fine parenchymal detail), abdominal organs, and lymph nodes and ducts systemically. WB-MRI, particularly with DWIBS sequences, can detect almost all significant lung and brain metastases that would be visible on CT. Compared to scintigraphy, the vertebrae and pelvic bones are generally better visualized for metastatic marrow disease on MRI. A WB-MRI scan for metastatic survey can often be completed within a reasonable timeframe (e.g., 30-60 minutes depending on protocol), making this method a viable alternative to scintigraphy when searching for metastases, especially when soft tissue or marrow detail is important.
Positron Emission Tomography combined with Computed Tomography (PET-CT) and WB-MRI often show similar diagnostic results when searching for distant metastases in many cancer types. MRI is generally preferred when searching for bone marrow or liver metastases due to its superior soft tissue contrast and ability to detect marrow infiltration. However, it should be borne in mind that MRI might have limitations in accurately assessing tumor stage T (local tumor extent) and N (lymph node involvement) for some specific primary tumors compared to dedicated regional imaging or PET-CT, and there can be a risk of overdiagnosis or misinterpretation of certain benign findings. If PET-CT is not available or feasible, or if repeated examinations are necessary in children (due to the high radiation risk from repeated CT exposure), WB-MRI can be an acceptable and valuable alternative. MRI is also particularly relevant for patients with an allergy to iodine-containing contrast agents (idiosyncrasy), which are administered intravenously with CT scans.
Patient Preparation, Procedure, and Safety
Preparation for WB-MRI is similar to regional MRI. Patients are screened for contraindications like incompatible metallic implants (pacemakers, certain aneurysm clips, cochlear implants) or claustrophobia. All external metallic objects must be removed. Fasting for 4-6 hours may be required, especially if contrast is used or abdominal/pelvic regions are a key focus. The procedure involves lying still on a table that moves through the MRI scanner. The duration can be longer than regional scans, ranging from 45 minutes to over an hour, depending on the protocol. Intravenous gadolinium-based contrast is often used, particularly for oncological or vascular indications.
WB-MRI does not involve ionizing radiation. The main risks are associated with the strong magnetic field (interaction with metallic implants) and, rarely, allergic reactions to gadolinium contrast or nephrogenic systemic fibrosis in patients with severe renal impairment (a very low risk with current agents and screening).
Advantages and Limitations of WB-MRI
Advantages:
- Comprehensive, whole-body assessment in a single session.
- No ionizing radiation.
- Excellent soft tissue contrast.
- Superior for detecting bone marrow infiltration (metastases, lymphoma) compared to bone scintigraphy.
- Good for systemic vascular assessment with WB-MRA.
- Valuable alternative when CT contrast is contraindicated.
Limitations:
- Long scan times can lead to motion artifacts.
- High cost and limited availability compared to CT or ultrasound.
- Lower spatial resolution for lung parenchyma compared to CT.
- Large volume of data requires careful interpretation, potential for incidental findings.
- Standard MRI contraindications apply (metallic implants, claustrophobia).
- Not all pathologies are equally well visualized across all body regions with a single "generic" protocol; often tailored sequences are still needed for specific questions.
Comparison with Other Whole-Body Imaging Modalities
| Modality | Primary Use for Whole-Body Assessment | Radiation | Strengths | Weaknesses |
|---|---|---|---|---|
| Whole-Body MRI (WB-MRI) | Metastatic screening (bone marrow, liver, soft tissues), lymphoma staging, systemic vascular disease (WB-MRA), multiple myeloma. | No | Excellent soft tissue & bone marrow contrast, no radiation, versatile sequences (DWI, MRA). | Long scan time, cost, motion artifacts, poor for lung parenchyma detail, MRI contraindications. |
| PET-CT | Cancer staging, restaging, treatment response, detecting metabolically active disease. | Yes (from CT & PET tracer) | Combines metabolic (PET) and anatomical (CT) information, highly sensitive for many cancers. | Radiation, cost, availability, false positives from inflammation, some tumors have low FDG uptake. |
| Skeletal Scintigraphy (Bone Scan) | Detecting bone metastases, osteomyelitis, fractures. | Yes (from tracer) | Sensitive for osteoblastic activity, relatively inexpensive for whole skeleton. | Low specificity (detects various causes of bone turnover), poor anatomical detail, radiation. Less sensitive for lytic or marrow-only metastases compared to MRI. |
| Whole-Body CT (WBCT) | Trauma (pan-scan), some cancer staging protocols (less common now for primary whole-body screening for unknown primary or mets compared to PET-CT or WB-MRI). | Yes (high dose) | Fast, excellent for bone, lung parenchyma, acute hemorrhage/trauma. | High radiation dose, poorer soft tissue contrast than MRI. Iodinated contrast risks. |
Conclusion: The Expanding Role of WB-MRI
Whole-Body MRI, including WB-MRA and specialized oncologic protocols, is a rapidly evolving field. As technology improves and clinical experience grows, its applications are expanding, offering a comprehensive, radiation-free alternative or adjunct to other imaging modalities for systemic disease assessment, particularly in oncology, vascular medicine, and rheumatology (for inflammatory arthropathies). Its ability to provide both anatomical and functional information across large body regions in a single examination underscores its significant diagnostic potential.
References
- Lauenstein TC, Goehde SC, Herborn CU, et al. Whole-body MR imaging: evaluation of patients for metastases. Radiology. 2004 Nov;233(2):139-48.
- Schmidt GP, Baur-Melnyk A, Haug A, et al. Whole-body MRI and PET-CT in the diagnosis of bone metastases in patients with breast cancer. Eur J Nucl Med Mol Imaging. 2008 Jun;35(6):1321-30.
- Kellenberger CJ, Epelman M, Miller SF, Babyn PS. Whole-body MR imaging in children: principles, technique, and clinical applications. Radiographics. 2004 Nov-Dec;24(6):1099-115.
- Bley TA, Uhl M, Fikry S, et al. Diagnostic value of whole-body magnetic resonance angiography: a prospective study. J Am Coll Cardiol. 2008 Nov 4;52(19):1593-601.
- Takeuchi M, Matsuzaki K, Nishitani H. Diffusion-weighted magnetic resonance imaging of bone marrow: a new approach for evaluating bone marrow changes in patients with lymphoma. J Magn Reson Imaging. 2006 Mar;23(3):359-65. (Context for DWIBS)
- Goo HW, Choi SH, Ghim T, et al. Whole-body MRI of paediatric lymphoma: comparison with PET-CT. Pediatr Radiol. 2007 Aug;37(8):739-51.
- Walker RE, Lauenstein TC, Knopp MV. Whole body magnetic resonance imaging. Eur J Radiol. 2006 Dec;60(3):393-9.
- Koh DM, Collins DJ. Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol. 2007 Jun;188(6):1622-35.
See also
- Magnetic Resonance Imaging (MRI)
- Magnetic Resonance Angiography (MRA) of the Cerebral Vessels
- Magnetic Resonance Imaging (MRI) of the Abdomen
- Magnetic Resonance Imaging (MRI) of the Brain
- Magnetic Resonance Imaging (MRI) of the Cervical Spine
- Magnetic Resonance Imaging (MRI) of the Hip Joint
- Magnetic Resonance Imaging (MRI) of the Knee Joint
- Magnetic Resonance Imaging (MRI) of the Lumbar Spine
- Magnetic Resonance Imaging (MRI) of the Pelvic Organs
- Magnetic Resonance Imaging (MRI) of the Pituitary Gland (Hypophysis)
- Magnetic Resonance Imaging (MRI) of the Shoulder Joint
- Magnetic Resonance Imaging (MRI) of the Thoracic Cavity Organs
- Magnetic Resonance Imaging (MRI) of the Thoracic Spine
- Magnetic Resonance Imaging (MRI) Study Principle
- Whole-Body Magnetic Resonance Imaging (MRI)