Magnetic Resonance Imaging (MRI) of the Hip Joint
Understanding Magnetic Resonance Imaging (MRI) of the Hip Joint
Magnetic Resonance Imaging (MRI) of the hip joint is a highly advanced and non-invasive medical imaging technique that utilizes strong magnetic fields, radiofrequency waves, and sophisticated computer algorithms to generate detailed cross-sectional images of the hip joint's complex anatomy. It is recognized as one of the most promising and rapidly advancing methods in modern diagnostics for evaluating a wide array of hip pathologies, encompassing bone, cartilage, labrum, tendons, ligaments, and surrounding soft tissues.
Diagnostic Capabilities and Principles
When performing an MRI of the hip joint, physicians are able to meticulously investigate not only structural abnormalities and pathological changes but also to evaluate certain physicochemical and pathophysiological processes occurring within the entire hip joint or its specific components. MRI provides exceptional soft tissue contrast, allowing for detailed visualization of:
- Articular Cartilage: Covering the femoral head and acetabulum, for detecting thinning, defects, chondromalacia, and osteochondral lesions.
- Acetabular Labrum: The fibrocartilaginous rim around the acetabulum (hip socket), for identifying tears, degeneration, and paralabral cysts.
- Bones: Femoral head and neck, acetabulum, and surrounding pelvic bones for fractures (especially occult or stress fractures), bone marrow edema (contusions), osteonecrosis (avascular necrosis), tumors, and signs of osteoarthritis or inflammatory arthritis.
- Tendons: Including the gluteal tendons (medius and minimus), hamstring origin, iliopsoas tendon, and adductor tendons for tendinopathy, tears, or bursitis associated with them.
- Ligaments: Such as the ligamentum teres and capsular ligaments, for sprains or tears.
- Muscles: Surrounding the hip for strains, tears, atrophy, or masses.
- Synovium and Joint Fluid: Detecting synovitis (inflammation of the joint lining), joint effusions, or loose bodies.
- Bursae: Such as the trochanteric bursa, iliopsoas bursa, or ischial bursa for bursitis.
- Nerves and Blood Vessels: In the vicinity of the hip joint, such as the sciatic nerve or femoral neurovascular bundle, especially if impingement or involvement by a mass is suspected.
Video explaining the hip MRI procedure and what patients might experience.
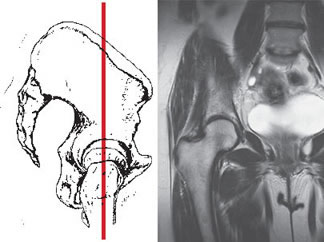
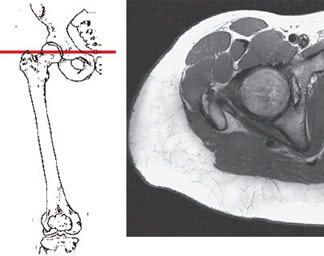
Imaging Reconstruction and Surgical Planning
MRI of the hip joint allows for the acquisition of a series of thin slices in multiple anatomical planes (typically axial, coronal, and sagittal, with oblique planes sometimes added for specific structures like the labrum). These images can be processed by computer software to create three-dimensional (3D) reconstructions of the hip joint and surrounding area. This advanced visualization can also highlight the vasculature (when MRA sequences are employed) and even help delineate individual nerve trunks and blood vessels passing in the projection of the hip joint.
Such detailed hardware-assisted reconstructions from an MRI scan provide invaluable assistance to orthopedic surgeons or traumatologists in precisely planning surgical interventions on the hip (e.g., arthroscopy for labral repair or femoroacetabular impingement, hip replacement, fracture fixation) and for subsequent postoperative monitoring of the patient's condition and healing progress. Early and accurate diagnosis with MRI allows for the prompt initiation of appropriate treatment, which can significantly improve outcomes.
Technology and Contrast Enhancement
The ability of MRI to simultaneously demonstrate the joint itself (articular surfaces, labrum, ligaments, capsule) and the surrounding soft tissues (muscles, tendons, bursae) over a large area is a key strength. This is typically achieved without the need for intra-articular contrast agent injection for many common indications, and importantly, without using ionizing radiation (unlike X-rays or CT scans). MRI can effectively determine the localization and size of soft tissue tumors, assess the cartilaginous surfaces, and evaluate the integrity of muscles and tendons.
Currently, MRI of the hip joint has become a primary diagnostic tool for many diseases and injuries of the hip, often providing significantly more comprehensive information than X-rays or CT scans, especially for soft tissue pathologies. High-field MRI scanners (e.g., 1.5T or 3.0T) are preferred for their superior image quality. Intravenous gadolinium-based contrast (e.g., Omniscan, though specific agents vary) may be used to enhance the visual difference between healthy tissue and pathological processes like tumors, inflammation (synovitis), or infection. MR Arthrography, which involves injecting dilute gadolinium contrast directly into the hip joint under imaging guidance (fluoroscopy or ultrasound) before the MRI scan, is particularly useful for detecting subtle labral tears, loose bodies, or cartilage defects. Patient weight restrictions (e.g., up to 200 kg) are applicable to most MRI scanners.
Clinical Indications for Hip MRI
A physician may order an MRI examination of the hip joint in various clinical scenarios, including but not limited to:
- Arthritis of the hip: Including osteoarthritis, inflammatory arthritis (e.g., rheumatoid arthritis, ankylosing spondylitis), and septic arthritis.
- Osteoarthritis (Coxarthrosis) of the hip joint: To assess cartilage loss, bone spurs, subchondral cysts, and associated soft tissue changes.
- Avascular Necrosis (Osteonecrosis) of the Femoral Head: MRI is highly sensitive for detecting early stages of bone death due to compromised blood supply.
- Labral Tears: Tears of the acetabular labrum, often associated with femoroacetabular impingement (FAI) or trauma.
- Femoroacetabular Impingement (FAI): To assess for cam or pincer morphologies and associated labral/cartilage damage.
- Tendon and Muscle Injuries: Tears or tendinopathy of the gluteal tendons (medius, minimus), hamstring origin, iliopsoas tendon, or adductor muscles.
- Ligamentous Injuries: Sprains or tears of hip ligaments, including the ligamentum teres.
- Bursitis: Trochanteric bursitis, iliopsoas bursitis, ischial bursitis.
- stress fractures or Occult Fractures: Especially in athletes or individuals with osteoporosis, when X-rays are negative.
- Soft tissue injuries of the hip joint: Including damage to the joint capsule.
- Hip dislocation: To assess for associated soft tissue and bony injuries after reduction.
- Tumors: Evaluation of primary bone or soft tissue tumors, or metastases of tumor cells in the area of the hip joint. Intravenous contrast is often used.
- Infections: Osteomyelitis, septic arthritis, soft tissue abscesses.
- Snapping Hip Syndrome: To identify the cause (e.g., iliopsoas tendon, iliotibial band).
- Transient Osteoporosis of the Hip.
- Pediatric Hip Conditions: Legg-Calvé-Perthes disease, slipped capital femoral epiphysis (SCFE), developmental dysplasia of the hip (DDH) complications.
- Unexplained Hip, Groin, or Buttock Pain unresponsive to conservative management or when the diagnosis is unclear after initial evaluation.
Common Pathologies Visualized with Hip MRI
Hip MRI is adept at identifying a wide spectrum of pathologies:
- Labral Tears: Clearly delineates tears, their location, and associated paralabral cysts.
- Cartilage Defects: Shows thinning, fibrillation, or full-thickness loss of articular cartilage.
- Avascular Necrosis: Highly sensitive for early detection before changes are visible on X-ray, showing characteristic bone marrow edema patterns and subchondral collapse.
- Tendon Tears/Tendinopathy: Especially of the gluteus medius/minimus (abductor tendons) and hamstrings.
- Femoroacetabular Impingement (FAI): Visualizes cam and pincer deformities and associated chondrolabral damage.
- stress fractures: Detects subtle fractures not seen on X-rays, particularly in the femoral neck.
- Synovitis and Effusions: Indicates joint inflammation or fluid accumulation.
- Bursitis: Inflammation of bursae around the hip.
- Soft Tissue Masses/Tumors: Characterizes benign and malignant soft tissue and bone tumors.
Patient Preparation and Procedure for Hip MRI
Preparation for a hip MRI is generally minimal:
- Screening: Patients complete a comprehensive safety questionnaire to check for MRI contraindications (e.g., incompatible pacemakers, certain aneurysm clips, cochlear implants, severe claustrophobia, known gadolinium allergy, severe renal impairment if contrast is planned).
- Metal Objects: All removable ferromagnetic items (jewelry, watches, belts, coins, hairpins, etc.) must be removed.
- Clothing: Patients are usually asked to change into a hospital gown to avoid any metal fasteners or fibers in their clothing that could interfere with the scan.
- Fasting: Not typically required for a standard hip MRI without IV contrast or sedation. If MR Arthrography or IV contrast is planned, specific fasting instructions (usually 4-6 hours) may be given by the imaging facility.
- Contrast Agent: If intravenous gadolinium-based contrast or intra-articular contrast (for MR Arthrography) is to be used, an IV line may be placed, or the joint will be injected under fluoroscopic or ultrasound guidance prior to the MRI. Patients must inform staff of any allergies (especially to contrast media) or history of kidney disease.
During the procedure, the patient lies supine (on their back) on the MRI examination table. A specialized surface coil designed for hip or pelvic imaging is placed over or around the hip region to optimize signal reception and image quality. The table then slides into the bore (tunnel) of the MRI scanner. The patient must remain as still as possible during the scan, which typically lasts between 30 and 60 minutes, depending on the number of sequences performed and whether contrast material is administered. The MRI scanner produces loud tapping, banging, or knocking sounds during operation; earplugs or headphones are provided to reduce noise and enhance patient comfort. The MRI technologist will communicate with the patient via an intercom system throughout the scan.
Advantages and Limitations of Hip MRI
Advantages:
- Excellent soft tissue contrast, superior for visualizing cartilage, labrum, tendons, ligaments, muscles, and bone marrow.
- No ionizing radiation exposure, making it safe for repeated studies and for pediatric or pregnant patients (though typically avoided in the first trimester of pregnancy unless absolutely essential).
- Multiplanar imaging capability (sagittal, axial, coronal, and oblique views) without repositioning the patient.
- Highly sensitive for detecting a wide range of pathologies, including early osteonecrosis, stress fractures, labral tears, and tendinopathies that may not be visible on X-ray or ultrasound.
- Can guide treatment decisions, including the need for conservative management versus surgical intervention, and aids in precise surgical planning.
- Non-invasive evaluation for standard MRI; MR Arthrography is minimally invasive.
Limitations:
- Higher cost compared to X-ray or ultrasound.
- Longer scan times, making it more susceptible to motion artifacts if the patient is unable to remain still.
- Less sensitive than X-ray or CT for evaluating fine cortical bone detail or acute fractures in some instances (though excellent for bone marrow edema/bruises and stress fractures).
- Contraindicated in patients with certain incompatible metallic implants (e.g., older pacemakers, certain aneurysm clips) or ferromagnetic foreign bodies.
- Can be challenging for claustrophobic patients or those who have difficulty lying supine for the required duration.
- MRI findings (e.g., asymptomatic labral tears or cartilage fraying) are relatively common in certain age groups and may not always correlate directly with the patient's clinical symptoms, necessitating careful clinical correlation by the referring physician.
- Interpretation requires specialized expertise in musculoskeletal radiology.
- MR Arthrography, while providing enhanced detail for certain intra-articular structures, is an invasive procedure involving joint injection, with associated small risks (e.g., infection, pain, contrast reaction).
Comparison with Other Hip Imaging Modalities
| Modality | Principle | Radiation | Primary Strengths for Hip Imaging | Primary Weaknesses for Hip Imaging |
|---|---|---|---|---|
| Hip MRI / MR Arthrography | Magnetic fields, radio waves | No | Labrum, cartilage, tendons, ligaments, bone marrow (osteonecrosis, stress fractures, edema), synovitis, soft tissue masses. MR Arthrography for subtle labral/cartilage tears. | Cost, scan time, motion sensitivity, less detail for cortical bone fractures. Arthrography is invasive. |
| Hip X-ray (Radiography) | X-rays | Yes (low dose) | Bone fractures, dislocations, alignment, osteoarthritis (joint space narrowing, osteophytes), Legg-Calvé-Perthes, SCFE, bone density (qualitative). Inexpensive, fast, widely available. | Poor visualization of soft tissues (labrum, cartilage, tendons, ligaments), insensitive to early osteonecrosis or stress fractures. |
| Hip CT Scan / CT Arthrography | X-rays | Yes (higher dose) | Complex bone fractures, detailed bony anatomy (e.g., for FAI morphology, pre-op planning for joint replacement), loose bodies, bone tumors. CT Arthrography for labral/cartilage if MRI contraindicated. | Radiation, poorer soft tissue contrast than MRI. Iodinated contrast risks if used. |
| Hip Ultrasound | Sound waves | No | Superficial soft tissues (tendons like iliopsoas, gluteals; bursae), joint effusions, developmental dysplasia of the hip (DDH) in infants, dynamic assessment. Guiding aspirations/injections. | Operator dependent, limited view of intra-articular structures (deep labrum, deep cartilage), cannot see through bone well. Limited by patient habitus. |
| Bone Scan (Scintigraphy) | Radiotracer uptake | Yes (from tracer) | Detecting areas of increased bone turnover (stress fractures, osteonecrosis, infection, metastases, inflammatory arthritis). Highly sensitive but often non-specific. | Radiation, poor anatomical detail. Often requires correlation with other imaging. |
The Importance of MRI in Managing Hip Conditions
MRI of the hip joint has become an invaluable diagnostic tool in orthopedics, sports medicine, and rheumatology. Its superior ability to visualize soft tissue structures, bone marrow, and subtle pathological changes allows for early and accurate diagnosis of a wide spectrum of hip disorders. This detailed diagnostic information is crucial for formulating effective and individualized treatment plans, guiding decisions between conservative management and surgical intervention, facilitating precise surgical planning when necessary, and monitoring treatment outcomes. Ultimately, hip MRI contributes significantly to improving patient care, optimizing functional recovery, and enhancing the long-term prognosis for individuals suffering from hip pain and dysfunction.
References
- Stoller DW. Magnetic Resonance Imaging in Orthopaedics and Sports Medicine. 3rd ed. Lippincott Williams & Wilkins; 2007.
- Resnick D, Kang HS, Pretterklieber ML. Internal Derangements of Joints. 2nd ed. Saunders Elsevier; 2007. Chapter on Hip.
- Blankenbaker DG, De Smet AA. MR arthrography of the hip. Radiol Clin North Am. 2004 Jul;42(4):757-73.
- Kaplan PA, Helms CA, Dussault R, Anderson MW. Musculoskeletal MRI. 2nd ed. Saunders; 2001.
- Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007 Aug;15(8):1041-7. (Context for FAI imaging)
- American College of Radiology. ACR Appropriateness Criteria® Chronic Hip Pain. Last review date: 2018.
- Steinbach LS, Palmer WE, Schweitzer ME. Special focus session. MR arthrography. Radiographics. 2002 Sep-Oct;22(5):1223-46.
- Kassarjian A, Yoon LS, Belzile E, Connolly SA, Millis MB, Palmer WE. Triad of MR arthrographic findings in patients with cam-type femoroacetabular impingement. Radiology. 2005 May;235(2):588-95.
See also
- Magnetic Resonance Imaging (MRI)
- Magnetic Resonance Angiography (MRA) of the Cerebral Vessels
- Magnetic Resonance Imaging (MRI) of the Abdomen
- Magnetic Resonance Imaging (MRI) of the Brain
- Magnetic Resonance Imaging (MRI) of the Cervical Spine
- Magnetic Resonance Imaging (MRI) of the Hip Joint
- Magnetic Resonance Imaging (MRI) of the Knee Joint
- Magnetic Resonance Imaging (MRI) of the Lumbar Spine
- Magnetic Resonance Imaging (MRI) of the Pelvic Organs
- Magnetic Resonance Imaging (MRI) of the Pituitary Gland (Hypophysis)
- Magnetic Resonance Imaging (MRI) of the Shoulder Joint
- Magnetic Resonance Imaging (MRI) of the Thoracic Cavity Organs
- Magnetic Resonance Imaging (MRI) of the Thoracic Spine
- Magnetic Resonance Imaging (MRI) Study Principle
- Whole-Body Magnetic Resonance Imaging (MRI)