Rhinogenic orbital and intracranial complications
- Understanding Rhinogenic Orbital and Intracranial Complications
- Rhinogenic Orbital Complications
- Rhinogenic Intracranial Complications
- Differential Diagnosis of Orbital and Intracranial Symptoms
- Prevention and When to Seek Urgent Multidisciplinary Care
- References
Understanding Rhinogenic Orbital and Intracranial Complications
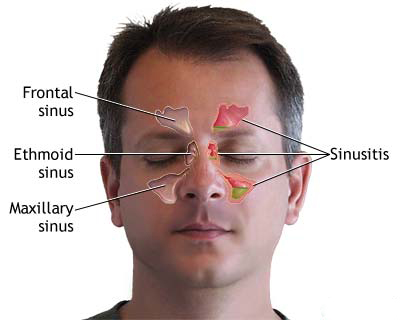
Rhinogenic orbital and intracranial complications are serious, potentially life-threatening conditions that arise when infections originating in the nasal cavity or paranasal sinuses spread to the adjacent orbit (eye socket) or cranial cavity (containing the brain). The close anatomical proximity of these structures, shared bony walls (which can be thin or dehiscent), a well-developed vascular network with valveless veins facilitating bidirectional blood flow, and lymphatic connections create pathways for infection to extend beyond the sinuses.
Pathways of Infection Spread
Infection can penetrate into the orbit or cranial cavity via several routes:
- Direct Extension (Contact Spread): Infection can erode through the thin bony walls separating the sinuses from the orbit (e.g., lamina papyracea of the ethmoid sinus, floor of the frontal sinus, roof of the maxillary sinus) or the cranial cavity (e.g., posterior wall of the frontal sinus, roof of the ethmoid or sphenoid sinuses). This is common with aggressive sinus infections or if there are pre-existing bony defects (congenital or post-traumatic).
- Hematogenous Spread: Bacteria can enter the bloodstream from the infected sinus mucosa and travel to the orbit or brain, often via the valveless diploic veins of the skull or through thrombophlebitis (inflammation and clotting) of communicating veins.
- Perineural Spread: Infection can track along cranial nerves that pass through or near the sinuses.
- Lymphogenous Spread: Spread through lymphatic channels, though less common for these specific complications.
Congenital bony defects or dehiscent sutures can also serve as pre-existing pathways for infection spread, especially in children.
Rhinogenic Orbital Complications
Predisposing Factors and Overview
Rhinogenic orbital complications are more frequently associated with acute ethmoiditis, particularly in children, but can arise from infections in any paranasal sinus (frontal, maxillary, sphenoid). They can occur during acute infectious diseases like influenza, measles, or scarlet fever, which often involve severe rhinosinusitis. In early childhood, acute osteomyelitis of the maxilla, rather than primary sinusitis, may predominate and often presents with orbital complications.
Orbital complications are often preceded by reactive edema (inflammatory swelling) of the eyelids and orbital tissues, or diffuse non-suppurative inflammation (preseptal or orbital cellulitis) before distinct abscess formation.
Conventionally, rhinogenic orbital complications are classified into several forms, based on the Chandler classification or similar systems:
- Preseptal Cellulitis (Periorbital Cellulitis): Inflammation anterior to the orbital septum.
- Orbital Periostitis/Osteoperiostitis
- Subperiosteal Abscess
- Eyelid Abscess (often a component of preseptal or subperiosteal processes)
- Eyelid and Orbital Wall Fistula
- Orbital Cellulitis (Phlegmon)
- Retrobulbar Abscess (often considered part of orbital cellulitis/abscess spectrum)
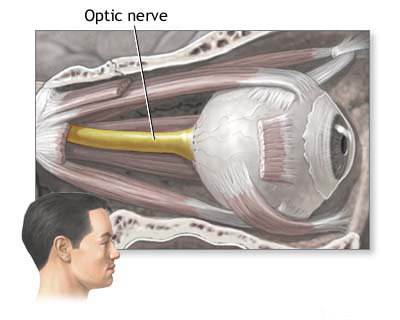
- Optic Neuritis
- Cavernous Sinus Thrombosis (also an intracranial complication)
Orbital Periostitis/Osteoperiostitis
Orbital periostitis, inflammation of the periosteum lining the bony orbit, typically develops secondary to inflammation of the adjacent sinus bone wall (osteitis), hence the term osteoperiostitis. It can occur with acute sinusitis or during an exacerbation of chronic sinusitis. Systemic symptoms like fever, headache, and general weakness are common. Clinical signs depend on the affected orbital wall and originating sinus:
- Typical Signs: Swelling of the eyelids, chemosis (conjunctival swelling), and exophthalmos (protrusion of the eyeball) with displacement of the eye away from the site of the lesion (e.g., downward and outward displacement with frontal or ethmoid involvement).
- Ethmoid Sinus Origin: Eyelid swelling is often most pronounced medially (inner part of the eye).
- Maxillary Sinus Origin: Relatively rare to cause osteoperiostitis. If the inferior orbital rim or anterior orbital floor is involved, the lower eyelid and lower conjunctiva may be swollen.
- Pain on eye movement and localized tenderness over the affected orbital rim may be present.
Subperiosteal Abscess
A subperiosteal abscess is a collection of pus between the bony orbital wall and its periosteal lining. It is essentially the next stage in the progression of suppurative osteoperiostitis. Characteristic features include:
- Pronounced inflammatory changes in the eyelids and conjunctiva (swelling, redness, chemosis).
- Proptosis and displacement of the eyeball.
- Restricted and painful eye movements (ophthalmoplegia).
- Decreased visual acuity may occur due to optic nerve compression or inflammation.
- Fluctuation (a sign of pus collection) is not always palpable, especially with deep-seated abscesses.
- Origin from Anterior Ethmoid Cells: A typical marginal subperiosteal abscess develops in the superomedial (upper inner) corner of the orbit. Initial signs include hyperemia of the medial conjunctiva, followed by outward and downward displacement of the eyeball.
- Origin from Posterior Ethmoid Cells: The leading symptom is often axial proptosis (eyeball pushed straight forward), with lateral displacement and eyelid swelling being secondary signs. Impaired eye mobility and decreased visual acuity are common. Paralysis of the abducens (CN VI) and oculomotor (CN III) nerves can occur with increasing intraorbital pressure. Pain on eye movement or pressure is typical.
Eyelid Abscess
An eyelid abscess as an isolated rhinogenic complication is rare in clinical practice. More commonly, eyelid swelling and abscess formation are part of preseptal cellulitis or an extension of a subperiosteal abscess that points anteriorly.
Eyelid and Orbital Wall Fistula
Fistulas (abnormal tracts) opening onto the skin of the upper eyelid or at the root of the nose are usually caused by chronic inflammation of the ethmoid or frontal sinuses. The fistula represents the endpoint of a chronic suppurative process in the sinus that has eroded through the bone and soft tissues to drain externally. These are typically manifestations of chronic sinus suppuration, often with a torpid (sluggish) course and less pronounced acute inflammation from the orbit and eyelids at the time of fistula presentation.
Retrobulbar Abscess
A retrobulbar abscess is a localized collection of pus within the orbital soft tissues behind the eyeball (in the orbital fat/muscle cone). It often develops as an extension of a subperiosteal abscess or orbital cellulitis. It typically presents with:
- Severe systemic reaction: high fever, chills, significant changes in blood counts (leukocytosis).
- Pronounced axial proptosis.
- Severe limitation of eye mobility (ophthalmoplegia).
- Decreased visual acuity, potentially leading to blindness if the optic nerve is compressed or compromised.
- Pain, especially with eye movement.
- The clinical picture can be very similar to severe orbital cellulitis (phlegmon).
Orbital Cellulitis (Phlegmon)
Orbital cellulitis (or orbital phlegmon) is a diffuse, non-localized, progressive acute inflammatory process involving the soft tissues of the orbit posterior to the orbital septum. It is characterized by:
- Significant systemic illness: high fever, chills, headache, prostration.
- Painful proptosis.
- Marked ophthalmoplegia (impaired or complete immobility of the eye).
- Chemosis and eyelid edema, often without a tendency for localized suppuration or abscess pointing (unlike subperiosteal abscess).
- Decreased vision is a serious sign.
It can develop through direct extension from infected sinuses or via hematogenous spread.
Retrorbital Venous Thrombosis
Thrombosis (clotting) of the orbital veins, particularly the superior and inferior ophthalmic veins, is a rare but serious complication. It can lead to marked orbital congestion, proptosis, ophthalmoplegia, and visual loss. It may also predispose to the spread of infection to the cavernous sinus (cavernous sinus thrombosis).
Treatment of Rhinogenic Orbital Complications
Management of rhinogenic orbital complications is a medical emergency and requires a multidisciplinary approach, often involving ENT specialists, ophthalmologists, and sometimes neurosurgeons or infectious disease specialists. The primary focus must be on treating the underlying sinusitis (the primary focus of infection) while concurrently addressing the orbital complication.
Treatment strategies depend on the specific type and severity of the orbital complication and the nature of the underlying sinus disease (acute or chronic).
- Medical Management (often initial approach for preseptal cellulitis, early orbital cellulitis, or periostitis without abscess):
- High-Dose Intravenous Antibiotics: Broad-spectrum antibiotics covering common sinus pathogens (*S. pneumoniae, H. influenzae, M. catarrhalis, S. aureus*, anaerobes) should be started immediately. Antibiotic choice may be guided by severity and local resistance patterns.
- Nasal Decongestants: Topical and sometimes systemic decongestants to promote sinus drainage. Local treatment, especially at the onset, includes sinus punctures (if indicated for maxillary or frontal sinusitis) and anemization of the middle nasal meatus mucosa (e.g., 4-5 times daily). In young children, suctioning of contents from the nasal passages is important.
- Intranasal Corticosteroids: To reduce mucosal inflammation.
- Analgesics and Antipyretics.
- Physiotherapeutic methods (e.g., UHF therapy) and general anti-inflammatory therapy may be considered adjunctive.
- Surgical Intervention: Often required, especially for subperiosteal abscess, orbital abscess, severe orbital cellulitis unresponsive to medical therapy, or if vision is threatened.
- Drainage of Abscesses: Subperiosteal and orbital abscesses require prompt surgical drainage. This can often be achieved via an endoscopic transnasal approach (FESS) to drain the infected sinus(es) and decompress the orbit by removing part of the lamina papyracea or orbital floor. External approaches (e.g., Lynch incision for medial orbital abscesses) may be used if endoscopic access is inadequate or for specific locations. Eyelid abscesses are opened with incisions parallel to the palpebral fissure.
- Sinus Surgery: Addressing the infected paranasal sinus(es) is crucial. This usually involves FESS to open and drain the involved sinuses (e.g., ethmoidectomy, maxillary antrostomy, frontal sinusotomy). For frontal sinus involvement, trephination with instillation of antibacterial agents may be performed if FESS is not immediately feasible or sufficient. Resection of hypertrophied or polypoid nasal conchae may be necessary.
- Fistula Management: Fistulas require excision of the tract and adequate treatment of the underlying chronic sinus infection.
The decision to operate and the choice of surgical approach are based on clinical findings, imaging (CT/MRI), and the patient's response to medical therapy. If conservative treatment for acute sinusitis with orbital complications is unsuccessful or symptoms worsen, surgery on the corresponding paranasal sinus is performed. With phlegmon of the orbit, a diagnostic puncture may be performed, and the affected paranasal sinus opened with removal of orbital contents if necessary. If a fistula is found, it may be preferable to access the orbit through it.
In early childhood, if orbital phlegmon occurs, the primary focus is usually the maxillary or ethmoid sinus. The ethmoid sinus is often opened via an external approach in such severe cases, while the maxillary sinus might be approached through the inferior orbital wall. During the period of permanent tooth eruption (ages 6-11 years), radical surgery on the maxillary sinus is generally undesirable to avoid damaging tooth germs; endonasal intervention is preferred. If urgent radical sinusitis surgery is needed at this age, trepanation of the outer sinus wall is performed as high as possible (further from the alveolar ridge and near the edge of the piriform opening). From age 12 onwards, indications for surgical intervention on the maxillary sinus can be broader.
With non-purulent orbital lesions (e.g., reactive edema) and acute sinusitis in children, conservative therapy is primarily carried out. For non-purulent orbital lesions with chronic sinusitis, conservative surgical interventions are necessary, considering age-related sinus development. If a purulent process exists in both the orbit and paranasal sinuses, wide opening of the affected sinuses is performed with simultaneous drainage of the orbital abscess (either through the operated sinus or via an additional orbitotomy), all against a background of massive anti-inflammatory therapy. Endonasal intervention alone may be insufficient in these severe cases. **A decrease in vision is a strict indication for urgent surgical intervention on the affected paranasal sinuses and orbit.**
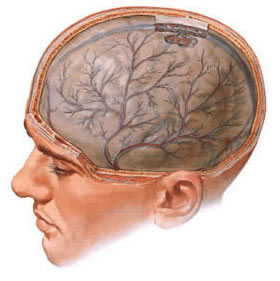
Rhinogenic Intracranial Complications
Overview and Types of Complications
Rhinogenic intracranial complications arise when infection from the paranasal sinuses spreads into the cranial cavity. These are severe, life-threatening conditions. Common types include:
- Secondary Hydrocephalus (often communicating)
- Arachnoiditis
- Serous and Purulent Meningitis
- Meningoencephalitis
- Epidural Abscess
- Subdural Abscess (Empyema)
- Brain Abscess
- Thrombosis of Dural Venous Sinuses (e.g., Cavernous Sinus, Superior Longitudinal Sinus)
Sometimes one form of complication can transition into another, or multiple forms can coexist.
Secondary Hydrocephalus
Can be primary (due to direct inflammation affecting CSF pathways) or secondary (e.g., to meningitis or arachnoiditis). It is characterized by edema of the brain membranes with symptoms of cerebrospinal fluid (CSF) hypertension: increased CSF volume and pressure, often with decreased protein content but unchanged cytosis in non-inflammatory hydrocephalus. Symptoms include headache (often frontal and temporal), nausea, vomiting, visual disturbances, papilledema (congestive nipples of the optic nerves), and potential cranial nerve palsies (abducens, oculomotor, trigeminal, olfactory), epileptiform seizures, or paralysis.
Arachnoiditis
Inflammation of the arachnoid mater (one of the brain's covering membranes). It can be adhesive, cystic, or mixed. Characteristic locations include the anterior cranial fossa, opticochiasmatic region (affecting optic nerves and chiasm), less often the posterior cranial fossa, or the convex surface of the brain, leading to a variety of neurological symptoms.
- Anterior Cranial Fossa Localization: Focal neurological symptoms may be absent; pain in the forehead and bridge of the nose is common.
- Opticochiasmatic Arachnoiditis: Accompanied by impaired visual acuity and visual fields, potentially leading to optic nerve atrophy. Paroxysms, paralysis of oculomotor and (less often) abducens nerves, and pain in the forehead/orbit can occur.
- Basal Arachnoiditis (involving trigeminal nerve): Characterized by pain in one half of the face.
- Posterior Cranial Fossa Arachnoiditis: Typical symptoms include coordination disorders like ataxia and adiadochokinesis.
Rhinogenic arachnoiditis is not always accompanied by CSF changes; moderate pleocytosis (increased cells) and a slight increase in protein are possible.
Serous and Purulent Meningitis
- Serous Meningitis: Characterized by acute onset, mild meningeal symptoms, and increased CSF pressure with clear or slightly turbid CSF, often with lymphocytic pleocytosis.
- Purulent Meningitis: More common than other intracranial complications. Acute onset with high fever, severe headache, nausea, vomiting, and prominent meningeal syndrome (neck stiffness, Kernig's/Brudzinski's signs). High CSF pleocytosis (predominantly neutrophils, thousands of cells/mm³), elevated protein (sometimes 1-3 g/L or more), decreased glucose (10-15 mg% or lower), and decreased chloride (350-450 mg%) are typical. CSF appears purulent and flows out under high pressure. Cranial nerve involvement (commonly VI and VII pairs), psychomotor agitation, delirium, and loss of consciousness can occur. Seizures and positive pathological reflexes (Babinski, Rossolimo, Oppenheim, Gordon) may be present.
Meningoencephalitis
Develops acutely, accompanied by headache, vomiting, meningeal signs, and convulsions. Consciousness is often impaired. The meningeal syndrome is complemented by focal neurological symptoms due to brain parenchyma involvement (encephalitis). Skin and tendon reflexes may change, and pathological reflexes can appear. CSF pressure and cytosis increase.
Epidural Abscess
A collection of pus between the dura mater and the inner table of the skull. Often occurs by direct extension from an infected frontal, ethmoid, or sphenoid sinus. It can be asymptomatic and discovered incidentally during surgery for sinusitis. Symptoms, if present, may include headache, vomiting, difficulty with outward eye movement (abducens nerve palsy), weakened corneal reflex, choking sensation, or nasal voice quality.
Subdural Abscess (Empyema)
A collection of pus in the subdural space (between the dura mater and arachnoid mater). Often appears via hematogenous spread, less commonly by direct contact, especially if an extradural abscess is also present. Characterized by progressively worsening headache unresponsive to medication. Seizures, paresis of the extremities, and (with left-sided localization in right-handed individuals) motor aphasia are possible. CSF shows increased protein and cells.
Brain Abscess
More often localized in the frontal lobe, typically resulting from an exacerbation of chronic purulent frontal sinusitis. Characterized by increased body temperature, headache, vomiting, lack of appetite, and general weakness. Mental status changes (rudeness, buffoonery, ridiculous acts, gluttony, untidiness), impaired statics (balance), appearance of pathological reflexes (grasping, sucking), and decline in intelligence and memory can be noted. If localized in the left frontal lobe (or temporal lobe in right-handers), speech disorders may occur. With an encapsulated abscess, protein-cellular dissociation (high protein, low cells) may appear in the CSF, which flows out under pressure. If a brain abscess is combined with meningitis, symptoms of the latter often prevail. Deterioration of general condition, pulse lagging behind body temperature after meningeal symptoms resolve and CSF normalizes, more often indicate an abscess.
Thrombosis of Dural Venous Sinuses
Thrombosis of the cavernous sinus or superior longitudinal sinus can occur with purulent disease of the paranasal sinuses, facial/nasal trauma (e.g., nasal furuncle). Characterized by a severe general septic condition: high, intermittent fever, chills, headache, weakness, and meningeal symptoms.
- Cavernous Sinus Thrombosis: Manifests with eyelid and conjunctival swelling (chemosis), exophthalmos, and paralysis of eye muscles (ophthalmoplegia due to involvement of CN III, IV, VI).
- Superior Longitudinal Sinus Thrombosis: Rare in children; can cause seizures, focal neurological deficits, and increased intracranial pressure.
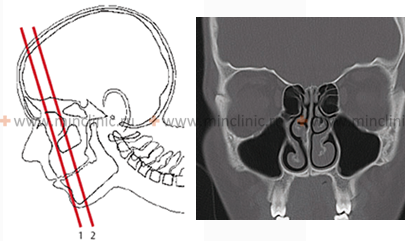
Diagnosis of Rhinogenic Intracranial Complications
Diagnosing these complications requires a high index of suspicion when a patient with sinusitis develops neurological or severe systemic symptoms. Key elements include:
- Identifying Sinus Disease: Evidence of acute or chronic sinusitis on clinical examination or imaging. The masking effect of prior antibiotic use on local nasal and general systemic symptoms must be considered; intracranial complications can sometimes be the first clinical sign of an otherwise asymptomatic sinusitis.
- Lumbar Puncture and CSF Analysis: Crucial for diagnosing meningitis, arachnoiditis, and sometimes providing clues for abscesses (e.g., increased pressure, pleocytosis, altered protein/glucose). CSF hypertension (if causative factor according to lumbar puncture) suggests hydrocephalus.
- Neurological Examination: To detect focal deficits, meningeal signs, cranial nerve palsies, and altered mental status. Arachnoiditis often proceeds without clear neurological symptoms or gross focal phenomena initially.
- Neuroimaging:
- CT Scan of Head and Sinuses (with contrast): Essential for detecting epidural/subdural abscesses, brain abscesses, sinus opacification, bony erosion, and hydrocephalus.
- MRI of the Brain (with contrast, including venography - MRV): Superior for evaluating brain parenchyma, meningitis, encephalitis, subdural empyema, brain abscesses, and dural venous sinus thrombosis.
- Other Neurodiagnostic Studies (less common now with advanced imaging): Pneumoencephalography, electroencephalography (EEG), angiography were historically used.
Differentiating conditions: Purulent meningitis typically has an acute onset with cerebral meningeal symptoms, high fever, and sinusitis signs, with high CSF pleocytosis. It must be distinguished from brain abscess and secondary meningitis. If, during CSF normalization, the patient's health remains poor or worsens (indifference, drowsiness), this is more characteristic of a brain abscess. Meningoencephalitis combines meningeal and focal symptoms. It is vital, though difficult, to distinguish it from a brain abscess as management differs. Brain abscess often has a subacute onset with gradually increasing neurological symptoms and mental changes (apathy, lethargy), whereas high fever, meningeal signs, agitation, and convulsions are atypical for the initial phase of an abscess. Extradural and subdural abscesses can be hard to recognize due to subtle focal neurological signs. Brain abscess diagnosis relies on detecting mental changes (frontal lobe) and focal symptoms (gaze palsy opposite the lesion, statokinetic disorders, grasping/resistance phenomena, eyelid closure issues; temporal lobe abscess may cause ataxia and impaired contralateral tests; left temporal lobe lesions can cause amnestic/sensory aphasia). Thrombophlebitis is characterized by a septic state combined with circulatory and neurological syndromes.
Diagnostic procedure: Magnetic Resonance Imaging (MRI) of the brain is crucial for detecting and characterizing intracranial complications of sinusitis.
Treatment of Rhinogenic Intracranial Complications
Management is complex and requires a multidisciplinary team (ENT, neurosurgery, infectious diseases, neurology, critical care). Treatment depends on the nature of the sinusitis, the specific complication, and the child's age and overall condition. The core principle is to address the primary focus of infection in the paranasal sinuses while simultaneously managing the intracranial complication.
- Aggressive Antibiotic Therapy: High-dose, broad-spectrum intravenous antibiotics that penetrate the blood-brain barrier are initiated immediately. Therapy is then tailored based on culture results from sinuses or intracranial collections. Prolonged courses are usually required.
- Surgical Drainage of Infected Sinuses: Emergency surgical drainage of the affected paranasal sinus(es) (usually FESS) is often indicated to eliminate the source of infection. This is critical.
- Neurosurgical Intervention:
- Epidural or Subdural Abscess/Empyema: Requires surgical drainage, often via craniotomy or burr holes. If an extradural abscess is found during sinus surgery (often with frontitis), and the posterior wall of the frontal sinus is changed or has a fistula, wide resection of this wall is necessary. Even suspected intracranial complications justify proactive surgical exploration. Osteomyelitic areas of the frontal bone are removed.
- Brain Abscess: May require stereotactic aspiration or surgical excision, depending on size, location, and encapsulation. Often, the affected paranasal sinus is widely opened first. With frontal sinusitis, trephination with removal of the posterior sinus wall is performed for decompression, and an anterior cranial fossa abscess is drained. When exposing the dura, its color, pulsation, thickness, and presence of granulations or fibrinous plaque are noted. Before puncturing the brain, a small dural incision may be made. A special blunt-ended needle is inserted into the brain (approx. 3 cm depth). The abscess is drained using rubber strips or catheters left in the cavity until discharge ceases.
- Management of Increased Intracranial Pressure: Measures such as osmotic diuretics (mannitol), hypertonic saline, corticosteroids (use in brain abscess is controversial but may be used for edema), and CSF diversion (e.g., ventricular drain) may be needed.
- Anticonvulsant Therapy: If seizures occur.
- Supportive Care: Including hydration, nutrition, and management of systemic complications.
For non-suppurative intracranial complications (hydrocephalus, arachnoiditis, serous meningitis) caused by acute sinusitis, conservative treatment is initially attempted. If there is no improvement within 2-3 days or if symptoms worsen, surgery on the paranasal sinuses is performed. If these non-suppurative complications are associated with chronic sinus inflammation, a sanitizing operation on the sinus is performed. For purulent intracranial complications, emergency surgery on the affected sinuses is indicated alongside massive antibacterial, dehydration, desensitizing, and general supportive therapy.
Differential Diagnosis of Orbital and Intracranial Symptoms
When a patient presents with symptoms suggestive of orbital or intracranial complications in the context of known or suspected sinusitis, it's important to consider the spectrum of possibilities:
| Presenting Symptom Complex | Rhinogenic Complication to Suspect | Other Differentials |
|---|---|---|
| Eyelid swelling, redness, proptosis, painful/restricted eye movements, +/- vision changes, fever | Orbital cellulitis, Subperiosteal abscess, Orbital abscess, Cavernous sinus thrombosis (if bilateral or CN palsies) | Primary orbital tumor, orbital pseudotumor (inflammatory), thyroid eye disease, dacryoadenitis, trauma |
| Severe headache, fever, neck stiffness, photophobia, altered mental status | Meningitis (bacterial/serous), Meningoencephalitis | Viral encephalitis, primary bacterial meningitis (non-rhinogenic), subarachnoid hemorrhage, brain tumor |
| Headache, fever, focal neurological deficits (weakness, speech problems, seizures) | Brain abscess, Subdural empyema, Epidural abscess, Dural venous sinus thrombosis with venous infarct | Stroke, brain tumor, viral encephalitis with focal signs, primary epilepsy |
| Progressive headache, nausea/vomiting, papilledema, vision changes, +/- cranial nerve palsies | Secondary hydrocephalus, Opticochiasmatic arachnoiditis (if visual field defects prominent) | Primary hydrocephalus, intracranial tumor causing obstruction, pseudotumor cerebri (idiopathic intracranial hypertension) |
Prevention and When to Seek Urgent Multidisciplinary Care
Prevention hinges on early and effective treatment of acute and chronic rhinosinusitis:
- Prompt medical attention for persistent or severe sinus symptoms.
- Adequate courses of antibiotics for bacterial sinusitis when indicated.
- Management of underlying predisposing factors like allergies or anatomical obstructions.
- Close monitoring of patients with sinusitis, especially children and immunocompromised individuals.
Immediate, urgent multidisciplinary consultation (ENT, ophthalmology, neurosurgery, infectious diseases, radiology) and hospital admission are imperative if any signs or symptoms suggestive of orbital or intracranial complications arise in a patient with sinusitis. These include:
- Proptosis (bulging eye)
- Ophthalmoplegia (restricted or painful eye movements)
- Decreased vision
- Severe, persistent headache unresponsive to analgesics
- Neck stiffness
- Photophobia
- Altered mental status (confusion, lethargy, irritability)
- Seizures
- Focal neurological deficits
- Persistent high fever despite antibiotic treatment for sinusitis
Rapid diagnosis and aggressive, coordinated treatment are critical to minimize morbidity and mortality associated with these severe complications.
References
- Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970 Sep;80(9):1414-28.
- Wald ER, Pang D, Milmoe GJ, Schramm VL Jr. Sinusitis and its complications in the pediatric patient. Pediatr Clin North Am. 1981 Nov;28(4):777-96.
- Jones NS, Walker JL, Bassi S, et al. The intracranial complications of rhinosinusitis: can they be prevented? Laryngoscope. 2002 Aug;112(8 Pt 1):1373-7.
- Clayman GL, Adams GL, Paugh DR, Koopmann CF Jr. Intracranial complications of paranasal sinusitis: a review of 137 cases. Ann Otol Rhinol Laryngol. 1991 Jun;100(6):491-6.
- Younis RT, Lazar RH, Anand VK. Intracranial complications of sinusitis: a surgeon's perspective. Laryngoscope. 2002 Jul;112(7 Pt 1):1150-7.
- Bedwell J, Kşnig H, Cho G, et al. Management of orbital complications of rhinosinusitis: A consensus statement. Int J Pediatr Otorhinolaryngol. 2021 Aug;147:110797.
- Germiller JA, Monin DL, Sparano AM, Tom LWC. Intracranial complications of sinusitis in children and adolescents and their outcomes. Arch Otolaryngol Head Neck Surg. 2006 Sep;132(9):969-76.
- Stokroos RJ, Manni JJ, de Vries N. Subdural empyema complicating sinusitis. Rhinology. 1998 Dec;36(4):193-6.
See also
Nasal cavity diseases:
- Runny nose, acute rhinitis, rhinopharyngitis
- Allergic rhinitis and sinusitis, vasomotor rhinitis
- Chlamydial and Trichomonas rhinitis
- Chronic rhinitis: catarrhal, hypertrophic, atrophic
- Deviated nasal septum (DNS) and nasal bones deformation
- Nosebleeds (Epistaxis)
- External nose diseases: furunculosis, eczema, sycosis, erysipelas, frostbite
- Gonococcal rhinitis
- Changes of the nasal mucosa in influenza, diphtheria, measles and scarlet fever
- Nasal foreign bodies (NFBs)
- Nasal septal cartilage perichondritis
- Nasal septal hematoma, nasal septal abscess
- Nose injuries
- Ozena (atrophic rhinitis)
- Post-traumatic nasal cavity synechiae and choanal atresia
- Nasal scabs removing
- Rhinitis-like conditions (runny nose) in adolescents and adults
- Rhinogenous neuroses in adolescents and adults
- Smell (olfaction) disorders
- Subatrophic, trophic rhinitis and related pathologies
- Nasal breathing and olfaction (sense of smell) disorders in young children
Paranasal sinuses diseases:
- Acute and chronic frontal sinusitis (frontitis)
- Acute and chronic sphenoid sinusitis (sphenoiditis)
- Acute ethmoiditis (ethmoid sinus inflammation)
- Acute maxillary sinusitis (rhinosinusitis)
- Chronic ethmoid sinusitis (ethmoiditis)
- Chronic maxillary sinusitis (rhinosinusitis)
- Infantile maxillary sinus osteomyelitis
- Nasal polyps
- Paranasal sinuses traumatic injuries
- Rhinogenic orbital and intracranial complications
- Tumors of the nose and paranasal sinuses, sarcoidosis