Osteochondrosis and Degenerative Disc Disease of the Spine
- Understanding Spinal Osteochondrosis and Degenerative Disc Disease (DDD)
- Neurological Syndromes Associated with Spinal Osteochondrosis and DDD
- Stages, Degrees, and Course of Spinal Osteochondrosis and DDD
- Spinal Osteochondrosis and DDD in Children and Adolescents
- Diagnosis of Spinal Osteochondrosis and Degenerative Disc Disease Symptoms
- Treatment of Symptoms Associated with Spinal Osteochondrosis and DDD
- Differential Diagnosis of Back Pain in the Context of Degenerative Spinal Changes
- Prevention and Lifestyle Management
- When to Consult a Specialist
- References
Understanding Spinal Osteochondrosis and Degenerative Disc Disease (DDD)
General Characteristics and Terminology
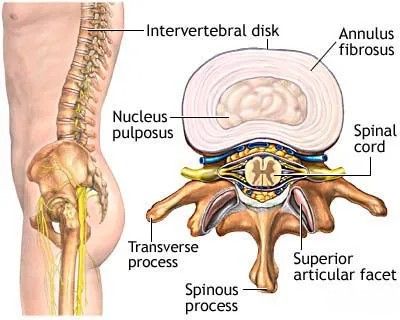
Spinal osteochondrosis is a term often used, particularly in some regions, to describe a degenerative-dystrophic disease process affecting the spine. This process primarily begins with degenerative changes in the intervertebral discs, which can subsequently lead to damage and secondary changes in other spinal structures, including vertebral bodies, facet joints, and ligaments. Degenerative Disc Disease (DDD) is a more universally accepted term that specifically refers to the age-related or pathological changes occurring within the intervertebral discs, such as desiccation (loss of water content), fissuring of the annulus fibrosus, and loss of disc height. While osteochondrosis may encompass broader spinal changes, DDD is a core component of this degenerative cascade.
It's important to note that degenerative changes in the spine, often labeled as osteochondrosis or DDD, are very common with aging. Radiographic signs of these changes (e.g., disc space narrowing, osteophytes) can be detected in a large percentage of individuals aged 40 and older, many of whom may be asymptomatic. Therefore, the presence of such radiological findings does not automatically equate to a "disease" state. The disease manifests only when these degenerative changes lead to clinically significant symptoms, such as pain, neurological deficits, or functional impairment. If osteochondrosis or DDD is detected incidentally during an examination for other reasons and the patient is asymptomatic, it should not necessarily be classified as a disease requiring active treatment, but rather as an age-related or structural finding.
This image shows the basic anatomy of a vertebra and an intervertebral disc, highlighting its components: the central nucleus pulposus and the surrounding annulus fibrosus. These structures are primarily affected in osteochondrosis and degenerative disc disease.
Spinal osteochondrosis/DDD is essentially a pathological process that *can* become a disease in the presence of appropriate clinical manifestations. Modern imaging methods, primarily Computed Tomography (CT of the spine) and Magnetic Resonance Imaging (MRI of the spine), can reveal some degree of degenerative changes in the spine in most adults, even healthy ones. The cervical and lumbar regions of the spine are most commonly affected due to their higher mobility and greater susceptibility to mechanical stress and overload, whereas the thoracic spine is relatively protected and stabilized by the rib cage and sternum.
Interestingly, it should be noted that in 60-75% of cases of radiologically confirmed spinal osteochondrosis, even with "prolapsed" or herniated lumbar discs, individuals may experience no pain or other symptoms. There is also no strict linear relationship between the radiographic degree of intervertebral disc dystrophy (degeneration) and the severity of neurological disorders. Moreover, in elderly and senile individuals, in whom the frequency and prevalence of advanced spinal osteochondrosis reach their maximum, lumbosacral radiculitis (sciatica) occurs 1.5-2 times less often than in middle-aged people, suggesting complex interactions between degeneration, inflammation, and symptom generation.
Pathophysiology and Etiological Factors
Various aspects of spinal osteochondrosis and its neurological manifestations in adults have been described in detail in numerous monographs, reference books, manuals, and countless journal articles. While only a few monographs are specifically devoted to the clinical manifestations of lumbar osteochondrosis in children and adolescents, this problem in younger age groups remains an area of ongoing study. Therefore, a detailed description of all causes and mechanisms of osteochondrosis development is beyond the scope here, but key concepts are well known to neurologists, neurosurgeons, and orthopedists, although much remains to be fully understood, and some aspects are still controversial.
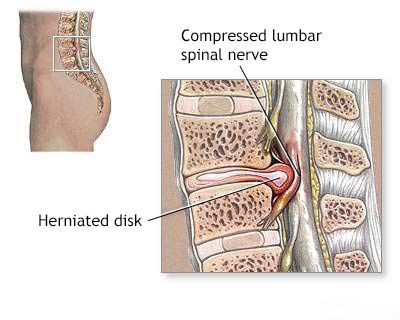
This image depicts the compression of a spinal nerve root by a herniated intervertebral disc, a common consequence of advanced spinal osteochondrosis.
Spinal osteochondrosis is considered a multifactorial disease, with contributions from:
- Hereditary and Congenital Traits: Genetic predisposition to disc degeneration or certain spinal anatomical variations.
- Acquired Factors:
- Static-Dynamic Loads: Mechanical stress from posture, occupational activities, trauma, and repetitive movements.
- Metabolic Changes: Alterations in disc nutrition and cellular metabolism.
- Vascular Factors: Some theories propose that an initial triggering mechanism of spinal osteochondrosis is vascular (ischemic). Pathomorphological data have shown a correlation between a decrease in the total area of the orifices of lumbar and median sacral arteries and an increase in osteochondrosis throughout the lumbar spine. A high frequency of developmental anomalies in vessels supplying lumbar segments (e.g., abnormal origin, multiple bends, narrowing) has also been revealed, potentially leading to insufficient blood supply to lumbar vertebrae and an imbalance between synthesis and destruction of crucial functional components of the intervertebral disc.
- Venous Outflow Impairment: In the pathogenesis of neurological manifestations of lumbar osteochondrosis, violation of venous outflow with partial or complete blockage of epidural veins at the level of a disc protrusion or herniation plays an important role. This can lead to venous congestion and edema. Detection of such venous disorders was historically based on specialized paraclinical studies like rheocaudospondylography, rheovasography, radiculography, and venospondylography. These findings historically prompted consideration of therapies targeting regional venous hemodynamics and cautioned against widely used thermal procedures that might worsen venous congestion.
The Role of Autoimmune Processes
Among the various etiological factors of spinal osteochondrosis and its neurological manifestations, autoimmune disorders are thought to play a leading role in the pathogenesis for some researchers. These autoimmune responses are believed to arise secondary to biochemical changes within the intervertebral discs (e.g., exposure of normally sequestered nucleus pulposus antigens) due to an imbalance between the processes of biosynthesis and the destruction of key functional components of connective tissue.
The autoimmune concept of spinal osteochondrosis pathogenesis and its clinical manifestations suggests that with neurological involvement (e.g., lumbar osteochondrosis with radiculopathy), the function of T- and B-systems of immunity can be impaired. This may manifest as increased production of autoantibodies against various structures of the intervertebral discs, potentially as a result of a deficiency in T-suppressor cells. These and other related data have been used to explain many mechanisms underlying the development of spinal osteochondrosis, including the staged progression of morphological changes in intervertebral discs, the characteristic alternation of remissions and relapses, and reactive inflammatory changes in nerve roots and surrounding tissues (e.g., epidural inflammation).
When assessing the role of autoimmune disorders in spinal osteochondrosis, it should also be borne in mind that autoimmune responses can be a universal reaction of the body to damage in any organ or tissue, not necessarily the primary driver of the degenerative process itself.
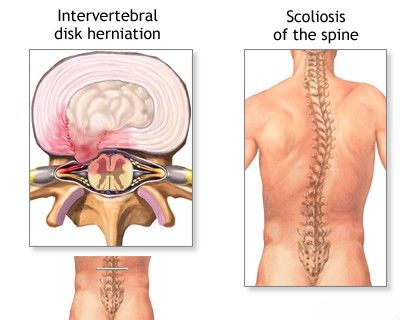
Antalgic scoliosis of the spine, accompanied by a protective spasm of the back muscles, is a common finding in patients with an acute hernia or protrusion of an intervertebral disc.
Neurological Syndromes Associated with Spinal Osteochondrosis and Degenerative Disc Disease
The neurological syndromes resulting from spinal osteochondrosis and DDD are clinically categorized based on the affected region of the spine. These syndromes arise primarily from mechanical compression or irritation of neural structures (nerve roots, spinal cord) by degenerated or displaced disc material, osteophytes, or hypertrophied ligaments, as well as from secondary inflammatory responses.
Common syndromes include:
- Cervical Spine Osteochondrosis/DDD Syndromes:
- Neck pain (cervicalgia).
- Cervical radiculopathy: Pain, numbness, tingling, and/or weakness radiating into the shoulder, arm, forearm, or hand in a dermatomal/myotomal pattern due to nerve root compression (e.g., by a herniated cervical disc or foraminal stenosis).
- Cervical myelopathy: Spinal cord compression in the cervical region leading to gait disturbance, balance problems, clumsiness in hands, weakness, spasticity, and sometimes bowel/bladder dysfunction.
- Cervicogenic headaches: Headaches originating from cervical spine structures.
- Vertebrobasilar insufficiency symptoms (e.g., dizziness, vertigo) if vertebral arteries are compressed by osteophytes.
- Thoracic Spine Osteochondrosis/DDD Syndromes:
- Mid-back pain (dorsalgia).
- Thoracic radiculopathy: Band-like pain radiating around the chest or upper abdomen (intercostal neuralgia) due to thoracic nerve root compression (less common than cervical or lumbar radiculopathy).
- Thoracic myelopathy: Rare, but can occur with large central disc herniations or severe spinal stenosis in the thoracic region.
- Lumbar Spine Osteochondrosis/DDD Syndromes:
- Low back pain (lumbago if acute, lumbodynia if chronic).
- Lumbar radiculopathy (sciatica): Pain, numbness, tingling, and/or weakness radiating from the lower back down the buttock, posterior or lateral thigh, calf, and into the foot, due to compression of lumbosacral nerve roots (commonly L4, L5, S1).
- Neurogenic claudication: Leg pain, numbness, or weakness brought on by walking or standing and relieved by sitting or bending forward, often due to lumbar spinal stenosis.
- Cauda equina syndrome: A serious condition caused by severe compression of the cauda equina nerve roots, resulting in bilateral leg weakness, saddle anesthesia, and bowel/bladder dysfunction (a neurosurgical emergency).
Stages, Degrees, and Course of Spinal Osteochondrosis and Degenerative Disc Disease
The progression of spinal osteochondrosis and DDD can be described in terms of stages of disc degeneration, radiographic severity, and the clinical course of symptoms.
Stages of Osteochondrosis (Disc Degeneration Pathophysiology)
While various staging systems exist, a common conceptualization of the degenerative cascade includes:
- Initial Stage (Dysfunction): Characterized by early biochemical changes within the disc (e.g., loss of proteoglycans, decreased water content in the nucleus pulposus), leading to altered disc mechanics and minor annular tears. Symptoms may be absent or mild and intermittent.
- Stage of Instability / Rupture of Annulus Fibrosus: Further degeneration leads to weakening and more significant tearing of the annulus fibrosus. This can result in disc bulging (protrusion), where the annulus remains intact but stretched, or disc herniation (prolapse/extrusion), where the nucleus pulposus breaks through the annulus. This stage is often associated with increased abnormal motion at the spinal segment (instability) and symptomatic episodes of pain or radiculopathy.
- Stage of Restabilization / Outcome and Residual Effects: Over time, with progressive disc height loss, osteophyte formation (bone spurs), and facet joint arthropathy, the affected spinal segment may become stiffer and relatively "restabilized," though often in a degenerated state. Symptoms may decrease in some individuals at this stage, but chronic pain or residual neurological deficits can persist. This stage represents the long-term outcome of spinal osteochondrosis, which can include spondylosis, spondyloarthrosis, and spinal stenosis.
Radiographic Severity of Osteochondrosis
The severity of osteochondrosis of the spine as observed on X-ray examination can be broadly graded based on features such as:
- Mild: Straightening of normal spinal curvatures (e.g., lumbar lordosis), slight flattening or reduction in height of the intervertebral disc, presence of small osteophytes (exostoses) at vertebral body margins, minor proliferation of uncinate processes (in the cervical spine).
- Moderate: A slight narrowing of the intervertebral foramina and the spinal canal, more noticeable decrease in the height of intervertebral discs, signs of spinal instability (e.g., minor spondylolisthesis on functional views).
- Severe: Significant narrowing of the intervertebral foramina and the spinal canal, marked disc height loss, large osteophytes, significant degenerative spondylolisthesis, or advanced facet joint arthropathy.
The Pfirrmann classification for MRI provides a more detailed grading of disc degeneration itself.
Clinical Course Types
The clinical course of symptomatic spinal osteochondrosis and DDD can vary:
- Recurrent Course: Characterized by intermittent episodes of pain or neurological symptoms, with periods of complete or near-complete remission in between.
- Chronically Recurrent Course: Similar to recurrent, but with more frequent exacerbations or shorter remission periods.
- Chronic Progressive Course: Symptoms are persistent and gradually worsen over time.
- Chronic Stable Course: Symptoms are persistent but remain relatively stable in intensity without significant progression.
Periods of the Disease Course
The clinical course can also be described in terms of distinct periods:
- Debut: The initial onset of symptoms.
- Exacerbation (Relapse): A period of worsening or reappearance of symptoms after a period of improvement.
- Remission: A period during which symptoms are absent (complete remission) or significantly reduced (incomplete remission).
- Period of Relative Stabilization / Residual Period: A later stage where acute inflammatory processes may have subsided, but chronic pain or residual neurological deficits due to structural changes may persist.
Spinal Osteochondrosis and Degenerative Disc Disease in Children and Adolescents
For a long time, there was a prevailing opinion that osteochondrosis of the spine primarily develops in adulthood and old age. Even in specialized manuals on nervous diseases, the possibility of vertebrogenic (spine-related) lesions of the nervous system in childhood and adolescence was often not mentioned at all or was discussed very briefly.
Historical Perspectives and Etiological Theories
The first mentions of the possibility of herniated lumbar intervertebral discs in adolescents date back to the mid-20th century. F. Jelsma (1944) reported a 17-year-old boy among 150 operated patients. In 1946, N. Wahren provided a detailed description of a prolapsed lumbosacral disc in a 12-year-old girl. Similar data were presented later by other authors. J.H. Webb, H.J. Svien, and R.L.J. Kennedy (1954) reported results of surgical treatment for prolapsed lumbar discs in 3 children and 57 adolescents. By 1974, the total number of such operations in children and adolescents reported in the literature was 158 (S.E. Borgesen, P.S. Vang, 1974), with 71 cases in patients under 15 described between 1946-1981.
There are different viewpoints regarding the reasons for the development of spinal osteochondrosis in childhood and adolescence. One factor considered is the peculiarity of blood supply to the intervertebral discs. It is known that the disc is fed by diffusion from the vertebral endplates, as its direct vessels typically regress after the age of 4 years. However, this age-related tissue rearrangement does not inherently mean pathology. Great importance is often attached to increased muscle load, overwork (micro- and macrotraumatization), especially during sports competitions. However, it is unlikely that trauma alone can cause a previously healthy disc to "prolapse." Studies by J. A. Key (1950), S.E. Borgessen & P.S. Vang (1974), and D. Jaster (1974) indicated that the frequency of trauma in the history of children and adolescents with disc issues does not significantly differ from that in adults. This suggests that disc dystrophy (degeneration) may be primary, with injury only accelerating its prolapse. The role of congenital inferiority or weakness of intervertebral disc tissues has also been indicated (P. Rottgen, 1951).
According to I.E. O'Connell (1960), the rapid skeletal growth experienced during childhood and adolescence itself acts as a stressor that can contribute to the degeneration of intervertebral discs. This author also considered muscular inadequacy, found in 10% of examined patients, as a second etiological factor. This was manifested in some patients with spinal osteochondrosis being very tall or, conversely, having an adipose (overweight) physique, or having weakened muscles after prolonged bed rest due to various illnesses.
Dysplastic Signs and Hereditary Factors
With increasing study of spinal osteochondrosis and its resulting neurological disorders, more and more importance is being given to hereditary factors. Khodosovskaya and Okuyeva (1980) conducted a genealogical study in 68 children and adolescents aged 8 to 18 years with various clinical manifestations of osteochondrosis. They found that 69.1% of the probands (the individuals initially studied) had family cases of the disease: parents, grandparents, uncles, and aunts suffered from similar conditions. In contrast, hereditary burden in adults with similar conditions was noted in 53.3% of cases, significantly lower than in the pediatric and adolescent group. It was also shown that if both parents were affected, lumbosacral pain in the proband tended to occur at a younger age.
Various dysplastic signs (minor physical anomalies suggestive of connective tissue or developmental variations) were also identified in 75% of pediatric and adolescent patients with reflex and radicular syndromes of vertebral lesions of lumbosacral localization, which is significantly higher than in adults (49%). These developmental anomalies manifested as:
- Mild facial dysmorphias (28%)
- Deviations in the structure of hands and feet (47%)
- Anomalies in the development of the muscular system (8.8%)
- Asymmetry of body structure (63%)
- Skin and vascular anomalies (23.5%)
In addition, 40.9% of the examined children and adolescents had congenital anomalies of the lumbosacral spine itself:
- Splitting of the vertebral arch (spina bifida occulta) (19.7%)
- Transitional lumbosacral vertebra (lumbarization or sacralization) (14.6%)
- Violation of tropism (asymmetry) of the articular processes (facet joints) (5.7%)
- Spondylolisthesis (0.8%)
In most cases (60%), there was a combination of two or more different dysplastic signs, a rate significantly higher than in adults (10%). When examining the relatives of these probands, such anomalies were also quite common: foot deformities, birthmarks, dilatation of saphenous veins, irregular body structure, facial dysmorphia, and a family history of bony anomalies of the lumbosacral spine were also traced. It should be noted that the precise role of these latter bony anomalies in the occurrence of lumbar osteochondrosis and its clinical manifestations has not been definitively established.
There is an opinion that congenital structural changes, under the influence of various exogenous factors (like mechanical stress), can cause static inferiority or biomechanical compromise of the spine, thereby contributing to the development of a dystrophic process in the intervertebral discs, particularly those adjacent to an anomaly. These data collectively indicate a significant role for hereditary predisposition in the development of neurological manifestations of lumbar osteochondrosis. This predisposition can potentially be transmitted in both an autosomal dominant and autosomal recessive manner.
The presence of familial cases of vertebrogenic diseases of the lumbosacral part of the peripheral nervous system, coupled with a high frequency of dysplastic signs in probands and their relatives (primarily involving the lumbosacral spine), suggests a heightened possibility of developing osteochondrosis of the lumbar spine and its clinical manifestations during childhood and adolescence, often earlier or more severely than in individuals without such predisposing factors.
Diagnosis of Symptoms of Spinal Osteochondrosis and Degenerative Disc Disease
The diagnosis of symptomatic spinal osteochondrosis and DDD begins with a comprehensive clinical evaluation, including a detailed neurological and orthopedic examination performed by a physician. During this examination, the patient's neurological status is assessed (motor strength, sensation, reflexes), and possible disturbances in spinal biomechanics are identified, with a mandatory evaluation of the condition of the back and gluteal muscles (tone, tenderness, trigger points). Often, at this initial stage of the study, a patient presenting with spinal osteochondrosis and associated back and lower back pain can receive a presumptive diagnosis, and initial treatment can be planned.
Based on the results of this clinical examination, if further clarification is needed, or if "red flag" symptoms are present, the following additional diagnostic procedures may be prescribed:
- Radiography (X-rays) of the Lumbosacral Spine: Often includes functional tests (flexion and extension views) to assess for spinal instability, spondylolisthesis, disc space narrowing, osteophyte formation (spondylosis), and facet joint arthropathy.
- CT Scan of the Lumbosacral Spine: Provides excellent detail of bony structures, useful for evaluating complex fractures, severe degenerative bone changes (e.g., facet hypertrophy leading to spinal stenosis), or assessing bone fusion after surgery. Can also show calcified disc herniations.
- MRI of the Lumbosacral Spine: The gold standard for visualizing soft tissues, including intervertebral discs (hydration, degeneration, protrusions, herniations, sequestrations), the spinal cord and cauda equina (for compression), nerve roots, ligaments, and detecting inflammation (e.g., discitis, spondylitis, sacroiliitis) or tumors.
- Electromyography (EMG) and Nerve Conduction Studies (NCS): May be used to confirm nerve root damage (radiculopathy) by identifying signs of denervation in muscles or slowed nerve conduction, and to differentiate it from peripheral neuropathy.
A sagittal view from a Magnetic Resonance Imaging (MRI) scan of the lumbosacral spine in a patient with osteochondrosis, illustrating degenerative changes such as disc height loss and altered disc signal.
Treatment of Symptoms Associated with Spinal Osteochondrosis and DDD
The treatment approach for back and lower back pain related to spinal osteochondrosis, disc herniation, or disc protrusion depends on the severity of symptoms, the underlying cause, the presence of neurological deficits, and the patient's overall condition. A multimodal, often conservative-first, strategy is typically employed.
Conservative Management Strategies
- Pharmacological Therapy:
- NSAIDs (Nonsteroidal Anti-Inflammatory Drugs): To reduce pain and inflammation (e.g., ibuprofen, naproxen, diclofenac).
- Analgesics: Acetaminophen or, for more severe acute pain, short-term use of opioid analgesics under strict medical supervision.
- Muscle Relaxants: To alleviate painful muscle spasms (e.g., cyclobenzaprine, tizanidine).
- Neuropathic Pain Medications: For radicular pain (sciatica), drugs like gabapentin, pregabalin, or certain antidepressants (e.g., tricyclics, SNRIs) may be prescribed.
- Hormones (Corticosteroids): Short courses of oral corticosteroids (e.g., prednisone) may be used for severe acute inflammation and radiculopathy. Epidural steroid injections are a more targeted approach (see below).
- Activity Modification and Rest: Relative rest during acute severe pain, avoiding activities that aggravate pain. Prolonged bed rest is generally not recommended. Gradual return to activity is encouraged.
- Patient Education: Understanding the condition, proper body mechanics, lifting techniques, and self-management strategies.
Interventional Pain Management
Therapeutic injections (blockades) with local anesthetics and/or corticosteroid medications can provide significant pain relief and reduce inflammation, accelerating recovery. These are often performed under imaging guidance (fluoroscopy or ultrasound) for accuracy:
- Epidural Steroid Injections: Medication is injected into the epidural space around the spinal nerve roots to reduce inflammation associated with disc herniations or spinal stenosis.
- Facet Joint Injections: Medication is injected into or around the facet (zygapophyseal) joints if facet joint arthropathy is suspected as the pain source. Low doses of anesthetic (e.g., novocaine/procaine, lidocaine) and a corticosteroid (e.g., cortisone, diprospan/betamethasone, Kenalog/triamcinolone) are typically used.
- Selective Nerve Root Blocks: Medication is injected around a specific spinal nerve root to diagnose and treat radicular pain.
- Trigger Point Injections: Injection of local anesthetic, sometimes with a corticosteroid, into painful trigger points within muscles.
- Sacroiliac Joint Injections: If sacroiliitis or sacroiliac joint arthrosis is the cause of pain.
When combined with a properly selected physiotherapy regimen, these therapeutic blocks can have a good and long-term effect on lumbar and sacral pain (sacrodynia), particularly in cases of herniated discs or disc protrusions in patients with degenerative disc disease.
Manual Therapy and Physiotherapy
- Manual Therapy: Techniques performed by trained therapists, such as spinal mobilization or manipulation, soft tissue mobilization (massage), and specific muscle energy or radicular techniques, can help relieve pain, reduce muscle spasm, and improve joint mobility. A non-surgical "reduction" of a vertebral disc herniation using these methods may be attempted by some practitioners, focusing on restoring biomechanics and decompressing affected structures.
- Physiotherapy (Physical Therapy): A cornerstone of low back pain management. Includes:
- Exercise Therapy: Specific exercises to strengthen core muscles (abdominal, paraspinal), improve flexibility, and promote proper posture (e.g., McKenzie exercises, dynamic lumbar stabilization).
- Modalities: Application of heat, cold, ultrasound, SMT (Segmental Massage Therapy - likely referring to a specific regional technique), TENS (Transcutaneous Electrical Nerve Stimulation), or UHF (Ultra-High Frequency) therapy to alleviate pain and muscle spasm.
- Education: On body mechanics, ergonomics, and self-management strategies.
Soft muscle techniques, a form of manual therapy, can be effective in relieving muscle spasms and associated pain in the lumbar region.
Supportive Measures (e.g., Bracing)
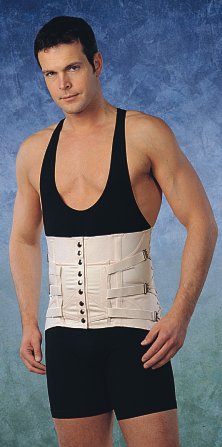
Wearing a semi-rigid lumbosacral corset during the treatment of back and lower back pain associated with spinal osteochondrosis, especially when there is a herniated disc or a protrusion of the intervertebral disc, can help to limit painful range of motion in the lumbar spine. This primarily aids in reducing pain in the area of inflamed intervertebral joints and relieving excessive protective tension and spasm of the back muscles. In such a corset, a patient with spinal osteochondrosis can often move independently at home and outdoors, and even sit in a car or at their workplace. The need to wear a brace typically diminishes as the back pain subsides. However, it is important to remember that during periods of acute exacerbation of back and lower back pain, excessive workloads should be avoided, and rest should be observed. This temporary restriction, combined with ongoing treatment, can significantly shorten recovery time and help prevent further progression of the spinal disease. There are several types of semi-rigid lumbosacral braces, all selected individually by size. They can be used repeatedly in case of recurrent pain or for prevention during activities that might exacerbate pain.
This image shows a variant of a semi-rigid lumbosacral brace that helps in the treatment of back and lower back pain occurring against the background of spinal osteochondrosis when complicated by a herniated disc or a protrusion of the intervertebral disc.
This is another variant of a semi-rigid lumbosacral brace designed to assist in the treatment of back and lower back pain that arises from spinal osteochondrosis.
- Acupuncture (Reflexotherapy): Can be very effective in treating back and lower back pain associated with degenerative disc disease, disc herniation, or disc protrusion by modulating pain signals and promoting muscle relaxation.
The use of acupuncture is often very effective in the treatment of back and lower back pain associated with osteochondrosis of the spine when complicated by a herniated or protruding intervertebral disc.
In the treatment of pain radiating to the leg and buttock against the background of degenerative disc disease with a herniated disc or intervertebral disc protrusion, physiotherapy is essential for eliminating soreness and tingling, and restoring sensitivity in the leg affected by sciatic nerve neuritis due to its compression.
Surgical Treatment (When Indicated)
Surgical intervention is considered if conservative treatment fails to provide adequate relief after a reasonable period (typically 6-12 weeks), or if there are "red flag" signs such as progressive or severe neurological deficits, or cauda equina syndrome (a surgical emergency). Surgical options vary depending on the specific pathology but may include microdiscectomy, laminectomy, foraminotomy, or spinal fusion.
Differential Diagnosis of Back Pain in the Context of Degenerative Spinal Changes
It is important to differentiate pain stemming directly from osteochondrosis/DDD and disc herniation from other conditions that can cause or mimic low back pain, even if degenerative changes are present on imaging.
| Condition | Key Differentiating Features |
|---|---|
| Spinal Osteochondrosis / DDD with Disc Herniation | Axial back/neck pain, often with radicular pain (sciatica/brachialgia), numbness, weakness if nerve root compressed. MRI/CT shows disc degeneration, protrusion, extrusion, or sequestration. |
| Facet Joint Syndrome (Spondyloarthrosis) | Localized back/neck pain, often worse with extension or twisting. May refer pain to buttock/thigh (lumbar) or shoulder/head (cervical). No true radiculopathy. Tenderness over facet joints. |
| Spinal Stenosis | Neurogenic claudication (leg/buttock pain, numbness, weakness with walking/standing, relieved by flexion/sitting). May have back pain. MRI/CT shows canal narrowing. |
| Spondylolisthesis (Degenerative) | Low back pain, may have radicular symptoms or neurogenic claudication. Vertebral slippage on X-ray/CT/MRI. Often associated with advanced DDD. |
| Myofascial Pain Syndrome / Muscular Strain | Aching muscle pain, stiffness, trigger points. Often related to posture, overuse, or minor injury. Neurological exam usually normal. |
| Sacroiliac Joint Dysfunction | Pain over SI joint, buttock, groin, sometimes referring to posterior thigh. Positive SI joint provocative tests. Can coexist with lumbar DDD. |
| Inflammatory Spondyloarthropathies (e.g., Ankylosing Spondylitis) | Inflammatory back pain (morning stiffness, improves with exercise). Sacroiliitis on imaging. HLA-B27 positive. Systemic features. |
| "Red Flag" Conditions (Tumor, Infection, Fracture) | Persistent night pain, unexplained weight loss, fever, history of cancer/trauma. Require urgent investigation. |
Prevention and Lifestyle Management
While age-related degeneration is inevitable to some extent, certain measures can help prevent or slow the progression of symptomatic osteochondrosis and DDD:
- Maintaining a healthy body weight to reduce stress on the spine.
- Regular exercise focusing on core strength, flexibility, and cardiovascular fitness.
- Practicing good posture during sitting, standing, and daily activities.
- Using proper body mechanics for lifting and other physical tasks.
- Creating an ergonomic workspace.
- Avoiding smoking, as it impairs disc nutrition and healing.
- Adequate nutrition and hydration.
When to Consult a Specialist
Consultation with a neurologist, neurosurgeon, orthopedic spine specialist, or pain management physician is recommended if:
- Back or neck pain is severe, persistent (lasting more than a few weeks), or significantly impacts daily life.
- Pain radiates into the arms or legs, especially if accompanied by numbness, tingling, or weakness.
- There are "red flag" symptoms such as unexplained weight loss, fever, night pain, or bowel/bladder dysfunction (Cauda Equina Syndrome is a surgical emergency).
- Conservative self-care measures fail to provide adequate relief.
- There is a history of significant spinal trauma.
A specialist can conduct a thorough evaluation, including appropriate imaging, to establish an accurate diagnosis and develop a comprehensive, individualized treatment plan.
References
- Adams MA, Roughley PJ. What is intervertebral disc degeneration, and what causes it? Spine (Phila Pa 1976). 2006 Aug 15;31(18):2151-61.
- Fardon DF, Williams AL, Dohring EJ, et al. Lumbar disc nomenclature: version 2.0: Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J. 2014 Nov 1;14(11):2525-45.
- Bogduk N. Clinical anatomy of the lumbar spine and sacrum. 5th ed. Churchill Livingstone Elsevier; 2012.
- Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001 Sep 1;26(17):1873-8.
- Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014 Jan;14(1):180-91.
- Cohen SP, Argoff CE, Carragee EJ. Management of low back pain. BMJ. 2008 Dec 4;337:a2718.
- Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001 Feb 1;344(5):363-70.
- Videman T, Battié MC, Gibbons LE, Maravilla K, Manninen H, Kaprio J. Associations between back pain history and lumbar MRI findings. Spine (Phila Pa 1976). 2003 Mar 15;28(6):582-8. (Highlights discrepancy between imaging and symptoms)
See also
- Anatomy of the spine
- Ankylosing spondylitis (Bechterew's disease)
- Back pain by the region of the spine:
- Back pain during pregnancy
- Coccygodynia (tailbone pain)
- Compression fracture of the spine
- Dislocation and subluxation of the vertebrae
- Herniated and bulging intervertebral disc
- Lumbago (low back pain) and sciatica
- Osteoarthritis of the sacroiliac joint
- Osteocondritis of the spine
- Osteoporosis of the spine
- Guidelines for Caregiving for Individuals with Paraplegia and Tetraplegia
- Sacrodinia (pain in the sacrum)
- Sacroiliitis (inflammation of the sacroiliac joint)
- Scheuermann-Mau disease (juvenile osteochondrosis)
- Scoliosis, poor posture
- Spinal bacterial (purulent) epiduritis
- Spinal cord diseases:
- Spinal spondylosis
- Spinal stenosis
- Spine abnormalities
- Spondylitis (osteomyelitic, tuberculous)
- Spondyloarthrosis (facet joint osteoarthritis)
- Spondylolisthesis (displacement and instability of the spine)
- Symptom of pain in the neck, head, and arm
- Pain in the thoracic spine, intercostal neuralgia
- Vertebral hemangiomas (spinal angiomas)
- Whiplash neck injury, cervico-cranial syndrome