Osteoarthritis of the sacroiliac joint
- Anatomy of the Sacrum and Sacroiliac Joint (SIJ)
- Understanding Osteoarthritis of the Sacroiliac Joint
- Diagnosis of Sacroiliac Joint Osteoarthritis
- Treatment of Sacroiliac Joint Osteoarthritis
- Differential Diagnosis of Sacroiliac Region Pain
- Prevention and Lifestyle Management
- When to Consult a Specialist
- References
Anatomy of the Sacrum and Sacroiliac Joint (SIJ)
Development and Characteristics of the Sacrum
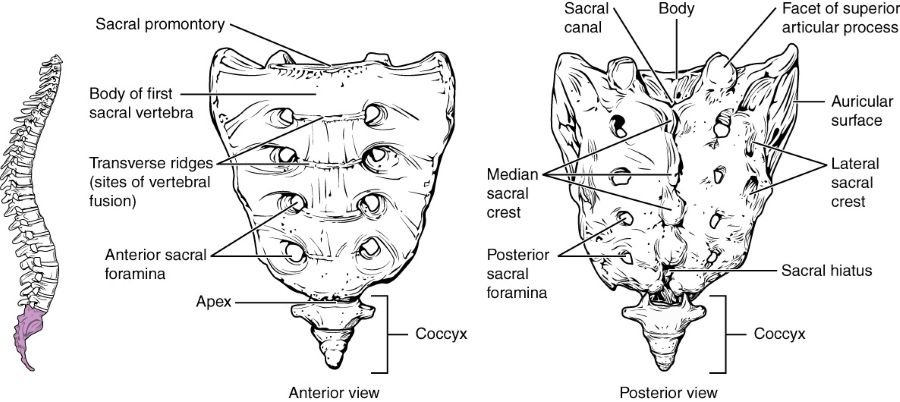
In adults, the sacrum is typically formed by the fusion of five sacral vertebrae (S1-S5). This fusion is a developmental process that occurs relatively late, generally between the ages of 18 and 25 years. The fusion usually begins after 15 years of age with the three lower sacral vertebrae (S3, S4, S5), and by approximately age 25, the two upper sacral vertebrae (S1, S2) also fuse to each other and to the lower segments, creating a single, solid sacral bone. Anatomically, the sacrum in males tends to be longer, narrower, and more significantly curved than in females; these differences are adaptations primarily related to the requirements of childbirth in the female pelvis.
In cases of incomplete fusion of the sacral vertebrae or associated congenital developmental anomalies—such as spina bifida, transitional vertebrae like sacralization (fusion of L5 to S1) or lumbarization (S1 behaving as an L6 vertebra)—splitting of the vertebral arch with or without the formation of a meningocele or meningomyelocele can be detected. The lateral surfaces of the sacrum feature prominent auricular (ear-shaped) articular surfaces. These articulate with corresponding auricular surfaces on the iliac bones of the pelvis on each side, forming the sacroiliac (SI) joints.
Posterior view of the sacrum, coccyx, and the sacroiliac joints, illustrating their anatomical relationship.
The Sacroiliac Joint Structure and Function
The sacroiliac joint (SIJ) is a complex, weight-bearing articulation. It is a diarthrodial-amphiarthrodial joint, meaning it has features of both a synovial joint (with a joint cavity and synovial fluid, primarily in its anterior part) and a syndesmosis (a fibrous joint with very limited movement, primarily in its posterior part). The SIJ is characterized by its inherent stability, provided by strong, interlocking, irregular articular surfaces and an extensive network of robust ligaments (including the anterior and posterior sacroiliac ligaments, interosseous sacroiliac ligament, sacrotuberous, and sacrospinous ligaments). This makes it a very rigid formation, often referred to as the sacroiliac junction, designed primarily for transferring loads between the spine and the lower limbs rather than for extensive motion. However, a small amount of rotational and translational movement does occur at the SIJ, which can be a source of pain if the joint is dysfunctional or diseased.
Understanding Osteoarthritis of the Sacroiliac Joint
Definition and Pathophysiology
Osteoarthritis (OA) of the sacroiliac joint (articulation), often referred to as sacroiliac joint arthrosis or degenerative sacroiliitis, is a chronic dystrophic (degenerative) process affecting the articular cartilage and underlying bone of the SIJ. It typically occurs against the background of, or as a consequence of, long-term mechanical stress, previous inflammation (e.g., resolved sacroiliitis of other causes), or impaired mobility (hypomobility or hypermobility) in the joint. OA involves the progressive loss of articular cartilage, formation of osteophytes (bone spurs), subchondral bone sclerosis (hardening), and sometimes cyst formation.
Causes and Risk Factors for SIJ Osteoarthritis
- Age: OA is more common with increasing age due to cumulative wear and tear.
- Mechanical Stress/Overload: Prolonged positional overload (e.g., from sedentary work, repetitive lifting, carrying heavy loads), leg length discrepancy, spinal deformities (scoliosis), or altered gait biomechanics.
- Trauma: Previous direct trauma to the pelvis or SIJ.
- Pregnancy and Childbirth: Hormonal changes leading to ligamentous laxity and altered biomechanics during pregnancy can stress the SIJs.
- Obesity: Increased weight places greater stress on weight-bearing joints like the SIJ.
- Previous Spinal Surgery: Particularly lumbar fusion, which can alter stress distribution to adjacent segments, including the SIJs (adjacent segment degeneration).
- Inflammatory Conditions: While distinct from inflammatory sacroiliitis (like in ankylosing spondylitis), previous resolved inflammation might predispose to later degenerative changes.
Clinical Symptoms and Pain Characteristics
The pain in the sacrum (sacrodynia) associated with osteoarthritis of the SIJ is often of a similar aching nature to that experienced by patients with inflammatory sacroiliitis. It can manifest as:
- Constant Heaviness and Discomfort: Particularly after exertion such as prolonged walking, sitting, or activities like dancing.
- Pain Location: Typically localized over the affected SIJ (buttock area), but can also refer pain to the lower back, groin, posterior thigh, and occasionally down the leg (pseudo-sciatica), usually not extending below the knee.
- Aggravating Factors: Pain often worsens with activities that load or stress the SIJ, such as transitioning from sitting to standing, climbing stairs, lying on the affected side, or impact activities.
- Relieving Factors: Pain may be relieved by rest or changing positions.
- Stiffness: Morning stiffness or stiffness after inactivity may be present, though usually less prolonged than in inflammatory spondyloarthropathies.
The pain associated with SIJ osteoarthritis can be intermittent, with periods of remission, and can re-escalate when the joint is overloaded or subjected to adverse conditions like overcooling (hypothermia).
This image displays the anatomy of the sacrum and sacroiliac joints in an adult. Osteoarthritis can develop in these joints due to long-term wear and tear or previous injury.
Diagnosis of Osteoarthritis of the Sacroiliac Joint
The diagnosis of osteoarthritis of the sacroiliac joint (articulation), similar to the diagnostic process for inflammatory sacroiliitis, involves a comprehensive evaluation. This includes a detailed examination of the patient, a thorough study of their medical history (anamnesis) regarding the onset and progression of the disease, and an assessment of biomechanical changes (such as gait abnormalities, alterations in muscle tone and strength, and the range of motion in the joints of the lower pelvic girdle).
Locally, with osteoarthritis of the sacroiliac joint, soreness and tenderness may be elicited upon palpation on the side of the inflamed or degenerated articulation.
Gynecological diseases affecting the pelvic organs in women can cause referred pain symptoms (sacrodynia) in the sacrum, which may mimic the pain of sacroiliac joint osteoarthritis. (Image illustrative of pelvic anatomy).
Blood tests in osteoarthritis of the sacroiliac joint typically do not show significant signs of systemic inflammation (e.g., Erythrocyte Sedimentation Rate - ESR, C-Reactive Protein - CRP are usually normal or only mildly elevated), unlike in inflammatory sacroiliitis. Radiography of the pelvic bones allows for the exclusion of traumatic injuries to the sacroiliac joint and conditions like osteomyelitis in the patient.
Computed tomography (CT) of the lumbosacral spine and pelvic bones is valuable in diagnosing osteoarthritis of the sacroiliac joint. It can clearly demonstrate degenerative changes such as joint space narrowing, subchondral sclerosis, osteophyte formation, and subchondral cysts. CT also helps to differentiate degenerative changes from inflammatory sacroiliitis and allows for the exclusion of oncological causes for lesions affecting the pelvic bones or vertebral bodies in the patient. MRI can also show degenerative changes and is useful for assessing surrounding soft tissues and ruling out other pathologies, though CT is often superior for fine bony detail of arthrosis.
Computed tomography (CT) of the sacroiliac joint is instrumental in visualizing degenerative changes of osteoarthritis and makes it possible to exclude an oncological nature of lesions affecting the pelvic bones or vertebral bodies in a patient with SIJ symptoms.
Treatment of Osteoarthritis of the Sacroiliac Joint
The treatment of osteoarthritis of the sacroiliac joint (articulation), similar to the management of inflammatory sacroiliitis, aims to reduce pain, improve function, and slow down degenerative progression where possible. It often involves a multimodal approach.
Conservative Management Strategies
- Activity Modification: If possible, complete or partial restriction of excessive physical activity or prolonged postures that place stress on the sacroiliac joint is recommended. This includes avoiding activities that provoke pain.
- Supportive Measures: For unloading the lumbosacral region, especially in conditions like pregnancy where ligamentous laxity can exacerbate SIJ pain, a special maternity support belt or a sacroiliac belt can be used to provide external support and stability. It is advisable to restrict prolonged sitting or walking if these activities aggravate symptoms.
- Weight Management: For overweight or obese individuals, weight loss can significantly reduce stress on the SIJs.
Pharmacological Therapy
Drug therapy, similar to that for sacroiliitis, is prescribed depending on the severity of specific symptoms in a patient with osteoarthritis of the sacroiliac joint. Options include:
- Analgesics: Acetaminophen (paracetamol) is often a first-line analgesic.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Oral NSAIDs (e.g., ibuprofen, naproxen, diclofenac, celecoxib) or topical NSAID preparations (gels, creams) can be used to reduce pain and any associated inflammation.
- Glucocorticoids (Corticosteroids): Systemic glucocorticoids are generally not indicated for SIJ osteoarthritis. However, intra-articular corticosteroid injections are a key treatment modality (see below).
- Other Medications: For chronic pain, duloxetine or tricyclic antidepressants may sometimes be considered.
In the treatment of osteoarthritis of the sacroiliac joint, physiotherapy helps to eliminate swelling (puffiness) and inflammation, alleviate soreness, and restore the volume of movement in the affected joint and the muscles of the lower back and buttocks, thereby accelerating recovery.
Interventional Pain Management (Injections)
If there is significant pain (sacrodynia) in a patient with arthrosis of the sacroiliac joint (articulation) that is unresponsive to oral medications and physical therapy, targeted injections can be performed:
- Sacroiliac Joint Injections: Under imaging guidance (fluoroscopy or ultrasound), a local anesthetic (e.g., lidocaine) and a corticosteroid (e.g., hydrocortisone, Diprospan/betamethasone, Kenalog/triamcinolone) are injected directly into the SIJ. This can provide significant diagnostic information (if pain is relieved) and therapeutic benefit by reducing inflammation and pain.
- Periarticular Ligament/Trigger Point Injections: If pain is thought to arise from surrounding ligaments or myofascial trigger points.
- Radiofrequency Ablation (RFA) / Neurotomy: For chronic SIJ pain that responds well but transiently to diagnostic blocks, RFA of the sensory nerves (lateral branches of the sacral dorsal rami) innervating the SIJ can provide longer-lasting pain relief (months to over a year).
Manual Therapy and Physiotherapy
- Manual Therapy: This is a mandatory component if the patient has no other contraindications. Techniques such as SIJ mobilization or manipulation, muscle energy techniques, and myofascial release can help improve regional blood circulation, restore lost range of motion in the affected SIJ, and address compensatory dysfunctions in the lumbar spine and hips.
- Physiotherapy (Physical Therapy): In addition to exercises, specific physical modalities are prescribed for the side of the inflamed sacroiliac joint. These can include:
- Heat or cold therapy.
- TENS (Transcutaneous Electrical Nerve Stimulation).
- Ultrasound.
- UHF (Ultra-High Frequency) therapy.
- Infrared radiation therapy.
- Acupuncture: May be used as an adjunctive therapy for pain relief.
Supportive Measures (Bracing)
Wearing a semi-rigid lumbosacral brace or, more specifically, a sacroiliac belt helps to limit the amount of movement in the sacroiliac joint. This support can reduce pain in the area of SIJ inflammation/degeneration and relieve excessive protective tension and spasm of the muscles of the back and buttock area. In such a brace, the patient can often move more independently at home and on the street, sit in a car, and manage tasks at their workplace. The need for a corset or SI belt typically diminishes as the pain in the sacrum subsides. Various types of lumbosacral semi-rigid corsets and SI belts are available, all selected according to size and usable repeatedly for recurrent sacral pain.
Wearing a lumbosacral or specific sacroiliac belt can be helpful in the treatment of pain in the sacrum due to sacroiliitis and arthrosis of the sacroiliac joint (articulation), and can be particularly beneficial for providing support and pain relief for pregnant women experiencing SIJ discomfort.
This image shows a variant of a semi-rigid lumbosacral brace, which can help in the treatment of pain localized to the sacrum (sacrodynia) by providing external support.
Surgical Treatment (e.g., SIJ Fusion)
Surgical treatment for primary osteoarthritis of the sacroiliac joint is reserved for a small subset of patients with severe, debilitating chronic pain that has failed to respond to comprehensive conservative and interventional pain management strategies for at least 6-12 months, and where the SIJ has been definitively identified as the primary pain generator through diagnostic blocks. The most common surgical procedure is **sacroiliac joint fusion (arthrodesis)**, which aims to eliminate motion at the painful joint by promoting bony fusion across it. This can be performed using open techniques or, more commonly now, minimally invasive surgical (MIS) approaches with implantation of devices like threaded cages or screws across the joint.
Differential Diagnosis of Sacroiliac Region Pain
Pain in the SIJ region can arise from various sources, requiring careful differentiation:
| Condition | Key Differentiating Features |
|---|---|
| Osteoarthritis of Sacroiliac Joint | Chronic, aching pain over SIJ/buttock, worse with activity/prolonged positions. Imaging shows degenerative changes (joint space narrowing, osteophytes, sclerosis). Inflammatory markers usually normal. |
| Inflammatory Sacroiliitis (e.g., Ankylosing Spondylitis) | Inflammatory back/buttock pain, morning stiffness >30 min, improves with exercise. MRI shows active inflammation (bone marrow edema). HLA-B27 often positive. Systemic features. |
| Lumbar Disc Herniation with Radiculopathy (L5/S1) | Radiating leg pain (sciatica) in dermatomal pattern, numbness, weakness. Positive SLR. MRI shows disc herniation. SIJ exam may be normal. |
| Lumbar Facet Joint Syndrome | Low back pain, may refer to buttock/thigh (rarely below knee). Worse with extension/twisting. Tenderness over lumbar facets. |
| Piriformis Syndrome / Gluteal Myofascial Pain | Buttock pain, may mimic sciatica. Tenderness over piriformis or gluteal trigger points. Pain with specific muscle stretch/contraction. |
| Hip Joint Pathology (e.g., Osteoarthritis) | Groin pain, lateral hip pain, pain with hip movements. Can refer to buttock or thigh. |
Prevention and Lifestyle Management
While age-related degeneration cannot be entirely prevented, certain measures can help manage symptoms and potentially slow progression of SIJ osteoarthritis:
- Weight Management: Maintaining a healthy weight reduces stress on the SIJs.
- Regular Low-Impact Exercise: Activities like swimming, walking, and cycling can maintain joint mobility and muscle strength without excessive stress. Core and hip strengthening exercises are particularly important.
- Proper Body Mechanics and Posture: Avoiding activities or postures that strain the SIJs.
- Supportive Footwear: Can improve overall lower limb biomechanics.
When to Consult a Specialist
Consultation with a physician (e.g., general practitioner, rheumatologist, orthopedic specialist, physiatrist, or pain management specialist) is recommended if:
- Pain in the lower back, buttock, or sacral region is persistent, severe, or disabling.
- Pain is associated with morning stiffness, improves with activity, or has other inflammatory features.
- There is a history of trauma to the pelvis or lower back.
- Symptoms significantly impact daily functioning or sleep.
- Conservative self-care measures fail to provide relief.
An accurate diagnosis is essential for developing an effective treatment plan tailored to the individual's specific condition and underlying cause of SIJ pain.
References
- Cohen SP, Chen Y, Neff N. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2013 Mar;116(3):695-710.
- Ou-Yang DC, York PJ, Kleck CJ, Patel VV. Diagnosis and Management of Sacroiliac Joint Dysfunction. J Bone Joint Surg Am. 2017 Oct 18;99(20):1767-1776.
- Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012 Dec;221(6):537-67.
- Bernard TN, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop Relat Res. 1987 Mar;(217):266-80.
- Hansen HC, McKenzie-Brown AM, Cohen SP, et al. Sacroiliac joint interventions: a systematic review. Pain Physician. 2007 Jan;10(1):165-84.
- Sembrano JN, Polly DW Jr. Sacroiliac joint pain. A meta-analysis. Global Spine J. 2013 Sep;3(3):147-52.
- Laslett M. Evidence-based diagnosis and treatment of the painful sacroiliac joint. J Man Manip Ther. 2008;16(3):142-52.
- Polly DW. The Sacroiliac Joint. Neurosurg Clin N Am. 2017 Jul;28(3):303-313.
See also
- Anatomy of the spine
- Ankylosing spondylitis (Bechterew's disease)
- Back pain by the region of the spine:
- Back pain during pregnancy
- Coccygodynia (tailbone pain)
- Compression fracture of the spine
- Dislocation and subluxation of the vertebrae
- Herniated and bulging intervertebral disc
- Lumbago (low back pain) and sciatica
- Osteoarthritis of the sacroiliac joint
- Osteocondritis of the spine
- Osteoporosis of the spine
- Guidelines for Caregiving for Individuals with Paraplegia and Tetraplegia
- Sacrodinia (pain in the sacrum)
- Sacroiliitis (inflammation of the sacroiliac joint)
- Scheuermann-Mau disease (juvenile osteochondrosis)
- Scoliosis, poor posture
- Spinal bacterial (purulent) epiduritis
- Spinal cord diseases:
- Spinal spondylosis
- Spinal stenosis
- Spine abnormalities
- Spondylitis (osteomyelitic, tuberculous)
- Spondyloarthrosis (facet joint osteoarthritis)
- Spondylolisthesis (displacement and instability of the spine)
- Symptom of pain in the neck, head, and arm
- Pain in the thoracic spine, intercostal neuralgia
- Vertebral hemangiomas (spinal angiomas)
- Whiplash neck injury, cervico-cranial syndrome