Acute and chronic sphenoid sinusitis (sphenoiditis)
Understanding Sphenoid Sinusitis (Sphenoiditis)
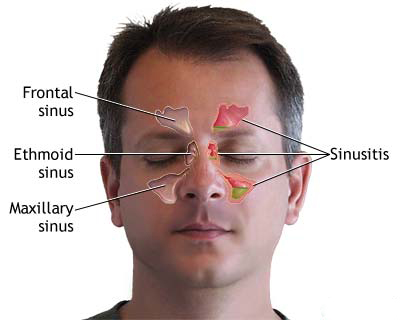
Sphenoiditis refers to the inflammation of the mucosal lining of the sphenoid sinus(es). The sphenoid sinuses are a pair of air-filled cavities located deep within the skull, in the body of the sphenoid bone, posterior to the ethmoid sinuses and nasal cavity, and inferior to the pituitary gland and optic chiasm. Due to their deep and relatively inaccessible location, isolated sphenoiditis is less common than inflammation of other paranasal sinuses.
Anatomy and Clinical Significance
Sphenoiditis frequently occurs in conjunction with inflammation of the posterior group of ethmoid sinus cells (posterior ethmoiditis) due to their close anatomical relationship and shared drainage pathways into the sphenoethmoidal recess. Less commonly, it may be associated with frontal sinusitis or maxillary sinusitis as part of a pansinusitis (inflammation of multiple or all paranasal sinuses). The symptoms of sphenoiditis can therefore overlap significantly with those of other sinus infections.
The proximity of the sphenoid sinuses to critical neurovascular structures—such as the optic nerves, internal carotid arteries, cavernous sinuses, pituitary gland, and cranial nerves III, IV, V1, V2, and VI—means that sphenoiditis, though relatively uncommon, carries a risk of serious orbital and intracranial complications if not diagnosed and treated promptly.
Symptoms of Sphenoiditis
The symptoms of sphenoiditis can be vague and non-specific, often leading to diagnostic delays. Common manifestations include:
- Headache: This is a prominent symptom. The headache in sphenoiditis is often described as non-localized, deep-seated, or difficult for the patient to pinpoint. It may be felt in various locations:
- Occipital region (back of the head)
- Vertex (crown of the head)
- Frontal or temporal regions
- Retro-orbital (behind the eyes)
- Sometimes described as a "headache in the middle of the head."
- Post-Nasal Drip: Discharge from the sphenoid sinus drains posteriorly into the nasopharynx, leading to a sensation of mucus dripping down the throat. This can cause throat clearing, cough, or a sore throat. Anterior nasal discharge is less common with isolated sphenoiditis unless there is coexisting anterior sinusitis.
- Nasal Congestion: May be present but is often less prominent than with anterior sinus infections.
- Vertigo or Dizziness: Can occasionally occur.
- Visual Disturbances: If the optic nerve or cavernous sinus is affected (rare, indicates complication), symptoms like blurred vision, double vision (diplopia), or pain with eye movement may arise.
- Cranial Nerve Palsies: Involvement of cranial nerves passing near the sphenoid sinus can lead to specific neurological deficits (e.g., ophthalmoplegia).
- Fever and Malaise: May be present, especially in acute sphenoiditis.
- Neck Pain or Stiffness.
Diagnosis of Sphenoiditis
The diagnosis of sphenoiditis is based on a combination of clinical manifestations identified during an ENT examination, imaging studies, and sometimes diagnostic procedures like probing or puncture (though the latter are less commonly performed as primary diagnostic tools today).
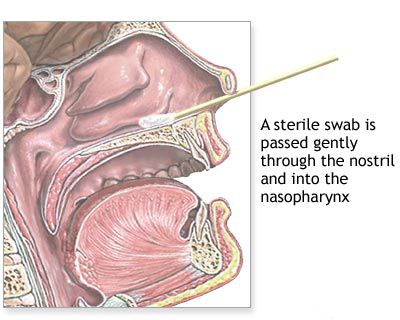
- Clinical Evaluation: A thorough history focusing on the nature of headaches, post-nasal drip, and any associated neurological or visual symptoms. Nasal endoscopy performed by an ENT doctor is crucial to visualize the sphenoethmoidal recess (where the sphenoid sinus ostium is located) for signs of inflammation or purulent discharge.
- Imaging Studies:
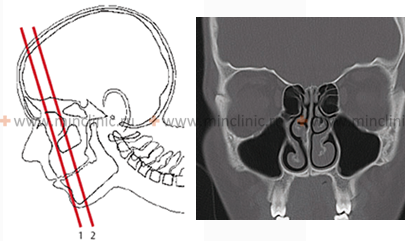
- Computed Tomography (CT) of the Paranasal Sinuses: This is the gold standard for diagnosing sphenoiditis. CT scans provide detailed images of the sphenoid sinus anatomy, showing mucosal thickening, air-fluid levels, opacification, or bony erosion. Axial, coronal, and sagittal views are important.
- Magnetic Resonance Imaging (MRI): MRI may be used if complications such as intracranial extension, optic nerve involvement, or cavernous sinus thrombosis are suspected, or to differentiate soft tissue inflammation from tumors.
- Plain X-ray Examination: Lateral skull X-rays can sometimes show opacification of the sphenoid sinus, but they have limited sensitivity and specificity compared to CT.
- Diagnostic Probing and Puncture of the Sphenoid Sinus (Historical and Current Context):
- Probing: To diagnose sphenoiditis, the sphenoid sinus can be probed, ideally under direct vision using an endoscope or operating microscope, especially if the olfactory cleft is wide. If anatomical conditions are unfavorable (e.g., narrow olfactory cleft, obstructing middle turbinate), thorough anesthesia and anemization of the olfactory area are necessary. The middle nasal concha might need to be gently displaced medially (e.g., with a Killian's nasal speculum) to visualize the natural ostium located near the roof of the nose. Probing is performed with a probe slightly curved at the end or a cannula probe at least 10 cm long. The distance from the nasal entrance to the anterior wall of the sphenoid sinus in older children and adults is approximately 8 cm, and about 3 cm from the posterior edge of the nasal septum.
The probing technique for sphenoiditis involves using a self-retaining nasal dilator. With the patient's head tilted back, the end of the probe is placed on the lower edge of the nasal entrance and guided along the nasal septum (without deviating laterally) towards the middle of the lower edge of the middle nasal concha, aiming for the natural sphenoid ostium. A characteristic sensation is often felt upon entering the sinus. The sphenoid sinus can then be flushed using a graduated cannula or a thin ear catheter (no more than 2 mm in diameter).
Challenges in probing arise because the natural sphenoid ostium is small (about 1 mm in diameter), and the probe may not easily penetrate it. If the probe is directed too superiorly from the anterior part of the middle turbinate, there is a risk of penetrating the cribriform plate and entering the cranial cavity. It is generally safer to aim slightly lower and more posteriorly than this landmark. Failures can also occur due to the highly variable shape of the sphenoid sinus, which may have additional septa, ridges, be rudimentary, or even completely absent on one side.
- Puncture: An original method involving puncture of the sphenoid sinus by accurately determining the angle using a sighting device is generally not used in children due to its technical difficulty and feasibility issues. When performed, sinus puncture allows for aspiration of contents for culture and cytology, and for therapeutic lavage.
- Probing: To diagnose sphenoiditis, the sphenoid sinus can be probed, ideally under direct vision using an endoscope or operating microscope, especially if the olfactory cleft is wide. If anatomical conditions are unfavorable (e.g., narrow olfactory cleft, obstructing middle turbinate), thorough anesthesia and anemization of the olfactory area are necessary. The middle nasal concha might need to be gently displaced medially (e.g., with a Killian's nasal speculum) to visualize the natural ostium located near the roof of the nose. Probing is performed with a probe slightly curved at the end or a cannula probe at least 10 cm long. The distance from the nasal entrance to the anterior wall of the sphenoid sinus in older children and adults is approximately 8 cm, and about 3 cm from the posterior edge of the nasal septum.
Treatment of sphenoiditis is most often conservative. However, in cases of complicated pansinusitis, or if orbital or intracranial symptoms related to sphenoiditis arise, surgical intervention is typically required.
Treatment of Acute and Chronic Sphenoiditis
The management of sphenoiditis depends on whether it is acute or chronic, the severity of symptoms, and the presence of any complications.
Conservative Medical Management
For most cases of uncomplicated acute sphenoiditis and as initial therapy for chronic sphenoiditis, conservative medical management is the first line of approach:
- Antibiotics: If a bacterial infection is suspected (especially in acute cases with purulent discharge, fever, or prolonged symptoms), a course of appropriate antibiotics is prescribed. The choice may be empiric initially, covering common sinus pathogens, or guided by culture results if available (e.g., from endoscopic sampling).
- Nasal Decongestants: Topical (sprays/drops) or oral decongestants can help reduce mucosal swelling around the sphenoid ostium and improve drainage. Topical agents should be used for a limited duration (3-5 days).
- Intranasal Corticosteroids: These are crucial for reducing mucosal inflammation in both acute and chronic sphenoiditis. Long-term use is often necessary for chronic conditions.
- Nasal Saline Irrigation: Helps to clear secretions from the nasal passages and nasopharynx, improving comfort and potentially facilitating drainage from the sphenoethmoidal recess.
- Analgesics: For pain relief (e.g., acetaminophen, NSAIDs).
- Mucolytics: May help thin tenacious secretions.
- Management of Underlying Conditions: If allergies or other predisposing factors are present, they should be addressed.
Surgical Intervention for Sphenoiditis
Surgical intervention is typically reserved for cases of chronic sphenoiditis unresponsive to maximal medical therapy, recurrent acute sphenoiditis, sphenoid sinus mucocele, fungal sphenoiditis (fungus ball), or if complications arise.
The primary surgical procedure is **endoscopic sphenoidotomy**, performed under local or general anesthesia. The goals are to:
- Create a widely patent opening into the sphenoid sinus to ensure adequate long-term drainage and ventilation.
- Remove any diseased tissue, polyps, or fungal debris from within the sinus.
- Facilitate postoperative topical medication delivery.
The essence of the operation is to create conditions for drainage by removing the anterior wall of the sinus, which is sometimes facilitated by an atrophic process in the nasal cavity where the natural opening of the sinus might be more visible. Various approaches can be used:
- Transnasal Endoscopic Approach: The most common method. The endoscope is passed through the nasal cavity, and the sphenoid ostium is identified in the sphenoethmoidal recess. The ostium is then enlarged, or the anterior wall of the sphenoid sinus is opened. This may be done directly (transostial) or sometimes via a transethmoidal approach if posterior ethmoidectomy is also required.
- Transethmoidal Approach: In some cases, particularly if there is coexisting posterior ethmoiditis, the sphenoid sinus is accessed after performing a posterior ethmoidectomy. This involves sequentially opening all posterior ethmoid cells, after previously (if necessary) resecting the middle turbinate, correcting a deviated nasal septum, or removing nasal polyps to gain access. A hook, probe, or sharp elongated spoon is then inserted into the natural ostium of the sphenoid sinus, or the anterior wall of the sinus is resected using specialized chisels, cutters, or powered instruments (microdebrider). Sometimes, not only the anterior but also part of the lower wall is removed, or the sinus is opened using elongated burs under endoscopic guidance.
- Transseptal Approach: Less commonly, the sphenoid sinus can be approached by traversing the nasal septum.
Extranasal approaches to the sphenoid sinus are rarely used today for inflammatory disease due to the efficacy of endoscopic techniques.
Ozone Therapy as an Adjunctive Treatment
Local ozone therapy has been proposed as an adjunctive treatment for purulent sinusitis, including sphenoiditis, particularly for patients with hypersensitivity to standard antibiotics or antiseptics. The proposed regimen involves:
- Sinus Lavage: Washing the inflamed sinuses with a physiological saline solution containing ozone at a concentration of 6-8 mg/L to evacuate purulent discharge.
- Ozone Insufflation: Subsequent saturation of the sinus mucosa with ozone by aerating the sinuses for 15-20 minutes with an ozone-oxygen gas mixture (ozone concentration 6-8 mg/L).
- Concentration Adjustment: As inflammation and pus discharge decrease, it is recommended to reduce the ozone concentration to 3-4 mg/L to potentially stimulate tissue regeneration.
- Hydrocortisone Suspension: Local ozone therapy may be supplemented with the introduction of a hydrocortisone suspension into the affected sinuses to relieve mucosal swelling and inflammation around the anastomosis (opening).
- Parenteral Ozone Therapy: For patients with severe symptoms of intoxication, intravenous administration of ozonated physiological saline (ozone content 0.8-1 mg/L, 400 ml every other day, for a course of 3 to 6 infusions) has been suggested. The duration is determined by the patient's general condition and resolution of intoxication signs. Due to the relative instability of ozone in physiological solution, drip infusion is advisable.
It is important to note that while ozone therapy is explored in some regions, its efficacy and safety for sinusitis are not universally established by robust, large-scale clinical trials, and it is not considered a standard part of mainstream international treatment guidelines for sinusitis. Its use should be considered experimental or adjunctive and undertaken by practitioners experienced in this modality.
Differential Diagnosis of Sphenoiditis Symptoms
The often vague and non-specific symptoms of sphenoiditis, particularly headache, require careful differentiation from other conditions:
| Condition | Key Differentiating Features |
|---|---|
| Sphenoid Sinusitis | Deep-seated, often non-localized headache (occipital, vertex, retro-orbital); post-nasal drip; +/- fever, nasal congestion. Diagnosis confirmed by endoscopy (pus in sphenoethmoidal recess) and CT/MRI showing sphenoid sinus inflammation/opacification. |
| Migraine Headache | Often unilateral, throbbing, associated with nausea, vomiting, photophobia, phonophobia; may have aura. Nasal symptoms can occur ("sinus migraine") but sinus imaging usually normal. |
| Tension-Type Headache | Bilateral, band-like pressure or tightness; often related to stress/muscle tension. Usually no fever or purulent nasal discharge. |
| Cluster Headache | Severe, excruciating, unilateral periorbital/temporal pain; occurs in clusters; associated autonomic symptoms (tearing, nasal congestion, ptosis on affected side). |
| Posterior Ethmoiditis | Very similar symptoms to sphenoiditis due to close proximity and shared drainage. Often coexists. Differentiated by imaging. |
| Pituitary Apoplexy or Tumor | Severe headache, visual disturbances (bitemporal hemianopsia, ophthalmoplegia), endocrine dysfunction. Requires urgent neuroimaging (MRI). |
| Cavernous Sinus Thrombosis | Headache, proptosis, ophthalmoplegia (CN III, IV, VI palsies), periorbital edema, fever, sepsis. Life-threatening emergency. Often secondary to facial or sinus infection. |
| Temporal Arteritis (Giant Cell Arteritis) | Typically in older adults (>50); new-onset headache (often temporal), scalp tenderness, jaw claudication, visual symptoms. Elevated ESR/CRP. |
| Cervicogenic Headache | Pain referred from cervical spine structures. Often occipital or suboccipital, may radiate to head. Related to neck movement/posture. |
Potential Complications of Sphenoiditis
Due to the sphenoid sinus's proximity to critical neurovascular structures, untreated or aggressive sphenoiditis can lead to severe complications:
- Orbital Complications:
- Optic neuritis leading to visual impairment or blindness (due to proximity of optic nerve).
- Orbital apex syndrome (involvement of CN II, III, IV, V1, VI).
- Superior orbital fissure syndrome.
- Intracranial Complications:
- Cavernous sinus thrombosis.
- Meningitis.
- Epidural, subdural, or brain abscess (especially temporal or frontal lobes).
- Pituitary abscess or dysfunction.
- Carotid artery involvement (aneurysm, vasospasm - very rare).
- Neurological Deficits: Cranial nerve palsies (III, IV, V, VI are most at risk).
- Sphenoid Sinus Mucocele/Pyocele: Can expand and erode surrounding bone, compressing adjacent structures.
These complications are medical emergencies requiring immediate and aggressive management.
Prevention and When to Seek Specialist Care
Prevention involves:
- Prompt and effective treatment of acute upper respiratory infections and rhinosinusitis involving other sinuses to prevent spread to the sphenoid.
- Management of underlying predisposing factors like allergies or anatomical issues.
Consultation with an ENT specialist is crucial if sphenoiditis is suspected, especially if experiencing:
- Persistent, severe, or unusual headaches (especially occipital, vertex, or retro-orbital).
- Persistent post-nasal drip unresponsive to standard treatments.
- Any visual disturbances (blurred vision, double vision, decreased vision).
- Pain with eye movements or restricted eye movements.
- Unexplained fever with headache and nasal symptoms.
- Neurological symptoms such as facial numbness, weakness, or altered mental status.
Early diagnosis and treatment of sphenoiditis are vital to prevent potentially devastating complications due to its deep anatomical location and proximity to critical structures.
References
- Lew D, Southwick FS, Montgomery WW, Weber AL, Baker AS. Sphenoid sinusitis. A review of 30 cases. N Engl J Med. 1983 Jan 27;308(4):178-82.
- Fokkens WJ, Lund VJ, Hopkins C, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020 (EPOS 2020). Rhinology. 2020 Feb 20;58(Suppl S29):1-464.
- Soh KB, Tan KK. Isolated sphenoid sinusitis: a diagnostic dilemma? Med J Malaysia. 2000 Dec;55(4):488-92.
- Lawson W, Reino AJ. Isolated sphenoid sinus disease: an analysis of 132 cases. Laryngoscope. 1997 Dec;107(12 Pt 1):1590-5.
- Friedman A, Batra PS, Fakhri S, Citardi MJ, Lanza DC. Isolated sphenoid sinus disease: etiology and management. Otolaryngol Head Neck Surg. 2005 Apr;132(4):518-25.
- Grillone GA, Nuss DW. Management of isolated sphenoid sinus disease. Otolaryngol Clin North Am. 2005 Feb;38(1):161-76.
- Deosthali A, Roplekar S, Singh R, Pathak S. Sphenoid Sinusitis: A Clinical Enigma. Indian J Otolaryngol Head Neck Surg. 2016 Dec;68(4):442-446.
- Lee LA. Sphenoid sinusitis: a common cause for headache. J Am Board Fam Pract. 2001 Nov-Dec;14(6):448-54.
See also
Nasal cavity diseases:
- Runny nose, acute rhinitis, rhinopharyngitis
- Allergic rhinitis and sinusitis, vasomotor rhinitis
- Chlamydial and Trichomonas rhinitis
- Chronic rhinitis: catarrhal, hypertrophic, atrophic
- Deviated nasal septum (DNS) and nasal bones deformation
- Nosebleeds (Epistaxis)
- External nose diseases: furunculosis, eczema, sycosis, erysipelas, frostbite
- Gonococcal rhinitis
- Changes of the nasal mucosa in influenza, diphtheria, measles and scarlet fever
- Nasal foreign bodies (NFBs)
- Nasal septal cartilage perichondritis
- Nasal septal hematoma, nasal septal abscess
- Nose injuries
- Ozena (atrophic rhinitis)
- Post-traumatic nasal cavity synechiae and choanal atresia
- Nasal scabs removing
- Rhinitis-like conditions (runny nose) in adolescents and adults
- Rhinogenous neuroses in adolescents and adults
- Smell (olfaction) disorders
- Subatrophic, trophic rhinitis and related pathologies
- Nasal breathing and olfaction (sense of smell) disorders in young children
Paranasal sinuses diseases:
- Acute and chronic frontal sinusitis (frontitis)
- Acute and chronic sphenoid sinusitis (sphenoiditis)
- Acute ethmoiditis (ethmoid sinus inflammation)
- Acute maxillary sinusitis (rhinosinusitis)
- Chronic ethmoid sinusitis (ethmoiditis)
- Chronic maxillary sinusitis (rhinosinusitis)
- Infantile maxillary sinus osteomyelitis
- Nasal polyps
- Paranasal sinuses traumatic injuries
- Rhinogenic orbital and intracranial complications
- Tumors of the nose and paranasal sinuses, sarcoidosis