Plantar Fasciitis (Fasciopathy) and Heel Spurs
What is Plantar Fasciitis / Plantar Fasciopathy?
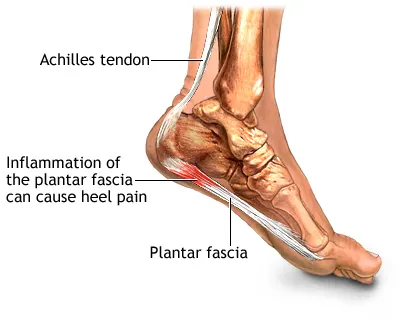
Plantar Fasciitis is one of the most common causes of heel pain. It involves inflammation, irritation, or degeneration of the plantar fascia, a thick band of connective tissue that runs across the bottom of the foot, connecting the heel bone (calcaneus) to the toes and supporting the arch (1, 2).
The condition is often considered a degenerative process (tendinosis) rather than purely inflammatory, especially in chronic cases. Therefore, the term Plantar Fasciopathy is increasingly used to encompass both inflammation (fasciitis) and degeneration (fasciosis) (1, 3).
The primary symptom is typically sharp, stabbing pain in the bottom of the heel, which is often most severe with the first steps taken in the morning or after periods of rest (post-static dyskinesia) (2, 4).
What are Heel Spurs (Calcaneal Spurs)?
A heel spur (or calcaneal spur) is a bony outgrowth (osteophyte) that can form on the underside of the heel bone (calcaneus), often near the attachment point of the plantar fascia (1, 5). They can vary in size and shape.
Important Distinction: While heel spurs are often found on X-rays of people *with* plantar fasciitis (present in about 50-70% of cases), the spur itself is rarely the direct cause of the pain (1, 2, 5). Many people have heel spurs without experiencing any pain at all. The pain typically associated with "heel spurs" actually originates from the inflamed or degenerated plantar fascia tissue, not from the bone spur pressing on soft tissues (1, 4). The spur likely forms as a response to chronic stress and pulling of the fascia on the calcaneus.
Therefore, treatment should target the plantar fasciopathy, not just the presence of a spur (1).
Causes and Risk Factors
Plantar fasciopathy is primarily thought to be caused by repetitive microtrauma and excessive strain on the plantar fascia, leading to inflammation or degeneration (1, 2, 3). Factors that increase this strain include:
- Biomechanical Issues: Foot structure abnormalities like flat feet (pes planus) or high arches (pes cavus) can alter stress distribution (2, 4).
- Tight Calf Muscles (Gastrocnemius/Soleus) or Achilles Tendon: Limited ankle dorsiflexion increases strain on the plantar fascia (1, 4).
- Obesity/Excess Weight: Increases the load on the plantar fascia with each step (1, 2).
- Occupational Factors: Jobs requiring prolonged standing or walking on hard surfaces (2, 4).
- Activity Changes: Sudden increase in the intensity, duration, or type of physical activity (e.g., running, dancing) (2).
- Inappropriate Footwear: Shoes with poor arch support, inadequate cushioning, or worn-out soles (4).
- Age: Most common between ages 40 and 60 (2).
- Less commonly associated with systemic inflammatory conditions (e.g., spondyloarthropathies).
Symptoms
The hallmark symptom is heel pain, typically characterized by (2, 4):
- Location: Sharp or stabbing pain on the bottom of the heel, near the front aspect, where the fascia attaches to the calcaneus. Pain may sometimes radiate into the arch.
- Timing: Pain is usually most severe with the first steps out of bed in the morning or after prolonged sitting/resting.
- Activity Pattern: Pain often decreases somewhat after initial walking but may return and worsen after extended periods of standing, walking, or intense activity.
- Pain is generally *not* caused by the spur itself pressing on tissue (1).
Patients may alter their gait (limp or walk on their toes) to avoid putting pressure on the painful heel.
Diagnosis
Diagnosis of plantar fasciopathy is primarily based on the patient's history and a clinical examination (1, 2, 4).
- History: Detailed description of the pain location, timing (especially morning pain), aggravating and relieving factors, activity levels, footwear, and relevant medical history.
- Physical Examination:
- Palpation: Identifying point tenderness typically at the medial calcaneal tuberosity (origin of the plantar fascia).
- Windlass Test: Passive dorsiflexion of the toes (especially the big toe) while the ankle is stabilized can recreate the heel pain by stretching the plantar fascia.
- Assessment of ankle dorsiflexion (checking for calf tightness).
- Evaluation of foot structure (arch height).
- Neurological exam to rule out nerve involvement.
- Imaging Studies: Usually not required for initial diagnosis but may be used to rule out other conditions or in persistent cases (1, 2).
- X-rays: Can identify heel spurs (but their presence doesn't confirm PF as the cause of pain) and rule out stress fractures, bone tumors, or arthritis.
- Ultrasound: Can visualize the plantar fascia, showing thickening (>4mm is often considered abnormal), hypoechogenicity (darker appearance indicating fluid/degeneration), and sometimes calcifications or tears (1, 6). Can also guide injections.
- MRI: Generally reserved for complex cases or when other diagnoses (like stress fracture or nerve entrapment) are strongly suspected. Can show fascia thickening, edema, and adjacent bone marrow edema (1, 6).
If you experience persistent heel pain, it's essential to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan (2).
Treatment
Treatment for plantar fasciopathy is typically conservative and successful in the majority of cases (around 90%), although it may take several months (1, 2, 7). The focus is on reducing strain on the fascia and controlling inflammation/degeneration.
Conservative (First-Line) Treatments:
- Rest and Activity Modification: Reducing activities that aggravate the pain (e.g., high-impact running, prolonged standing) (2).
- Stretching Exercises: Crucial component targeting both the plantar fascia itself (e.g., rolling foot over a ball/can, towel stretches) and the Achilles tendon/calf muscles (e.g., runner's stretch) (1, 7).
- Appropriate Footwear: Wearing supportive shoes with good arch support and cushioning; avoiding flat, unsupportive shoes or walking barefoot (4).
- Orthotics/Insoles: Over-the-counter or custom orthotic inserts can help support the arch and reduce strain on the fascia (1, 7). Heel cups or pads may provide cushioning.
- Ice Application: Applying ice packs to the heel for 15-20 minutes several times a day can help reduce pain and inflammation (2).
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen or naproxen can help manage pain and inflammation, particularly in the acute phase, but are less effective for chronic degeneration (1, 2).
- Night Splints: Worn during sleep to keep the foot and ankle in a dorsiflexed position, preventing the fascia from tightening overnight and reducing morning pain (1, 7).
Other Treatments (if conservative measures fail after several months):
- Physical Therapy: Formal guidance on stretching, strengthening exercises, manual therapy techniques (like soft tissue mobilization), and possibly modalities like ultrasound or iontophoresis (evidence varies) (1, 7). Myofascial release therapy may be included.
- Corticosteroid Injections: Can provide significant short-term pain relief by reducing inflammation. However, repeated injections carry risks, including fat pad atrophy or, rarely, fascia rupture (1, 2). Often reserved for persistent pain interfering with therapy.
- Extracorporeal Shockwave Therapy (ESWT): Uses sound waves directed at the heel to stimulate healing in chronic cases unresponsive to other treatments (1, 7).
- Platelet-Rich Plasma (PRP) Injections: An emerging treatment involving injecting concentrated platelets from the patient's own blood; evidence is still evolving (1).
- Surgery (Plantar Fasciotomy): Rarely needed. Involves partially cutting the plantar fascia to relieve tension. Reserved for severe, debilitating cases that have failed extensive conservative management for 6-12 months due to potential complications (1, 2, 7). Removing a heel spur is generally *not* part of the procedure unless it's exceptionally large and impinging on structures.
Treatment requires patience and consistent adherence, especially to stretching and appropriate footwear/orthotics (7).
Differential Diagnosis
Other conditions can cause heel pain and need to be considered (1, 2, 8):
| Condition | Key Differentiating Features |
|---|---|
| Calcaneal Stress Fracture | Pain often worsens *during* activity, less relief with rest compared to PF. Tenderness may be elicited by squeezing the heel bone side-to-side. May require MRI or bone scan for diagnosis if X-ray is negative. |
| Tarsal Tunnel Syndrome | Compression of the posterior tibial nerve. Pain often described as burning, tingling, or numbness, potentially radiating into the arch or toes. Positive Tinel's sign (tapping over the nerve) may be present. Nerve conduction studies can aid diagnosis. |
| Baxter's Nerve Entrapment | Entrapment of the first branch of the lateral plantar nerve. Can cause heel pain similar to PF but may lack the classic morning stiffness. Pain may be more medial or diffuse. |
| Fat Pad Atrophy | Thinning of the protective fatty tissue under the heel. Pain often feels like "walking on bone," worse on hard surfaces. More common in older adults. Tenderness is often central heel rather than at fascia insertion. |
| Achilles Tendinopathy | Pain localized to the Achilles tendon or its insertion on the back of the heel, not the bottom. Often associated with calf tightness. |
| Systemic Inflammatory Conditions | Conditions like ankylosing spondylitis, reactive arthritis, or psoriatic arthritis can cause enthesitis (inflammation where tendons/ligaments attach to bone) at the plantar fascia insertion. Often associated with other joint/systemic symptoms. |
| Lumbar Radiculopathy (S1) | Nerve root irritation in the lower back can sometimes refer pain to the heel. Often associated with back pain, sciatica, or neurological changes in the leg/foot. |
References
- Thomas JL, Christensen JC, Kravitz SR, et al. The diagnosis and treatment of plantar fasciitis. J Foot Ankle Surg. 2010;49(3 Suppl):S1-S19. doi:10.1053/j.jfas.2010.04.001 (Clinical Practice Guideline)
- Buchbinder R. Plantar fasciitis. N Engl J Med. 2004;350(21):2159-2166. doi:10.1056/NEJMcp032745
- Latt LD, Jaffe DE, Tang Y, Taljanovic MS. Evaluation and Treatment of Chronic Plantar Fasciitis. Foot Ankle Orthop. 2020;5(1):2473011419896763. doi:10.1177/2473011419896763
- Neufeld SK, Cerrato R. Plantar fasciitis: evaluation and treatment. J Am Acad Orthop Surg. 2008;16(6):338-346. doi:10.5435/00124635-200806000-00006
- Osborne HR, Breidahl WH, Allison GT. Critical differences in the reliability of manual palpation, static measurements and imaging techniques in the diagnosis of plantar fasciitis. J Sci Med Sport. 2006;9(1-2):155-161. doi:10.1016/j.jsams.2006.03.016 (Discusses spur relationship)
- McNally EG, Shetty S. Plantar fascia: imaging diagnosis and guided treatment. Semin Musculoskelet Radiol. 2010;14(3):334-343. doi:10.1055/s-0030-1254531
- McPoil TG, Martin RL, Cornwall MW, et al. Heel pain--plantar fasciitis: clinical practice guidelines linked to the international classification of function, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38(4):A1-A18. doi:10.2519/jospt.2008.0302
- Tu P, Bytomski JR. Diagnosis of heel pain. Am Fam Physician. 2011;84(8):909-916. Available from: https://www.aafp.org/pubs/afp/issues/2011/1015/p909.html
See also
- Achilles tendon inflammation (paratenonitis, ahillobursitis)
- Achilles tendon injury (sprain, rupture)
- Ankle and foot sprain
- Arthritis and arthrosis (osteoarthritis):
- Autoimmune connective tissue disease:
- Bunion (hallux valgus)
- Epicondylitis ("tennis elbow")
- Hygroma
- Joint ankylosis
- Joint contractures
- Joint dislocation:
- Knee joint (ligaments and meniscus) injury
- Metabolic bone disease:
- Myositis, fibromyalgia (muscle pain)
- Plantar fasciitis (heel spurs)
- Tenosynovitis (infectious, stenosing)
- Vitamin D and parathyroid hormone