Osteoporosis
What is Osteoporosis?
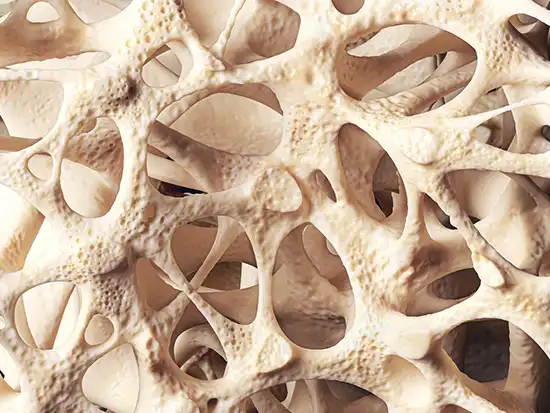
Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, resulting from an imbalance where bone resorption (breakdown) outpaces bone formation. This leads to enhanced bone fragility and a consequent increase in fracture risk.
Essentially, osteoporosis causes bones to become more porous, weaker, and less dense, making them more susceptible to fractures even from minor stress or falls.
The development of osteoporosis is often linked to age-related changes (particularly post-menopause in women), prolonged use of certain medications (like corticosteroids), and the presence of various chronic diseases that disrupt metabolism, including calcium and vitamin D metabolism.
Osteoporosis most commonly leads to fractures of the hip, wrist, and spine (vertebral compression fractures).
Osteoporosis Classification
Osteoporosis can be broadly classified into primary and secondary types:
A. Primary Osteoporosis: Occurs without a known underlying cause, often related to aging and hormonal changes.
- Postmenopausal Osteoporosis (Type I): Affects women after menopause due to estrogen deficiency.
- Senile Osteoporosis (Type II): Affects both men and women, typically over age 70, related to aging processes and changes in calcium/vitamin D metabolism.
- Juvenile Osteoporosis: Rare form occurring in children and adolescents.
- Idiopathic Osteoporosis: Occurs in younger adults with no identifiable cause.
B. Secondary Osteoporosis: Results from specific medical conditions, medications, or lifestyle factors.
- Associated with underlying medical conditions:
- Endocrine disorders (e.g., hyperparathyroidism, hyperthyroidism, Cushing's syndrome, diabetes mellitus, hypogonadism, primary ovarian insufficiency).
- Gastrointestinal diseases (e.g., malabsorption syndromes like Celiac disease, inflammatory bowel disease).
- Rheumatic diseases (e.g., rheumatoid arthritis, systemic lupus erythematosus).
- Chronic kidney disease.
- Hematologic disorders (e.g., multiple myeloma).
- Genetic disorders (e.g., osteogenesis imperfecta).
- Iatrogenic (medication-induced): Caused by treatment with certain drugs, including:
- Glucocorticoids (corticosteroids) - most common drug cause.
- Certain anti-seizure medications.
- Heparin (long-term use).
- Excess thyroid hormone replacement.
- Aromatase inhibitors (used for breast cancer).
- Proton pump inhibitors (long-term use).
- Immunosuppressants.
- Other factors: Immobilization, malnutrition, excessive alcohol intake.
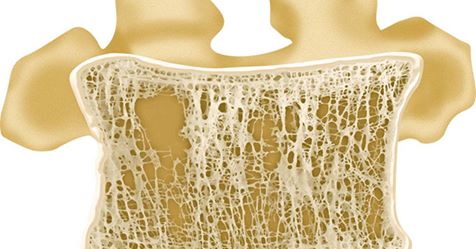
A frontal view (cut) of a vertebral body showing osteoporosis of the cancellous (spongy) bone. This weakening can subsequently lead to a compression fracture.
Compression fracture of a thoracic vertebra, side view, often a consequence of osteoporosis.
Risk Factors for Osteoporosis
Several factors can increase the likelihood of developing osteoporosis. Some are non-modifiable, while others relate to lifestyle or medical conditions:
- Non-Modifiable Factors:
- Advanced age
- Female sex
- Ethnicity (higher risk in White and Asian individuals)
- Family history of osteoporosis or fragility fractures (especially hip fracture in a parent)
- Low body weight / small body frame
- Previous fragility fracture
- Certain genetic disorders
- Hormonal Factors:
- Estrogen deficiency (menopause, oophorectomy, premature menopause before age 45)
- Low testosterone levels (hypogonadism in men)
- Hyperparathyroidism
- Hyperthyroidism
- Cushing's syndrome
- Nutritional Deficiencies:
- Low calcium intake
- Vitamin D deficiency
- Excessive intake of alcohol (>2-3 drinks/day)
- High caffeine intake
- High salt intake
- Malnutrition / Malabsorption
- Lifestyle Factors:
- Smoking (current or past)
- Sedentary lifestyle / Lack of weight-bearing exercise
- Immobilization
- Medications:
- Glucocorticoids (e.g., prednisone) - dose and duration dependent
- Long-term heparin use
- Certain anti-seizure drugs (e.g., phenytoin, phenobarbital)
- Aromatase inhibitors
- Proton pump inhibitors (long-term use)
- Excess thyroid hormone
- Certain immunosuppressants (e.g., cyclosporine)
- Chemotherapy agents
- Comorbid Medical Conditions: (As listed under Secondary Osteoporosis)
Osteoporosis Diagnosis
The diagnosis of osteoporosis involves assessing risk factors, clinical evaluation, and objective measurement of bone density.
Clinical Evaluation: A thorough medical history (including risk factors, previous fractures, family history) and physical examination are essential. Height loss or development of kyphosis (stooped posture) can be suggestive.
Bone Mineral Density (BMD) Testing: The gold standard for diagnosis is measuring BMD using Dual-energy X-ray Absorptiometry (DXA or DEXA). This non-invasive test measures bone density, typically at the hip and spine. Results are reported as T-scores and Z-scores:
- T-score: Compares the patient's BMD to the average BMD of a healthy young adult of the same sex. According to the World Health Organization (WHO):
- T-score ≥ -1.0: Normal bone density
- T-score between -1.0 and -2.5: Low bone mass (Osteopenia)
- T-score ≤ -2.5: Osteoporosis
- T-score ≤ -2.5 with one or more fragility fractures: Severe Osteoporosis
- Z-score: Compares the patient's BMD to the average BMD of people of the same age and sex. A Z-score ≤ -2.0 may suggest secondary causes of osteoporosis.
Bone Densitometry (DXA Scan) is the standard procedure for measuring bone mineral density (BMD) to diagnose osteoporosis.
Fracture Risk Assessment Tool (FRAX): This tool, developed by the WHO, uses clinical risk factors (with or without BMD) to estimate the 10-year probability of major osteoporotic fracture (hip, spine, forearm, humerus) and hip fracture specifically. It helps guide treatment decisions, especially for individuals with osteopenia.
Laboratory Tests: Blood tests may be ordered to rule out secondary causes of osteoporosis or conditions mimicking it. These can include:
- Serum calcium, phosphate, alkaline phosphatase
- Vitamin D level (25-hydroxyvitamin D)
- Kidney function tests (creatinine)
- Thyroid function tests (TSH)
- Parathyroid hormone (PTH) levels
- Complete blood count (CBC)
- Testosterone levels (in men)
- Tests for celiac disease or malabsorption if suspected
- Serum protein electrophoresis (if myeloma is suspected)
Imaging for Fractures: If a fracture is suspected (e.g., due to back pain, height loss), imaging studies are performed:
- X-rays: Can detect moderate to severe bone loss and confirm fractures, especially vertebral compression fractures.
- Computed Tomography (CT) Scan: Provides detailed images of bone structure and can be useful for assessing complex fractures.
- Magnetic Resonance Imaging (MRI): Useful for detecting acute vertebral fractures, assessing spinal cord or nerve root compression, and differentiating osteoporotic fractures from malignant infiltration.
Lumbar spine Computed Tomography (CT) scan reveals an L1 vertebral compression fracture, a common complication of osteoporosis.
Osteoporosis Treatment
The goals of osteoporosis treatment are to prevent fractures, stabilize or increase bone mass, relieve symptoms of fractures and skeletal deformity, and maximize physical function.
1. Lifestyle Modifications (Foundation of Treatment):
- Adequate Calcium Intake: Aim for 1000-1200 mg of elemental calcium per day (diet preferred, supplements if needed).
- Adequate Vitamin D Intake: Aim for 800-1000 IU of vitamin D per day (sun exposure, diet, supplements). Serum levels may be checked to guide supplementation.
- Regular Exercise: Include weight-bearing exercises (e.g., walking, jogging, dancing) and muscle-strengthening exercises (e.g., weight lifting). Balance exercises are also important to prevent falls.
- Fall Prevention: Assess home safety, review medications causing dizziness, check vision.
- Smoking Cessation: Smoking accelerates bone loss.
- Limit Alcohol Intake: Excessive alcohol increases fracture risk.
2. Pharmacological Therapy: Medications are typically recommended for individuals with diagnosed osteoporosis (T-score ≤ -2.5), those with osteopenia and a history of fragility fracture, or those with osteopenia and high fracture risk based on FRAX assessment.
- Bisphosphonates: (e.g., Alendronate, Risedronate, Zoledronic acid, Ibandronate) - First-line therapy for most patients. They reduce bone resorption. Available in oral (daily, weekly, monthly) and intravenous (yearly or quarterly) forms.
- Denosumab: A monoclonal antibody (RANKL inhibitor) that reduces bone resorption. Given as a subcutaneous injection every 6 months. Often used as first-line therapy or for patients intolerant to bisphosphonates.
- Anabolic Agents: (Teriparatide, Abaloparatide) - Recombinant forms of parathyroid hormone that stimulate bone formation. Used for patients with severe osteoporosis or those who haven't responded to other therapies. Given as daily subcutaneous injections for a limited duration (usually up to 2 years).
- Romosozumab: A monoclonal antibody (sclerostin inhibitor) with dual action: increases bone formation and decreases bone resorption. Given as monthly subcutaneous injections for 1 year, typically followed by an anti-resorptive agent. Reserved for high-risk patients.
- Selective Estrogen Receptor Modulators (SERMs): (e.g., Raloxifene) - Mimic estrogen's beneficial effects on bone in postmenopausal women. Primarily reduces the risk of vertebral fractures.
- Calcitonin: Less commonly used for long-term fracture prevention due to lower efficacy compared to other agents. May be used short-term (often as a nasal spray) for pain relief after an acute vertebral compression fracture.
- Hormone Replacement Therapy (HRT): Estrogen (with or without progestin) can prevent bone loss but is used cautiously due to potential risks; typically considered for younger postmenopausal women with persistent menopausal symptoms.
3. Management of Fractures:
- Pain Management: Analgesics, physical therapy, sometimes bracing.
- Surgical Intervention: May be required for certain fractures, especially hip fractures (fixation or replacement). For painful vertebral compression fractures, procedures like vertebroplasty (injecting bone cement into the fractured vertebra) or kyphoplasty (using a balloon to restore some height before injecting cement) may be considered.
- Rehabilitation: Physical and occupational therapy are crucial after a fracture to restore function and prevent future falls.
Post-fracture management always includes assessing and treating the underlying osteoporosis to prevent subsequent fractures.
Differential Diagnosis of Low Bone Density and Fractures
While osteoporosis is the most common cause of low bone density and fragility fractures, other conditions must be considered, especially if the presentation is atypical or occurs in younger individuals.
| Condition | Key Differentiating Features |
|---|---|
| Osteomalacia | Defective bone mineralization (soft bones) often due to severe Vitamin D deficiency. Features: Bone pain, muscle weakness, pseudofractures (Looser zones) on X-ray. Labs: Low/normal calcium, low phosphate, high alkaline phosphatase, very low Vitamin D. BMD may be low. |
| Multiple Myeloma | Malignancy of plasma cells. Features: Bone pain (often severe), fatigue, anemia, kidney problems. Imaging: Punched-out lytic lesions, diffuse osteopenia, fractures. Labs: Monoclonal protein (M-spike) in serum/urine, abnormal free light chains, hypercalcemia, elevated creatinine. |
| Metastatic Bone Disease | Cancer spread to bone from another primary site (e.g., breast, prostate, lung, kidney). Features: Bone pain, history of primary cancer, pathological fractures. Imaging: Lytic or blastic lesions depending on primary tumor type. |
| Primary Hyperparathyroidism | Overactive parathyroid gland(s) leading to excess PTH. Features: Often asymptomatic, but can cause kidney stones, bone pain, fatigue, constipation, depression. Labs: High serum calcium, high PTH, low/normal phosphate. Affects cortical bone more than trabecular bone initially. |
| Paget's Disease of Bone | Disordered bone remodeling leading to enlarged, deformed, and fragile bones. Features: Often localized bone pain, bone deformity, headache (if skull involved), hearing loss. Imaging: Mixed lytic and sclerotic lesions, bone expansion. Labs: Markedly elevated alkaline phosphatase. |
| Renal Osteodystrophy | Complex bone disease occurring in patients with chronic kidney disease (CKD). Features: Spectrum includes high-turnover (like hyperparathyroidism) or low-turnover (adynamic bone disease) states. Diagnosis based on clinical picture in CKD patient, PTH levels, alkaline phosphatase, possibly bone biopsy. |
References
- Kanis JA, McCloskey EV, Johansson H, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23(9):2239-2256. doi:10.1007/s00198-012-1964-3
- World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1994;843:1-129.
- Cosman F, de Beur SJ, LeBoff MS, et al. Clinician's Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25(10):2359-2381. doi:10.1007/s00198-014-2794-2 (Note: Updated guidelines may be available from the Bone Health & Osteoporosis Foundation - formerly NOF)
- Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis—2020 Update. Endocr Pract. 2020;26(Suppl 1):1-46. doi:10.4158/GL-2020-0524SUPPL
- Ensrud KE, Crandall CJ. Osteoporosis. Ann Intern Med. 2017;167(3):ITC17-ITC32. doi:10.7326/AITC201708010
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Osteoporosis. National Institutes of Health. Available at: https://www.niams.nih.gov/health-topics/osteoporosis (Accessed frequently for updates)
- Bone Health & Osteoporosis Foundation (BHOF). Clinician's Guide to Prevention and Treatment of Osteoporosis. Available at: https://www.bonehealthandosteoporosis.org/clinicians/clinicians-guides-and-position-statements/ (Accessed frequently for updates)
See also
- Achilles tendon inflammation (paratenonitis, ahillobursitis)
- Achilles tendon injury (sprain, rupture)
- Ankle and foot sprain
- Arthritis and arthrosis (osteoarthritis):
- Autoimmune connective tissue disease:
- Bunion (hallux valgus)
- Epicondylitis ("tennis elbow")
- Hygroma
- Joint ankylosis
- Joint contractures
- Joint dislocation:
- Knee joint (ligaments and meniscus) injury
- Metabolic bone disease:
- Myositis, fibromyalgia (muscle pain)
- Plantar fasciitis (heel spurs)
- Tenosynovitis (infectious, stenosing)
- Vitamin D and parathyroid hormone