Magnetic Resonance Imaging (MRI) of the Brain
- Understanding Magnetic Resonance Imaging (MRI) of the Brain
- Clinical Indications for Brain MRI
- Common MRI Sequences and Their Utility
- Patient Preparation and Procedure
- Advantages and Limitations of Brain MRI
- Interpreting Brain MRI Findings: Examples
- Comparison with Other Neuroimaging Modalities
- The Role of Brain MRI in Diagnosis and Treatment Planning
- References
Understanding Magnetic Resonance Imaging (MRI) of the Brain
Magnetic Resonance Imaging (MRI) of the brain stands as one of the most promising, versatile, and rapidly advancing methods in modern neuroradiology. It is a non-invasive imaging technique that uses a strong magnetic field, radiofrequency pulses, and sophisticated computer algorithms to generate highly detailed cross-sectional images of the brain and its surrounding structures.
Principles and Capabilities
Brain MRI provides physicians with an unparalleled opportunity to investigate structural abnormalities and pathological changes within the patient's brain tissue. It allows for the appreciation of intricate anatomical details and the assessment of various physicochemical and pathophysiological processes affecting the entire brain or its individual structures. The excellent soft tissue contrast of MRI enables clear differentiation between gray matter, white matter, cerebrospinal fluid (CSF), blood vessels, and various pathological lesions.
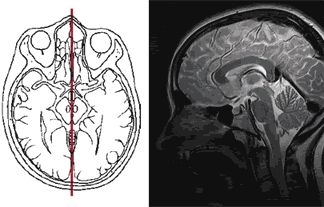
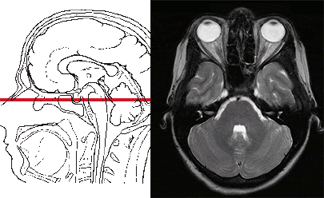
MRI can obtain a series of thin slices (sections) in multiple planes (axial, sagittal, coronal, and oblique) without repositioning the patient. These slices can then be used to construct three-dimensional (3D) reconstructions of the brain or specific areas of interest. This capability is invaluable for neurosurgeons in planning complex operations and for subsequent postoperative monitoring and control of treatment efficacy.
Advanced MRI Techniques (MRA, Functional MRI)
Beyond standard anatomical imaging, MRI of the brain allows for specialized studies:
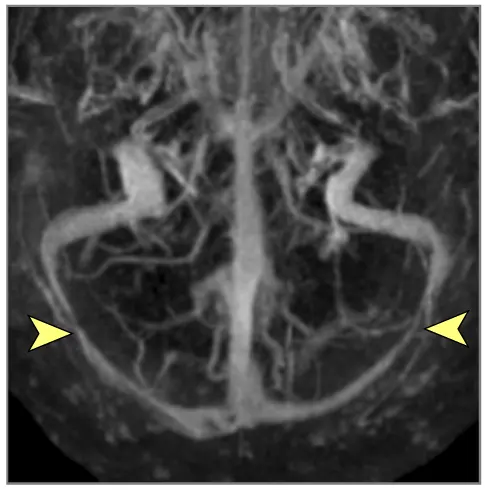
- Magnetic Resonance Angiography (MRA): This technique specifically visualizes the blood vessels of the brain (arteries and veins), often without the need for direct arterial puncture or contrast injection (though contrast can be used for enhanced MRA). It helps in detecting aneurysms, arteriovenous malformations (AVMs), stenosis, or occlusions.
- Functional MRI (fMRI): This technique can conduct functional studies of the brain by detecting changes in local brain activity based on blood flow (Blood-Oxygen-Level Dependent - BOLD contrast). It is used in research and clinical settings to map brain areas responsible for specific functions like language, motor control, or vision.
- Diffusion-Weighted Imaging (DWI) and Diffusion Tensor Imaging (DTI): DWI is highly sensitive for detecting acute ischemic stroke within minutes of onset. DTI allows for the visualization of white matter tracts and their integrity.
- Perfusion MRI: Measures blood flow and blood volume in brain tissue, useful in stroke, tumors, and other conditions affecting cerebral perfusion.
- MR Spectroscopy (MRS): Provides information about the chemical composition (metabolites) within a region of interest in the brain, which can help differentiate tumor types, assess metabolic disorders, or identify areas of neuronal injury.
MRI also allows for excellent visualization of the ventricular system (fluid-filled cavities within the brain), cisterns at the base of the skull, and other spaces containing cerebrospinal fluid (CSF), enabling assessment of their volume, position, and any abnormalities like hydrocephalus.
Video demonstrating the concept of 3D amplified MRI (aMRI), showcasing advanced visualization capabilities.
Safety and Technology
A key advantage of brain MRI is its safety profile concerning radiation. Unlike CT scans or X-rays, MRI does not use ionizing radiation, making it a safer option for repeated imaging or for vulnerable populations when appropriate. High-field MRI scanners (e.g., 1.5 Tesla or 3.0 Tesla) are commonly used for brain imaging to achieve high-resolution images. Intravenous contrast agents (gadolinium-based) can be administered to enhance the visibility of certain structures or pathologies, such as tumors or areas of inflammation, by increasing the visual difference between healthy and abnormal tissue. Patient weight limitations (e.g., up to 200 kg) exist for most scanners.
The ability of MRI to simultaneously demonstrate structures like the spinal cord and spine along the cervical region without contrast agents in the spinal spaces (unlike myelography) and without ionizing radiation further underscores its diagnostic power. It can effectively determine the localization and size of tumors, assess the state of intervertebral discs, facet joints, and vertebral bodies in this region if included in the scan field.
Currently, MRI of the brain has become a primary diagnostic tool for most diseases of the brain and its vasculature, often surpassing or complementing other methods like CT scans or more invasive procedures like conventional angiography or myelography.
Clinical Indications for Brain MRI
A brain MRI may be prescribed by a physician for a wide range of suspected or known neurological conditions. Common indications include, but are not limited to:
- Evaluation of the general anatomy of the nervous system.
- Central Nervous System Infections:
- Suspected Brain abscess (e.g., lobar, cerebellar).
- Evaluation of Eosinophilic granuloma, Langerhans cell histiocytosis (LCH) (which can affect skull bones and rarely brain), or conditions like Hennebert's symptom (vertigo induced by pressure changes, sometimes linked to inner ear/temporal bone issues visible on MRI).
- Suspected Epidural brain abscess.
- Assessment of sinusitis-associated intracranial complications or otogenic (ear-related) intracranial complications.
- Evaluation of sinusitis-associated ophthalmic complications if intracranial extension is queried.
- Diagnosis of bacterial otogenic meningitis and other forms of meningitis or encephalitis.
- Suspected Subdural brain abscess (empyema).
- Evaluation of sigmoid sinus suppurative thrombophlebitis or other dural venous sinus thrombosis.
- Suspected Colloid Cyst of the 3rd Ventricle or other intracranial cysts.
- Assessment of cerebral and spinal adhesive arachnoiditis.
- Investigation of neurodegenerative conditions like Corticobasal Ganglionic Degeneration (Limited Brain Atrophy) and other dementias or movement disorders.
- Evaluation of encephalopathy of various etiologies (e.g., hypoxic, metabolic, toxic).
- Investigation of persistent or unexplained headache or migraine, especially if red flag symptoms are present.
- Assessment of Traumatic Brain Injury (TBI), including concussion, contusion, brain hemorrhage (intracerebral, subdural, epidural), and diffuse axonal injury (axonal shearing lesions).
- Evaluation of increased intracranial pressure (ICP) and hydrocephalus.
- Diagnosis and monitoring of movement disorders like Parkinson's disease (often to rule out other causes or assess for atypical features).
- Evaluation of pituitary gland pathologies, including microadenomas, macroadenomas, nonfunctioning pituitary adenomas (NFPAs), and hyperprolactinemia syndrome.
- Detection of spontaneous cranial cerebrospinal fluid (CSF) leaks (rhinorrhea or otorrhea).
- Diagnosis of demyelinating diseases like Multiple Sclerosis.
- Evaluation of seizures and epilepsy to identify structural causes.
- Assessment of congenital brain malformations.
- Detection and characterization of primary or metastatic brain tumors.
Video illustrating the diagnostic procedure for Magnetic Resonance Imaging (MRI) of the brain, providing insights into what patients can expect.
Common MRI Sequences and Their Utility
A typical brain MRI study involves acquiring images using several different pulse sequences, each providing unique information about brain tissue characteristics:
- T1-Weighted Images (T1W): Provide excellent anatomical detail. Fat appears bright, while water/CSF appears dark. Often used with gadolinium contrast to highlight areas of blood-brain barrier breakdown (e.g., tumors, inflammation, infection).
- T2-Weighted Images (T2W): Highly sensitive to pathology. Water/CSF and edematous/inflamed tissues appear bright, while fat appears relatively dark.
- FLAIR (Fluid Attenuated Inversion Recovery): Similar to T2W images but with the bright signal from CSF suppressed. This makes lesions near CSF spaces (e.g., periventricular white matter lesions in MS) more conspicuous.
- Diffusion-Weighted Imaging (DWI): Highly sensitive for detecting acute ischemic stroke by showing restricted diffusion of water molecules in infarcted tissue. Also useful for characterizing abscesses and some tumors.
- Gradient Echo (GRE) / Susceptibility Weighted Imaging (SWI): Sensitive to blood products (hemorrhage, hemosiderin) and calcifications.
- Post-Contrast T1-Weighted Images: Acquired after intravenous administration of a gadolinium-based contrast agent to highlight areas with increased vascularity or disruption of the blood-brain barrier.
The specific sequences used will depend on the clinical question being addressed.
Patient Preparation and Procedure
Generally, minimal preparation is required for a brain MRI:
- Screening: Patients complete a detailed safety questionnaire to identify any contraindications (e.g., pacemakers, metallic implants, claustrophobia).
- Metal Objects: All metallic items (jewelry, watches, hairpins, removable dental work, clothing with metal) must be removed.
- Fasting: Usually not required for a standard brain MRI without sedation. If contrast or sedation is planned, specific fasting instructions may be given.
- Contrast Agent: If contrast is to be used, an IV line will be inserted. Patients should inform staff of any allergies or kidney problems.
- Procedure: The patient lies on a table that slides into the MRI scanner. They will hear loud knocking/thumping sounds and must remain as still as possible during the scan, which typically lasts 20-60 minutes depending on the number of sequences. Earplugs or headphones are provided.
Advantages and Limitations of Brain MRI
Advantages:
- Excellent soft tissue contrast, superior to CT for many brain pathologies.
- No ionizing radiation exposure.
- Ability to acquire images in multiple planes without repositioning.
- Capability for advanced techniques like MRA, fMRI, DWI, MRS, providing functional and physiological information in addition to anatomy.
- Gadolinium contrast agents generally have a better safety profile than iodinated contrast agents used in CT, especially regarding allergic reactions and nephrotoxicity.
Limitations:
- Higher cost compared to CT.
- Longer scan times, making it more susceptible to motion artifacts.
- Less sensitive than CT for detecting acute hemorrhage (especially subarachnoid) in the first few hours and for visualizing bone fractures or calcifications.
- Contraindicated in patients with certain metallic implants or foreign bodies.
- The enclosed scanner can induce claustrophobia in some patients.
- Loud operating noise.
- Limited availability in some areas compared to CT.
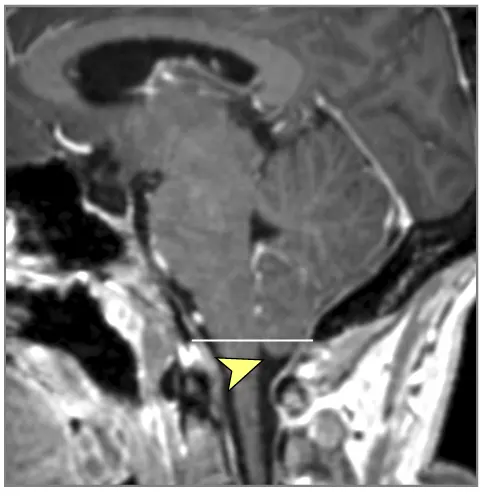
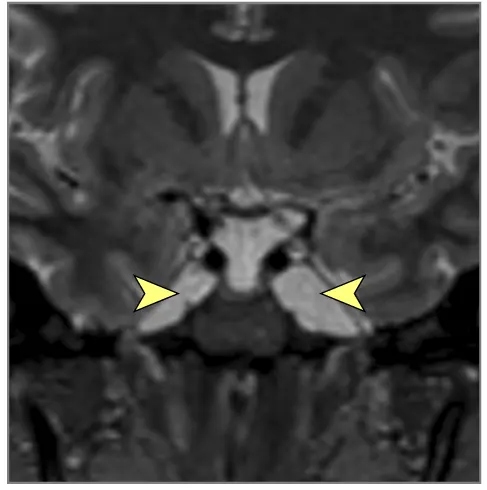
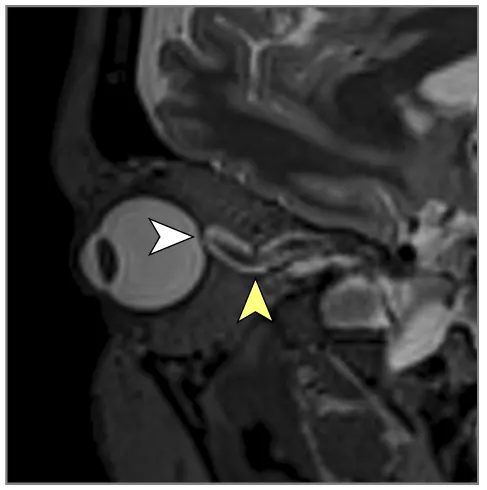
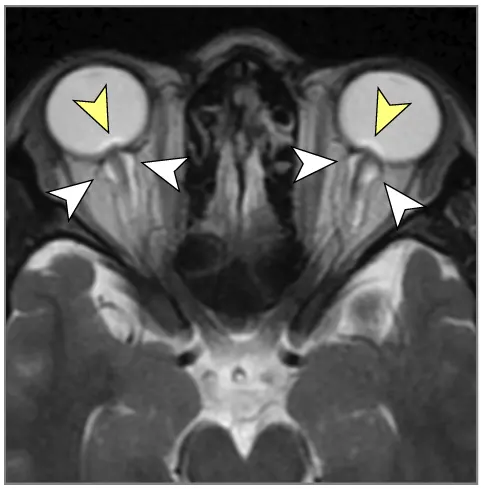
Interpreting Brain MRI Findings: Examples
Brain MRI can reveal a multitude of findings. The images provided illustrate some signs associated with Intracranial Hypertension (elevated pressure within the skull), which can have various underlying causes:
Such detailed three-dimensional reconstructions and multiplanar views of brain tissue obtainable with MRI provide invaluable assistance to neurologists and neurosurgeons in diagnosing conditions, planning complex surgical interventions, and for subsequent postoperative monitoring and assessment of treatment outcomes.
Comparison with Other Neuroimaging Modalities
| Modality | Principle | Radiation | Primary Strengths for Brain Imaging | Primary Weaknesses for Brain Imaging |
|---|---|---|---|---|
| Brain MRI | Magnetic fields, radio waves | No | Excellent soft tissue contrast (gray/white matter, CSF), detects subtle lesions, functional imaging (fMRI, DWI, Perfusion, MRS), MRA for vessels. | Longer scan time, motion sensitive, higher cost, less sensitive for acute hemorrhage/bone detail than CT, MRI contraindications. |
| Computed Tomography (CT) of the Head | X-rays | Yes | Fast, excellent for acute hemorrhage (stroke, trauma), bone fractures, hydrocephalus, widely available. Good for initial assessment in emergencies. | Radiation exposure, poorer soft tissue contrast than MRI, limited for posterior fossa and some tumor types. Iodinated contrast risks. |
| Positron Emission Tomography (PET) Scan | Radiotracer decay, metabolic activity | Yes (from tracer) | Assesses brain metabolism/function (e.g., glucose metabolism, receptor density). Used in oncology (tumor staging, recurrence), dementia (e.g., amyloid/tau imaging), epilepsy focus localization. | Lower spatial resolution than MRI/CT, requires cyclotron for some tracers, expensive, radiation. Often combined with CT (PET-CT) or MRI (PET-MRI) for anatomical correlation. |
| Single Photon Emission Computed Tomography (SPECT) | Radiotracer decay, regional blood flow/receptor binding | Yes (from tracer) | Assesses regional cerebral blood flow (rCBF), useful in stroke, dementia, epilepsy, some psychiatric disorders. | Lower spatial resolution than PET or MRI, radiation. |
| Ultrasound (Transcranial Doppler - TCD) | Sound waves | No | Non-invasive assessment of blood flow velocity in major intracranial arteries, vasospasm monitoring, right-to-left shunt detection. Portable. | Operator dependent, limited by acoustic window (bone), provides physiological not detailed anatomical data. |
The Role of Brain MRI in Diagnosis and Treatment Planning
Early and accurate diagnosis facilitated by brain MRI allows for the timely initiation of appropriate treatment for a wide range of neurological diseases, significantly impacting patient prognosis and quality of life. Its ability to provide detailed anatomical, physiological, and functional information makes it an indispensable tool in modern neuroscience and clinical practice.
References
- Westbrook C, Roth C, Talbot J. MRI in Practice. 5th ed. Wiley-Blackwell; 2018.
- Atlas SW. Magnetic Resonance Imaging of the Brain and Spine. 5th ed. Lippincott Williams & Wilkins; 2016.
- Brant WE, Helms CA. Fundamentals of Diagnostic Radiology. 4th ed. Lippincott Williams & Wilkins; 2012. Chapter: Brain MRI.
- Fischbein NJ, Phillips CD, Kelly HR, et al. ACR Appropriateness Criteria® Suspected Spine Trauma. J Am Coll Radiol. 2017 May;14(5S):S306-S314. (Context for combined imaging)
- Ogawa S, Lee TM, Kay AR, Tank DW. Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proc Natl Acad Sci U S A. 1990 Dec;87(24):9868-72. (Seminal paper on BOLD fMRI)
- Le Bihan D, Mangin JF, Poupon C, et al. Diffusion tensor imaging: concepts and applications. J Magn Reson Imaging. 2001 Apr;13(4):534-46. (DTI principles)
- American College of Radiology. ACR–ASNR–SPR Practice Parameter for the Performance and Interpretation of Magnetic Resonance Imaging (MRI) of the Brain. Revised 2023.
- Patel SH, Koury K, Kliot M, et al. MR imaging of the brain. Radiographics. 2000 May-Jun;20(3):815-30.
See also
- Magnetic Resonance Imaging (MRI)
- Magnetic Resonance Angiography (MRA) of the Cerebral Vessels
- Magnetic Resonance Imaging (MRI) of the Abdomen
- Magnetic Resonance Imaging (MRI) of the Brain
- Magnetic Resonance Imaging (MRI) of the Cervical Spine
- Magnetic Resonance Imaging (MRI) of the Hip Joint
- Magnetic Resonance Imaging (MRI) of the Knee Joint
- Magnetic Resonance Imaging (MRI) of the Lumbar Spine
- Magnetic Resonance Imaging (MRI) of the Pelvic Organs
- Magnetic Resonance Imaging (MRI) of the Pituitary Gland (Hypophysis)
- Magnetic Resonance Imaging (MRI) of the Shoulder Joint
- Magnetic Resonance Imaging (MRI) of the Thoracic Cavity Organs
- Magnetic Resonance Imaging (MRI) of the Thoracic Spine
- Magnetic Resonance Imaging (MRI) Study Principle
- Whole-Body Magnetic Resonance Imaging (MRI)