Nasal breathing and olfaction (sense of smell) disorders in young children
- Understanding Nasal Breathing and Olfaction Disorders in Young Children
- Clinical Presentation of Nasal Breathing and Olfaction Disorders
- Diagnosis of Nasal Breathing and Olfaction Disorders
- Treatment Approaches for Nasal Breathing and Olfaction Disorders
- Potential Complications of Chronic Nasal Obstruction
- Differential Diagnosis of Nasal Obstruction in Young Children
- When to Consult an ENT Specialist
- References
Understanding Nasal Breathing and Olfaction (Sense of Smell) Disorders in Young Children
Disorders of nasal breathing and olfaction (the sense of smell) in young children are primarily caused by obstruction of the nasal cavity or nasopharynx. Impaired nasal breathing in infants and children during their first years of life can stem from either congenital (present at birth) or acquired causes. Normal nasal breathing is crucial for proper respiratory function, feeding, sleep, facial development, and the development of the sense of smell.
Etiology and Pathogenesis
The underlying cause of these disorders is typically a physical blockage or significant narrowing of the nasal passages or the nasopharynx (the area behind the nose and above the soft palate).
Congenital vs. Acquired Obstructions
- Congenital Obstruction:
- Choanal Atresia: This is a blockage of the posterior nasal apertures (choanae) that connect the nasal cavity to the nasopharynx. It can be complete (no opening) or incomplete (narrowing/stenosis), unilateral or bilateral. Bilateral complete choanal atresia is a neonatal emergency as newborns are obligate nasal breathers.
- Nasal Cavity Atresia: Congenital blockage within the nasal cavity itself.
- Malformations or Hypoplasia of the Nasopharynx: Underdevelopment or abnormal formation of the nasopharyngeal space.
- Other Craniofacial Anomalies: Conditions like pyriform aperture stenosis or midface hypoplasia.
- Acquired Obstruction:
- Inflammatory Conditions:
- Rhinitis/Nasopharyngitis: Acute or chronic inflammation of the nasal and nasopharyngeal mucosa due to viral, bacterial, or allergic causes leads to mucosal edema and increased secretions (e.g., acute rhinitis, allergic rhinitis).
- Sinusitis: Inflammation of the paranasal sinuses can cause nasal discharge and swelling that obstructs nasal passages.
- Adenoid Vegetations (Hypertrophied Adenoids): Enlargement of the adenoid tissue in the nasopharynx is a very common cause of nasal obstruction and mouth breathing in young children.
- Granulomatous Diseases: Chronic inflammatory conditions like tuberculosis, syphilis, or rhinoscleroma can cause destructive lesions and obstruction (rare in many regions now).
- Diphtheria: Can cause pseudomembranes that obstruct the nasal passages.
- Structural Issues:
- Foreign Bodies: Objects inserted into the nose by children.
- Tumors/Masses: Benign (e.g., nasal polyps, encephaloceles, dermoids) or malignant neoplasms (rare in young children).
- Nasal Septal Hematoma or Abscess: Typically follows trauma.
- Deviated Nasal Septum: Can be congenital or acquired from trauma.
- Hypertrophy of the Turbinates: Chronic enlargement of the nasal conchae.
- Trauma: Nasal trauma leading to fractures, septal deviation, or hematoma.
- Iatrogenic Causes: Complications from previous nasal surgery, such as unqualified adenotomy leading to scarring or stenosis.
- Retropharyngeal Abscess: An infection in the space behind the pharynx can bulge forward and obstruct the nasopharynx.
- Inflammatory Conditions:
Impact of Vasoconstrictor Overuse and Systemic Conditions
Changes in the nasal mucous membrane due to excessive or prolonged local application of vasoconstrictor nasal drops (e.g., decongestants) in infants can paradoxically cause severe nasal obstruction, difficulty in nasal breathing, and discomfort. When used unnecessarily or for too long, vasoconstrictors can lead to a rebound effect (rhinitis medicamentosa), characterized by vasodilation of the nasal blood vessels and an increase in mucosal edema. The mucous membrane becomes even more inflamed and thickened, manifesting as swelling of the nasal conchae and increased secretion.
Among other less common reasons for nasal breathing difficulty and discharge, hyperthyroidism has been noted to cause changes in mucous gland function, leading to secretions that are thicker than usual. However, rhinoscopy in such cases often reveals only edematous mucosa. Even if nasal secretions are not prominent during examination and the middle nasal passages appear normal, if hypothyroidism (or hyperthyroidism) is suspected based on other systemic signs, thyroid gland function should be investigated.
Clinical Presentation of Nasal Breathing and Olfaction Disorders in Young Children
Prolonged obstruction of the nasal cavity in newborns and infants significantly impacts their well-being and development:
- Feeding Difficulties: Sucking is disturbed as infants are obligate nasal breathers. They may become irritable during feeding, frequently detach from the breast or bottle to gasp for air, leading to underfeeding, poor weight gain, and failure to thrive.
- Sleep Disturbances: The child is often capricious when being put to bed, snores during sleep, and sleeps with an open mouth. Apneic episodes or choking may occur.
- Mouth Breathing: Persistent mouth breathing can lead to dry mouth, chapped lips, and in the long term, may contribute to abnormal facial development (e.g., "adenoid facies" with an elongated face, high arched palate) and dental malocclusion.
- Nasal Discharge: If the obstruction is combined with infection or inflammation, purulent nasal discharge is common and may intensify as the obstruction progresses.
- Impaired Sense of Smell (Hyposmia/Anosmia): While difficult to assess formally in very young children, parents might notice a lack of reaction to strong odors or a disinterest in food if olfaction is significantly impaired. This can also affect taste perception and appetite.
- Voice Changes: A hyponasal (denasal) voice quality may be present due to lack of nasal resonance.
- Restlessness and Irritability: Due to discomfort and difficulty breathing.
On examination of the nasal cavity, anatomical constriction of varying nature (depending on the underlying cause) or edematous, inflamed tissue is typically observed.
Diagnosis of Nasal Breathing and Olfaction Disorders in Young Children
Diagnosing the cause of nasal breathing and olfaction disorders in young children requires a careful history, thorough physical examination, and often specific diagnostic tests.
Diagnosing Choanal Atresia
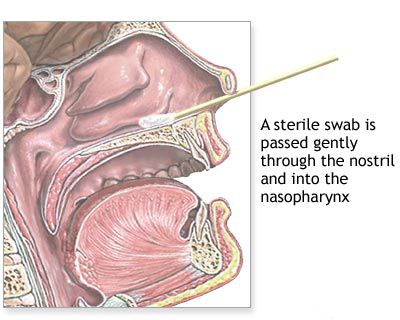
Complete bilateral choanal atresia is usually identified at birth or within the first few hours of life. It presents with severe asphyxia (difficulty breathing, cyanosis) when the newborn, who is an obligate nasal breather, attempts to breathe with the mouth closed (e.g., during feeding). Inspiratory dyspnea is prominent. The diagnosis is confirmed by the inability to pass a small (e.g., 5-6 Fr) flexible catheter through each nostril into the nasopharynx. Instilling a small amount of methylene blue dye into the nose: normally, it should be visible in the oropharynx; this will not occur if there's a complete blockage. Flexible nasal endoscopy provides direct visualization of the atretic plate. A CT scan can confirm the diagnosis and delineate whether the atresia is bony, membranous, or mixed.
Unilateral choanal atresia may not always be diagnosed in the newborn period, as the infant can breathe through the patent nostril. Symptoms may be minimal, such as persistent unilateral nasal discharge or obstruction. Asphyxia attacks might only occur during feeding when the patent nostril is occluded. Stagnant secretions in the obstructed nasal cavity can lead to recurrent rhinitis, sinusitis, and potentially exudative otitis media on that side.
Congenital nasal defects like choanal atresia or intranasal synechiae (connective tissue, cartilaginous, or bony bridges between nasal walls that partially or completely occlude nasal passages) are often associated with other craniofacial anomalies like cleft palate or cleft lip. X-ray examination with contrast material instilled into the nose can help establish the localization of the constriction, but CT is more definitive.
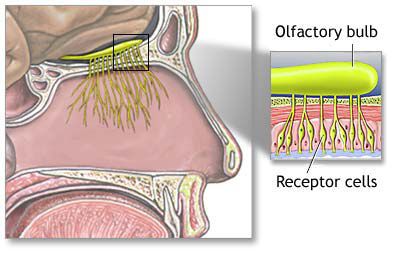
Assessing Olfactory Disorders
Disorders of the sense of smell (hyposmia or anosmia) are common with hereditary or acquired forms of deviated nasal septum. The superior part of the nasal septum, from the level of the middle nasal concha upwards, constitutes the olfactory region. It is important to note that not only the olfactory nerve (cranial nerve I) but also other nerves innervating the nasal septum (e.g., branches of the trigeminal nerve, autonomic nerves) participate in the perception of odors (e.g., trigeminal sensations from irritants). Therefore, any injury or significant deviation of the nasal septum, especially in its olfactory region, can lead to olfactory dysfunction.
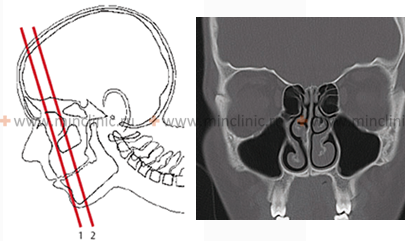
The cause of smell disorders is often a high septal deviation, particularly if it makes contact with the middle turbinate, obstructing the olfactory cleft. Minor deviations in the posterior septum or the presence of small crests or spurs lower down do not usually lead to significant smell disturbance, as they do not typically impede airflow to the olfactory epithelium. With a high septal deviation, the inspiratory air current may be forcibly directed along the lower nasal passage instead of arching upwards towards the olfactory region as it normally would. In some cases, the middle turbinate and the deviated septum may be in close contact, completely blocking the olfactory cleft and causing hyposmia or anosmia on the side of the narrowed nasal passage. Occasionally, smell can be disturbed on both sides or paradoxically on the side opposite the main deviation due to compensatory hypertrophy of the contralateral nasal concha. Olfactory disorders can also result from direct narrowing of the nasal cavity by the deviation or from secondary inflammatory changes within the nasal cavity. The cause is established by careful nasal examination (including endoscopy) and sometimes specific olfactory testing (though challenging in very young children).
Investigating Other Causes of Obstruction
- Nasal Trauma and Septal Hematoma/Abscess: Fracture of the nasal bones in infants may be confirmed by crepitus (a crackling sound or sensation) on palpation. Nasal trauma is usually accompanied by swelling and hemorrhage into the nasal mucosa. Radiographic evidence of a nasal fracture is not always definitive in infants, as it can be difficult to differentiate simple trauma from a fracture. A septal hematoma can occur during childbirth or, more commonly, from falls in young children when the nasal structures are not yet fully hardened. It results from sharp injury separating the perichondrium from the cartilage. Rhinoscopy reveals a bilateral (or sometimes unilateral) bluish-red swelling of the anterior septum, which is soft and compressible on probing. Aspiration of its contents with a thick needle may confirm the presence of blood (or pus if it has become an abscess). Anemization has little effect on the obstruction caused by a hematoma or abscess.
- Deviated Nasal Septum (Post-Traumatic or Developmental): Can result from birth trauma (passage through a narrow birth canal) or later injury. Rhinoscopy may reveal various displacements of the septum, often with thickening at its base due to maxillary crest involvement or cartilage displacement. Compensatory hypertrophy of the contralateral turbinate can further contribute to obstruction. Anamnestic data, including details of birth (pelvic size, neonatal nosebleeds, external nasal deformity, soft tissue swelling), are important. Dislocation or fracture of the cartilaginous septum is often visible. Anemization of the mucosa helps in visualizing the posterior nasal cavity.
- Nasal Foreign Body: In young children, this is characterized by unilateral nasal obstruction, unilateral mucous or mucopurulent (often foul-smelling) discharge, and recurrent nosebleeds. After anemization, rhinoscopy often reveals the foreign body, typically near the anterior end of the inferior turbinate. Radiopaque foreign bodies can be identified by X-ray. Removal attempts in infants may require general anesthesia.
- Adenoid Vegetations: Can develop in early childhood, leading to characteristic facial changes (adenoid facies: long face, half-open mouth, drooping lower jaw, flattened nasolabial folds). In infants, digital examination of the nasopharynx (performed by a physician) can help confirm the diagnosis. Lateral neck X-ray or nasal endoscopy are preferred methods.
- Sinusitis: In young children, sinusitis may not always manifest with obvious purulent nasal discharge. Chronic sinusitis (possible even by age 2) can cause hyperemia and swelling of the nasal mucosa, with mucopurulent discharge sometimes visible in the middle meatus.
- Retropharyngeal Abscess: Presents with nasal breathing disturbances, dysphagia (difficulty swallowing), and a nasal voice quality. Examination shows bulging of the posterior pharyngeal wall, which is soft to the touch.
- Rhinoscleroma: Rare in infants; characterized by narrowing of the nasal vestibule due to hard, protruding infiltrates in the nasal wings. Infiltrates can also be found in the nasopharyngeal arch and choanae. Diagnosis may involve serological tests (e.g., Bordet-Gengou reaction with scleral antigen) and biopsy.
- Allergy: Allergic rhinitis can cause significant nasal obstruction in young children but can be difficult to diagnose definitively without comprehensive allergological studies, which are challenging at an early age. Symptoms (sneezing attacks, profuse clear rhinorrhea, nasal itching, swollen, cyanotic inferior turbinates that don't shrink much with anemization) can mimic other conditions. A careful history is crucial to identify seasonal or episodic patterns. Allergic diseases can also reduce resistance to bacterial infections, leading to secondary bacterial rhinitis. Cytological examination of nasal secretions (for eosinophils) can be helpful.
- Vasomotor Rhinitis: Characterized by nasal hyperreactivity with vasodilation, hyperemia, hypersecretion, and mucosal hypertrophy, apparently of reflex origin. The etiology is often unknown, but stress and weather changes can exacerbate symptoms. The nasal mucosa may appear pale or hyperemic, with transparent watery discharge. Obstruction and rhinorrhea can occur together or separately.
For differential diagnosis, microbiological cultures (for bacteria, fungi), serological testing (e.g., for syphilis), and skin testing (e.g., for tuberculosis) may be performed as indicated. Careful interpretation of anamnestic data, thorough examination, and appropriate additional diagnostic studies are essential for an accurate diagnosis.
Treatment Approaches for Nasal Breathing and Olfaction Disorders in Young Children
Therapy for nasal breathing disturbances in young children must be directed at eliminating the underlying cause of the nasal cavity obstruction or addressing the specific pathology. It is generally inappropriate to use decongestant or anti-congestive agents, aerosols, or other medications empirically before a definitive diagnosis is established, as this can mask symptoms or lead to adverse effects like rhinitis medicamentosa.
- Emergency Airway Management: In cases of bilateral choanal atresia or other conditions causing severe asphyxia at birth, immediate measures are taken to ensure breathing through the mouth. This may involve positioning the child (e.g., gluing the chin to the chest with adhesive tape to keep the mouth open – a historical technique now replaced by more modern airway adjuncts) or inserting an oral airway.
- Management of Secretions: Accumulated nasal mucus due to rhinitis, sinusitis, or other pathologies should be removed by gentle aspiration, especially in infants before feeding.
- Treatment of Infections: Acute inflammatory diseases of the nose and paranasal sinuses, or exacerbations of chronic processes, often require antibacterial therapy (if bacterial) and general supportive treatment (hydration, antipyretics).
- Surgical Intervention: Surgical intervention in young children is generally limited and performed only for clear indications due to ongoing facial growth and development. However, procedures such as:
- Adenoidectomy (for hypertrophied adenoids).
- Polypectomy (for nasal polyps).
- Drainage of septal hematoma/abscess.
- Repair of choanal atresia.
- Removal of foreign bodies.
- Sinus puncture or lavage (less common now, often replaced by endoscopic approaches if surgery is needed).
- Management of Allergic/Vasomotor Rhinitis: If diagnosed, involves allergen avoidance, antihistamines, intranasal corticosteroids, or other appropriate medical therapies.
- Correction of Structural Deformities: Procedures like septoplasty for a deviated septum are usually deferred until facial growth is more complete (adolescence), unless the obstruction is exceptionally severe and causing significant complications.
Potential Complications of Chronic Nasal Obstruction in Young Children
Prolonged and significant obstruction of the nasal cavity in young children can lead to several important complications:
Hearing Impairment and Middle Ear Issues
One of the most common complications is hearing impairment resulting from **exudative otitis media (otitis media with effusion - OME)**, also known as "glue ear." Chronic nasal obstruction and inflammation (e.g., from adenoid hypertrophy or chronic rhinitis) can lead to Eustachian tube dysfunction. The Eustachian tube, which connects the middle ear to the nasopharynx, may become blocked, preventing proper ventilation and drainage of the middle ear. This results in the accumulation of sterile fluid in the middle ear space, causing conductive hearing loss.
Diagnosis of OME in children involves:
- Otoscopy: Examination of the tympanic membrane (eardrum) may reveal it to be dull, retracted, bulging, opaque, or amber-colored. Air bubbles or an air-fluid level may be visible behind the eardrum.
- Tympanometry: This objective test measures the compliance (mobility) of the tympanic membrane and middle ear pressure. In OME, the tympanogram is often flat (Type B), indicating fluid in the middle ear and poor eardrum mobility with both positive and negative applied pressure.
- Audiometry: Age-appropriate hearing tests (e.g., play audiometry, visual reinforcement audiometry, otoacoustic emissions) often indicate a conductive hearing loss, while bone conduction remains normal.
- Tuning Fork Tests (less commonly used in very young children but historically relevant):
- Weber's Test: Performed by placing a vibrating tuning fork on the midline of the skull or maxillary incisors. In conductive hearing loss, the sound lateralizes to the affected (more poorly hearing) ear.
- Rinne Test: Compares air conduction (AC) and bone conduction (BC). Normally, AC is better than BC (positive Rinne). In conductive hearing loss, BC is better than or equal to AC (negative Rinne).
Forceful nose blowing, covering the nose and mouth while inflating the cheeks, can potentially force air and secretions up the Eustachian tube, increasing the risk of middle ear infection if nasal secretions are infected.
Sinusitis
Another frequent complication of long-term nasal obstruction is **sinusitis**. Impaired nasal airflow and drainage create a stagnant environment within the paranasal sinuses, predisposing them to infection and inflammation. This is characterized by purulent nasal discharge, especially noticeable in the morning. While adults with sinusitis often report prominent symptoms like facial pain, chills, and headache, these may be less specific or harder for young children to articulate. In children, persistent rhinorrhea, chronic cough (especially at night due to post-nasal drip), and recurrent or persistent otitis media can be important indicators of underlying sinusitis. Common microbial culprits include *Streptococcus pneumoniae*, *Haemophilus influenzae*, and *Moraxella catarrhalis*.
Diagnostic aids for sinusitis in children include:
- Nasal Endoscopy: Can reveal purulent discharge from the sinus ostia, mucosal edema, or polyps.
- Imaging:
- X-ray Examination: May show mucosal thickening, diffuse opacification of the sinuses, or sometimes an air-fluid level. However, diaphanoscopy (transillumination of sinuses) is generally ineffective in children under 12 years due to the underdevelopment of their maxillary and ethmoid sinuses, which are most often involved.
- CT Scan: More definitive for assessing the extent of sinus disease, especially in chronic or complicated cases.
Other potential long-term consequences of chronic nasal obstruction include effects on facial growth, dental development, sleep quality (leading to daytime fatigue and behavioral issues), and overall quality of life.
Differential Diagnosis of Nasal Obstruction in Young Children
A broad differential diagnosis is essential when evaluating a young child with nasal obstruction:
| Condition | Key Differentiating Features |
|---|---|
| Adenoid Hypertrophy | Mouth breathing, snoring, hyponasal voice, recurrent otitis media; confirmed by endoscopy or lateral neck X-ray. |
| Choanal Atresia/Stenosis | Neonatal respiratory distress (if bilateral), persistent unilateral obstruction/discharge; confirmed by inability to pass catheter, endoscopy, CT. |
| Allergic Rhinitis | Nasal itching, sneezing, watery rhinorrhea, pale/boggy turbinates; often family history of atopy; positive allergy tests. |
| Infectious Rhinitis (Viral/Bacterial) | Acute onset, fever, mucopurulent discharge, inflamed mucosa. |
| Nasal Foreign Body | Unilateral, foul-smelling purulent discharge, epistaxis; object often visible on examination. |
| Deviated Nasal Septum | Congenital or traumatic; fixed obstruction; visible on rhinoscopy. |
| Turbinate Hypertrophy | Enlarged inferior or middle turbinates; can be allergic, vasomotor, or compensatory. |
| Nasal Polyps | Pale, grape-like masses; associated with chronic inflammation (e.g., cystic fibrosis, severe allergy). |
| Nasal Tumors (e.g., Encephalocele, Dermoid, Rhabdomyosarcoma) | Rare; progressive unilateral obstruction, epistaxis, facial deformity; requires imaging and biopsy. |
| Septal Hematoma/Abscess | History of trauma; bilateral fluctuant septal swelling, severe pain. |
When to Consult an ENT Specialist
Parents should seek consultation with an Ear, Nose, and Throat (ENT) specialist for their child if:
- Nasal obstruction is persistent, severe, or significantly impacting feeding, sleep, or daily activities.
- There is chronic mouth breathing or snoring.
- Recurrent ear infections or persistent middle ear fluid (OME) are present.
- Recurrent or chronic sinusitis is suspected.
- Unilateral nasal symptoms (obstruction, discharge, bleeding) are present.
- A nasal foreign body is suspected.
- There are concerns about the child's sense of smell.
- Congenital nasal anomalies like choanal atresia are suspected.
- Symptoms do not improve with primary care management.
An ENT specialist can perform a comprehensive evaluation, including nasal endoscopy and other necessary investigations, to determine the exact cause of the nasal breathing or olfaction disorder and recommend the most appropriate and timely management plan.
References
- Mancuso RF. Stridor in neonates. Pediatr Clin North Am. 1996 Aug;43(4):825-32. (Context for congenital airway issues)
- Bluestone CD, Klein JO. Otitis Media in Infants and Children. 4th ed. PMPH USA; 2007. (Relation to nasal obstruction)
- Mygind N. Nasal Allergy. 2nd ed. Blackwell Scientific Publications; 1979. (General rhinitis context)
- Friedman EM, McGill TJI, Healy GB. Nasal obstruction in children. In: Bluestone CD, Stool SE, Alper CM, et al, eds. Pediatric Otolaryngology. 5th ed. PMPH USA; 2013: Chap 60.
- Kashima HK, Kirtane MV, Pletcher SD. Choanal atresia. In: Flint PW, Haughey BH, Lund VJ, et al, eds. Cummings Otolaryngology: Head & Neck Surgery. 6th ed. Elsevier Saunders; 2015: Chap 185.
- Doty RL. The olfactory system. In: Kandel ER, Schwartz JH, Jessell TM, Siegelbaum SA, Hudspeth AJ, eds. Principles of Neural Science. 5th ed. McGraw-Hill; 2013: Chap 32.
- Scadding GK. Paediatric rhinitis. Pediatr Allergy Immunol. 2001 Jun;12(3):163-9.
- Valera FCP, Anselmo-Lima WT. Evaluation of the efficacy of topical corticosteroids for the treatment of idiopathic rhinitis in children. Am J Rhinol Allergy. 2011;25(1):e1-e4.
See also
Nasal cavity diseases:
- Runny nose, acute rhinitis, rhinopharyngitis
- Allergic rhinitis and sinusitis, vasomotor rhinitis
- Chlamydial and Trichomonas rhinitis
- Chronic rhinitis: catarrhal, hypertrophic, atrophic
- Deviated nasal septum (DNS) and nasal bones deformation
- Nosebleeds (Epistaxis)
- External nose diseases: furunculosis, eczema, sycosis, erysipelas, frostbite
- Gonococcal rhinitis
- Changes of the nasal mucosa in influenza, diphtheria, measles and scarlet fever
- Nasal foreign bodies (NFBs)
- Nasal septal cartilage perichondritis
- Nasal septal hematoma, nasal septal abscess
- Nose injuries
- Ozena (atrophic rhinitis)
- Post-traumatic nasal cavity synechiae and choanal atresia
- Nasal scabs removing
- Rhinitis-like conditions (runny nose) in adolescents and adults
- Rhinogenous neuroses in adolescents and adults
- Smell (olfaction) disorders
- Subatrophic, trophic rhinitis and related pathologies
- Nasal breathing and olfaction (sense of smell) disorders in young children
Paranasal sinuses diseases:
- Acute and chronic frontal sinusitis (frontitis)
- Acute and chronic sphenoid sinusitis (sphenoiditis)
- Acute ethmoiditis (ethmoid sinus inflammation)
- Acute maxillary sinusitis (rhinosinusitis)
- Chronic ethmoid sinusitis (ethmoiditis)
- Chronic maxillary sinusitis (rhinosinusitis)
- Infantile maxillary sinus osteomyelitis
- Nasal polyps
- Paranasal sinuses traumatic injuries
- Rhinogenic orbital and intracranial complications
- Tumors of the nose and paranasal sinuses, sarcoidosis