Chronic ethmoid sinusitis (ethmoiditis)
- Understanding Chronic Ethmoid Sinusitis (Ethmoiditis)
- Symptoms of Chronic Ethmoid Sinusitis
- Diagnosis of Chronic Ethmoid Sinusitis
- Treatment Approaches for Chronic Ethmoid Sinusitis
- Differential Diagnosis of Mid-Facial Pain/Pressure and Nasal Discharge
- Potential Complications
- When to Consult an ENT Specialist
- References
Understanding Chronic Ethmoid Sinusitis (Ethmoiditis)
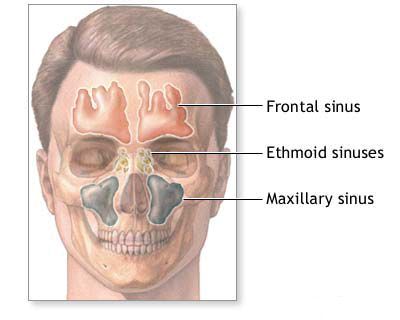
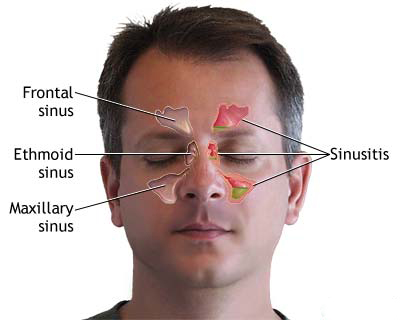
Chronic ethmoid sinusitis, also known as chronic ethmoiditis, is a persistent inflammation of the mucosal lining of the ethmoid sinuses lasting for 12 weeks or longer. The ethmoid sinuses are a complex group of numerous small, air-filled cells located between the eyes and at the base of the nose, forming part of the paranasal sinus system. Due to their intricate anatomy and proximity to other sinuses and critical structures, ethmoiditis often coexists with inflammation in other sinuses.
Etiology and Pathophysiology
The development of chronic ethmoid sinusitis is often multifactorial. Key contributing factors include:
- Recurrent or Inadequately Treated Acute Infections: Unresolved acute sinus infections can transition into a chronic inflammatory state.
- Impaired Nasal Breathing and Sinus Drainage: Conditions that obstruct nasal airflow or the narrow drainage pathways of the ethmoid cells, such as:
- Adenoid hypertrophy (enlarged adenoids), especially in children.
- Deviated nasal septum.
- Nasal polyps.
- Hypertrophied turbinates.
- Anatomical variations in the ostiomeatal complex (the common drainage area for frontal, maxillary, and anterior ethmoid sinuses).
- Altered Immune Reactivity: Underlying immune system dysregulation or deficiencies can predispose individuals to chronic infections. Allergies also play a significant role by causing chronic mucosal inflammation and swelling.
- Microbial Flora Changes: While acute ethmoiditis often involves a single pathogenic organism (monopathogenic flora), chronic ethmoiditis typically features a mixed polymicrobial flora. This can include common respiratory bacteria like Staphylococci, Streptococci, and Pneumococci, often in combination with various saprophytic organisms (normal commensals that can become pathogenic under certain conditions) and sometimes anaerobic bacteria or fungi. Bacterial biofilms, which are structured communities of bacteria resistant to antibiotics and host defenses, are increasingly recognized as playing a key role in the persistence of chronic rhinosinusitis.
Chronic ethmoiditis in children can sometimes present with subtle or nearly asymptomatic courses, making it challenging to recognize. It is almost invariably associated with inflammation in other paranasal sinuses (e.g., maxillary, frontal) and can be unilateral or bilateral. The inflammation typically manifests as an edematous-catarrhal type (swelling with mucus production), and less commonly, as a frankly purulent (pus-forming) process. A characteristic feature of chronic ethmoiditis, particularly when associated with allergy or certain inflammatory conditions, is the development of nasal polyps originating from the ethmoid sinus mucosa.
Pathological Changes
Histopathological examination of tissue from chronic ethmoiditis reveals several characteristic changes:
- Mucosal Edema and Thickening: The lining of the ethmoid cells becomes swollen and thickened.
- Epithelial Metaplasia: The normal ciliated pseudostratified columnar epithelium (prismatic multi-row epithelium) may undergo focal metaplasia, transforming into stratified squamous epithelium, which is less effective at mucociliary clearance.
- Vascular Changes: Blood vessels are typically enlarged (dilated) and congested, with signs of endothelial swelling and proliferation.
- Inflammatory Cell Infiltration: A diffuse, polymorphous inflammatory infiltrate consisting of lymphocytes, plasma cells, eosinophils (especially in allergic or eosinophilic forms), and neutrophils is usually present.
- Glandular Changes: The number and status of mucosal glands can vary considerably, often showing a mixed picture of hypertrophy, atrophy, or cystic dilation.
- Focal Sclerosis: Chronic inflammation can lead to focal areas of fibrosis (scarring) within the mucous membrane.
- Osseous Tissue Changes: In long-standing cases, changes in the thin bony walls (lamellae) of the ethmoid cells can occur, including signs of chronic osteitis (bone inflammation) or osteomyelitis, and focal fibrosis of the bone marrow.
- Polyp Formation: Protrusion of edematous, inflamed mucosa can lead to the development of nasal polyps.
Symptoms of Chronic Ethmoid Sinusitis (Ethmoiditis)
Chronic ethmoid sinusitis often has an insidious or latent course, with symptoms that may be persistent but less intense than acute episodes, or characterized by periods of exacerbation. Common symptoms include:
- Nasal Congestion or Blockage: A persistent feeling of stuffiness in the nose.
- Nasal Discharge: This can vary:
- Posterior Nasal Drip: Sensation of mucus dripping down the back of the throat, often leading to throat clearing or chronic cough. This is very common with ethmoiditis.
- Anterior Rhinorrhea: Runny nose, with discharge that can be clear, mucoid, or mucopurulent (thick, yellowish, or greenish), especially during exacerbations. Scanty discharge may lead to crust formation within the nasal passages.
- Facial Pain or Pressure: Patients may notice a dull, aching, or squeezing pain or pressure localized to:
- The root of the nose (between the eyes).
- Behind the eyes or in the medial canthal area (inner corner of the eye).
- Sometimes radiating to the forehead or temples.
- Reduced Sense of Smell (Hyposmia) or Loss of Smell (Anosmia): Due to inflammation and obstruction around the olfactory cleft.
- Headache: Often described as a dull, persistent headache, particularly in the mid-facial or frontal region.
- Chronic Cough: Especially worse at night, triggered by post-nasal drip.
- Fatigue and Malaise: A general feeling of being unwell or tired.
- Bad Breath (Halitosis).
- Sore Throat or Irritation: From post-nasal drip.
- Local Hyperplasia of the Middle Turbinate: Long-standing chronic ethmoiditis can lead to enlargement of the middle turbinate.
In debilitated patients, or those with underlying conditions like allergies or immune deficiencies, chronic ethmoiditis may be more persistent or severe. When the anterior and middle groups of ethmoid cells are predominantly affected, discharge is often seen in the middle and lower sections of the nasal cavity during rhinoscopy. If the posterior group of ethmoid cells is primarily involved, discharge tends to drain into the superior part of the nasal cavity and the nasopharynx.
Diagnosis of Chronic Ethmoid Sinusitis (Ethmoiditis)
The diagnosis of chronic ethmoid sinusitis relies on a combination of patient history (symptoms lasting 12 weeks or more), physical examination findings, and objective evidence from imaging or endoscopy:
- Medical History: Detailed questioning about the duration, nature, and severity of symptoms (nasal obstruction, discharge, facial pain/pressure, loss of smell), history of acute sinus infections, allergies, previous treatments, and any underlying medical conditions.
- Physical Examination:
- Anterior Rhinoscopy: May reveal mucosal edema, purulent discharge in the middle or superior meatus, or nasal polyps.
- Nasal Endoscopy: This is a key diagnostic tool. A thin, lighted endoscope is inserted into the nasal cavity to directly visualize the ethmoid sinus drainage areas (ostiomeatal complex, sphenoethmoidal recess), the appearance of the mucosa, the presence of pus, inflammation, polyps, or anatomical abnormalities.
- Imaging Studies:
- Computed Tomography (CT) Scan of the Paranasal Sinuses: This is the gold standard imaging modality for diagnosing chronic rhinosinusitis. It provides detailed images of the ethmoid air cells and surrounding structures, showing mucosal thickening, opacification (fluid or pus), bone changes, and any anatomical variations that might predispose to sinusitis. CT scans are typically performed without contrast unless a tumor or complicated infection is suspected.
- Plain X-rays: Generally have limited utility in diagnosing chronic ethmoiditis due to the complex anatomy and superimposition of structures, but may show general sinus opacification.
- Nasal Cultures: If purulent discharge is obtained, especially via endoscopy from the middle meatus, a sample may be sent for bacterial and/or fungal culture and sensitivity testing to guide antibiotic therapy, particularly if empiric treatment has failed or if surgery is planned.
- Allergy Testing: If allergies are suspected as a contributing factor, skin prick tests or specific IgE blood tests may be recommended.
- Biopsy: If nasal polyps or suspicious lesions are present, a biopsy may be taken during endoscopy for histopathological examination to rule out other conditions like fungal sinusitis or neoplasm.
A diagnostic puncture and lavage of the ethmoid sinuses was historically performed in some settings but is less common now with the advent of high-quality endoscopy and CT imaging.
Treatment Approaches for Chronic Ethmoid Sinusitis (Ethmoiditis)
The goals of treating chronic ethmoid sinusitis are to reduce mucosal inflammation, promote sinus drainage, eradicate infection, alleviate symptoms, and prevent recurrences and complications.
Conservative Management Challenges
Conservative medical treatment alone for chronic ethmoid sinusitis is often insufficient to provide lasting relief, especially if significant anatomical obstruction, polyps, or well-established chronic inflammation with biofilms are present. While medications can provide temporary subsidence of the inflammatory process, they may not address the underlying issues leading to chronicity. This can create a false premise for discontinuing treatment prematurely, leading to recurrent symptoms.
Medical therapies typically include:
- Nasal Saline Irrigation: Regular use helps to clear mucus, irritants, and allergens.
- Intranasal Corticosteroids: Long-term use is often necessary to control inflammation.
- Antibiotics: Longer courses (e.g., 3-6 weeks) may be used, ideally guided by culture results if purulence is evident. However, their role in non-purulent chronic rhinosinusitis is debated.
- Oral Corticosteroids: Short courses can be effective for severe inflammation or to shrink polyps, but long-term use has significant side effects.
- Leukotriene Modifiers or Antihistamines: If an allergic component is present.
- Biologic Agents: For severe chronic rhinosinusitis with nasal polyps (CRSwNP) unresponsive to other treatments, newer biologic therapies targeting specific inflammatory pathways (e.g., anti-IgE, anti-IL-5, anti-IL-4/13) may be considered.
Diagnostic and Therapeutic Puncture/Lavage
Historically, puncture and lavage (washing out) of the ethmoid sinuses were sometimes performed for both diagnostic (obtaining samples for culture) and therapeutic purposes (removing infected secretions and instilling medication). Specialized needles were designed for this, some with multiple distal holes for broader irrigation and a PTFE nozzle as a depth limiter. Indications included edematous-catarrhal and purulent forms unresponsive to conservative treatment, or to assess the drainage system in cases of middle turbinate hypertrophy. The procedure involved analgesia of the middle nasal passage mucosa (e.g., with 3% cocaine or 2% lidocaine solution) and careful needle insertion. After aspirating contents, the sinus could be washed with sterile saline, and antibiotics or antiseptics instilled. A drainage tube might be temporarily fixed in place. However, with modern endoscopic techniques, direct visualization and targeted interventions are generally preferred over blind puncture.
Surgical Intervention (Functional Endoscopic Sinus Surgery - FESS)
If medical management fails to control symptoms or if there are significant anatomical obstructions or complications like extensive polyposis, surgical intervention is often necessary. The standard surgical approach for chronic ethmoiditis is **Functional Endoscopic Sinus Surgery (FESS)**.
The goals of FESS are to:
- Remove diseased tissue (e.g., inflamed mucosa, polyps, infected bone).
- Enlarge the natural drainage pathways of the ethmoid sinuses.
- Improve ventilation of the sinuses.
- Facilitate the delivery of topical medications (e.g., nasal steroid sprays, rinses) to the sinus cavities postoperatively.
- Preserve as much healthy mucosa as possible.
FESS is performed using endoscopes inserted through the nostrils, providing excellent visualization. Specialized micro-instruments are used to carefully open the ethmoid air cells (ethmoidectomy), remove blockages, and address any associated issues in other sinuses if present. The extent of surgery depends on the severity and distribution of the disease.
Postoperatively, meticulous nasal care, including saline irrigations and often continued use of topical corticosteroids, is crucial for successful healing and long-term outcomes.
Differential Diagnosis of Mid-Facial Pain/Pressure and Nasal Discharge
When a patient presents with chronic mid-facial pain/pressure and nasal discharge, several conditions beyond chronic ethmoiditis should be considered:
| Condition | Key Differentiating Features |
|---|---|
| Chronic Ethmoid Sinusitis | Persistent symptoms >12 weeks; pain/pressure between/behind eyes, root of nose; post-nasal drip, hyposmia; CT shows ethmoid mucosal thickening/opacification; endoscopic findings of inflammation/polyps in ethmoid region. |
| Allergic Rhinitis | Itching (nose, eyes, palate), sneezing, clear watery rhinorrhea, nasal congestion. Symptoms often seasonal or related to specific allergen exposure. Allergy testing positive. |
| Non-Allergic Rhinitis (e.g., Vasomotor) | Nasal congestion, rhinorrhea triggered by irritants, weather changes, odors, stress. Itching usually absent. Allergy tests negative. |
| Migraine or Tension-Type Headache | Headache is primary symptom. Migraine often unilateral, throbbing, with nausea/photophobia. Tension headache often bilateral, band-like. Nasal symptoms less prominent or absent unless "sinus headache" is a migraine variant. |
| Temporomandibular Joint (TMJ) Dysfunction | Facial pain often related to jaw movement, clicking/popping in jaw, ear pain, headache. Can refer pain to mid-face. |
| Dental Infection/Pain | Pain originating from upper teeth can radiate to sinuses and mid-face. Often associated with tooth sensitivity or visible dental pathology. |
| Nasal Polyposis (CRSwNP) | Severe nasal blockage, significant loss of smell, thick discharge. Polyps visible on endoscopy/CT. Ethmoids are typically involved. |
| Fungal Rhinosinusitis (e.g., Allergic Fungal, Fungus Ball) | Can cause chronic symptoms. Allergic fungal sinusitis often presents with thick, tenacious, "allergic" mucin and polyps. Fungus ball typically in one sinus. Specific CT findings. |
| Neoplasm (Tumor) of Nasal Cavity/Sinuses | Unilateral symptoms, bloody discharge, persistent pain, facial swelling, cranial nerve deficits raise suspicion. Requires imaging and biopsy. |
Potential Complications
Untreated or poorly managed chronic ethmoid sinusitis can lead to several complications, although severe ones are less common than with acute infections:
- Orbital Complications: Due to the thin lamina papyracea separating the ethmoid sinuses from the orbit, infection can spread, potentially causing preseptal cellulitis, orbital cellulitis, subperiosteal abscess, or even vision impairment.
- Intracranial Complications: Rarely, infection can extend intracranially, leading to meningitis, epidural abscess, subdural empyema, or brain abscess.
- Mucocele/Pyocele Formation: Chronic obstruction can lead to the formation of a mucocele (mucus-filled cyst) or pyocele (infected mucocele) which can expand and erode bone.
- Osteitis/Osteomyelitis: Chronic inflammation of the ethmoid bone.
- Exacerbation of Asthma: Chronic sinus inflammation can worsen asthma control.
- Persistent Olfactory Dysfunction: Long-term loss or reduction in the sense of smell.
- Development or Worsening of Nasal Polyps.
When to Consult an ENT Specialist
Patients should consult an Ear, Nose, and Throat (ENT) specialist if they experience:
- Nasal or facial symptoms (congestion, discharge, pain/pressure, loss of smell) lasting for more than 12 weeks despite primary care treatment.
- Recurrent episodes of acute sinusitis that do not fully resolve.
- Symptoms significantly impacting quality of life.
- Suspicion of nasal polyps.
- Warning signs of complications (e.g., eye swelling or vision changes, severe headache, altered mental status).
- Failure of conservative medical management to improve chronic symptoms.
An ENT specialist can perform a comprehensive evaluation, including nasal endoscopy and CT imaging if necessary, to confirm the diagnosis, assess the extent of disease, and recommend an appropriate, individualized treatment plan, which may include advanced medical therapies or surgical intervention.
References
- Fokkens WJ, Lund VJ, Hopkins C, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020 (EPOS 2020). Rhinology. 2020 Feb 20;58(Suppl S29):1-464.
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015 Apr;152(2 Suppl):S1-S39.
- Benninger MS, Ferguson BJ, Hadley JA, et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg. 2003 Sep;129(3 Suppl):S1-S32.
- Lund VJ, Kennedy DW. Staging for rhinosinusitis. Rhinology. 1995;33(4):183-4. (Historical staging, context for CT)
- Stammberger H. Functional endoscopic sinus surgery. The Messerklinger technique. Philadelphia: BC Decker; 1991. (Seminal work on FESS)
- Kennedy DW. Prognostic factors, outcomes and staging in ethmoid sinus surgery. Laryngoscope. 1992 Oct;102(10 Pt 2 Suppl 57):1-18.
- Hopkins C. Chronic Rhinosinusitis with Nasal Polyps. N Engl J Med. 2019 Jul 4;381(1):55-63.
See also
Nasal cavity diseases:
- Runny nose, acute rhinitis, rhinopharyngitis
- Allergic rhinitis and sinusitis, vasomotor rhinitis
- Chlamydial and Trichomonas rhinitis
- Chronic rhinitis: catarrhal, hypertrophic, atrophic
- Deviated nasal septum (DNS) and nasal bones deformation
- Nosebleeds (Epistaxis)
- External nose diseases: furunculosis, eczema, sycosis, erysipelas, frostbite
- Gonococcal rhinitis
- Changes of the nasal mucosa in influenza, diphtheria, measles and scarlet fever
- Nasal foreign bodies (NFBs)
- Nasal septal cartilage perichondritis
- Nasal septal hematoma, nasal septal abscess
- Nose injuries
- Ozena (atrophic rhinitis)
- Post-traumatic nasal cavity synechiae and choanal atresia
- Nasal scabs removing
- Rhinitis-like conditions (runny nose) in adolescents and adults
- Rhinogenous neuroses in adolescents and adults
- Smell (olfaction) disorders
- Subatrophic, trophic rhinitis and related pathologies
- Nasal breathing and olfaction (sense of smell) disorders in young children
Paranasal sinuses diseases:
- Acute and chronic frontal sinusitis (frontitis)
- Acute and chronic sphenoid sinusitis (sphenoiditis)
- Acute ethmoiditis (ethmoid sinus inflammation)
- Acute maxillary sinusitis (rhinosinusitis)
- Chronic ethmoid sinusitis (ethmoiditis)
- Chronic maxillary sinusitis (rhinosinusitis)
- Infantile maxillary sinus osteomyelitis
- Nasal polyps
- Paranasal sinuses traumatic injuries
- Rhinogenic orbital and intracranial complications
- Tumors of the nose and paranasal sinuses, sarcoidosis