Meningovascular syphilis (tabes dorsalis)
- Understanding Neurosyphilis: Meningovascular Syphilis and Tabes Dorsalis
- Clinical Symptoms of Tabes Dorsalis (Locomotor Ataxia)
- Diagnosis of Meningovascular Syphilis and Tabes Dorsalis
- Treatment of Neurosyphilis (Including Tabes Dorsalis)
- Differential Diagnosis of Ataxia and Sensory Neuropathy
- Prognosis and Complications
- Prevention and When to Seek Medical Attention
- References
Understanding Neurosyphilis: Meningovascular Syphilis and Tabes Dorsalis
Overview and Historical Context
Neurosyphilis refers to infection of the central nervous system (brain and spinal cord) by the bacterium *Treponema pallidum*, the causative agent of syphilis. It can occur at any stage of syphilis. Meningovascular syphilis and tabes dorsalis are two distinct, though sometimes overlapping, manifestations of late (tertiary) neurosyphilis, typically developing years to decades after the initial infection if left untreated.
Since the advent and widespread use of penicillin, tabes dorsalis (also known as locomotor ataxia or syphilitic myelopathy) has become significantly less common than it was in the pre-penicillin era. However, the diagnosis of meningovascular syphilis and other forms of neurosyphilis should still be considered in the differential diagnosis of major neurological syndromes arising from diseases of the spinal cord or brain, especially in individuals with risk factors for syphilis or atypical neurological presentations.
Pathophysiology of Tabes Dorsalis
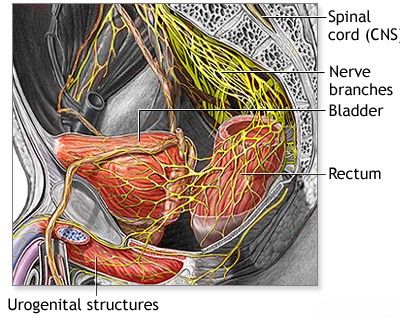
Tabes dorsalis is primarily characterized by slow, progressive degeneration of the posterior (dorsal) columns of the spinal cord, the dorsal roots, and dorsal root ganglia. These structures are crucial for transmitting sensory information, particularly proprioception (sense of position), vibration sense, and fine touch. Meningovascular syphilis, on the other hand, involves inflammation of the meninges and blood vessels of the brain and spinal cord ( syphilitic endarteritis), which can lead to strokes, cranial nerve palsies, and more diffuse neurological damage.
Clinical Symptoms of Tabes Dorsalis (Locomotor Ataxia)
The clinical manifestations of tabes dorsalis are diverse, reflecting the damage to the posterior columns and dorsal roots.
Sensory Symptoms: Pain and Paresthesias
- Lightning Pains: One of the most common and characteristic symptoms. These are sudden, brief, severe, stabbing, or shooting pains that occur recurrently. The legs are most frequently affected, with pains often described as "lumbago-like" or lancinating. Much less often, these pains can be felt by the patient in the face (mimicking trigeminal neuralgia), back, chest, abdomen, or arms.
- Paresthesias: Abnormal sensations such as numbness, tingling, burning, or a feeling of constriction ("girdle sensation" around the trunk) are noted in 15-30% of patients.
- Impaired Sensation: Loss or reduction of proprioception (joint position sense) and vibration sense are key features. Deep pain sensation may also be lost. Light touch sensation is often preserved longer.
Ataxia and Gait Disturbances
In approximately half of patients with tabes dorsalis, a significant gait disorder develops, characterized by sensory ataxia. This ataxia is caused by the loss of proprioception, particularly from the lower limbs.
- Wide-Based, Stomping Gait: Patients walk with a broad base, lifting their feet high and slapping them down forcefully (stomping) to try and gain sensory feedback from the ground.
- Instability: The imbalance is characteristically worsened when visual input is removed (e.g., when closing the eyes or in the dark), as the patient can no longer compensate visually for the loss of proprioceptive information. This is demonstrated by a positive Romberg test.
Autonomic and Visceral Symptoms
- Bladder Dysfunction: Urinary incontinence (overflow or urge), difficulty initiating urination, or a hypotonic, large-capacity bladder (tabetic bladder) are common.
- Sexual Dysfunction in Men: Erectile dysfunction and delayed ejaculation.
- Visceral Crises: Paroxysmal attacks of severe, acute abdominal pain, often accompanied by nausea and vomiting (gastric crises). Laryngeal or rectal crises can also occur.
- Trophic Changes: Due to sensory loss and autonomic dysfunction, patients may develop perforating ulcers on the feet (mal perforant), and Charcot joints (neurogenic arthropathy), which are painless, destructive joint deformities, most commonly affecting the knees and ankles.
Classic Neurological Signs
The most common objective neurological signs in tabes dorsalis include:
- Loss of Deep Tendon Reflexes: Particularly absence of the Achilles tendon reflex (ankle jerk) and patellar reflex (knee jerk) in the legs (Westphal's sign).
- Impaired Proprioception and Vibration Sense: Demonstrated by inability to determine joint position with eyes closed or perceive a vibrating tuning fork.
- Positive Romberg Test: Loss of balance when standing with feet together and eyes closed, indicating impaired proprioception.
- Pupillary Abnormalities:
- Argyll Robertson Pupil: A classic sign, though not exclusive to tabes dorsalis. It is characterized by small, irregular pupils that do not constrict in response to bright light (absent light reflex) but do constrict normally during accommodation (focusing on a near object). This is often described as "accommodation without reaction to light" or "prostitute's pupil" (accommodates but doesn't react). It is usually bilateral.
- Other pupillary changes like miosis (constricted pupils) or anisocoria (unequal pupil size) can also occur.
- Optic Atrophy: Can occur, leading to progressive visual loss.
- Hypotonia: Decreased muscle tone.
Diagnosis of Meningovascular Syphilis and Tabes Dorsalis
The diagnosis of neurosyphilis, including meningovascular forms and tabes dorsalis, is based on a combination of:
- Clinical Presentation: Characteristic neurological symptoms and signs as described above.
- Serological Tests for Syphilis:
- Non-treponemal tests (e.g., VDRL, RPR) on serum: Usually reactive in active syphilis, but can be non-reactive in late neurosyphilis (especially tabes dorsalis).
- Treponemal tests (e.g., FTA-ABS, TP-PA, EIAs) on serum: Usually remain reactive for life after infection and are more specific for confirming syphilis exposure.
- Cerebrospinal Fluid (CSF) Examination: This is crucial for diagnosing neurosyphilis. Findings suggestive of neurosyphilis include:
- Reactive CSF-VDRL: Highly specific for neurosyphilis, but not very sensitive (can be negative in many cases of active neurosyphilis, particularly tabes).
- CSF Pleocytosis: Increased white blood cell count (usually lymphocytic).
- Elevated CSF Protein: Indicates inflammation or damage to the blood-brain barrier.
- Positive CSF Treponemal Antibody Tests (e.g., CSF FTA-ABS or TP-PA): More sensitive than CSF-VDRL but can be positive due to passive transfer of antibodies from serum if the blood-brain barrier is compromised or due to past treated syphilis. Interpretation requires careful consideration of serum results and CSF integrity.
- Neuroimaging (MRI or CT of Brain and Spine): While often not diagnostic for tabes dorsalis itself (which primarily involves microscopic changes in the dorsal columns and roots), imaging can help rule out other causes of myelopathy or neurological symptoms. In meningovascular syphilis, MRI may show evidence of infarcts (strokes) or meningeal enhancement. Spinal MRI in tabes may show atrophy of the dorsal columns in advanced cases.
- Exclusion of Other Conditions: Differentiating from other causes of sensory ataxia, peripheral neuropathy, or myelopathy (see Differential Diagnosis section).
Treatment of Neurosyphilis (Including Tabes Dorsalis)
The primary goal of treating neurosyphilis, including tabes dorsalis and meningovascular syphilis, is to eradicate the *Treponema pallidum* infection and prevent further neurological progression. Unfortunately, existing neurological damage from tabes dorsalis is often irreversible.
- Penicillin Therapy: High-dose intravenous aqueous crystalline penicillin G is the treatment of choice for all forms of neurosyphilis. A typical regimen is 18-24 million units per day, administered as 3-4 million units IV every 4 hours or by continuous infusion, for 10-14 days.
- Alternative regimens for outpatients or those with penicillin allergy (after careful consideration and desensitization if possible) might include procaine penicillin G intramuscularly plus probenecid orally, or ceftriaxone. However, IV penicillin G is strongly preferred.
- Symptomatic Treatment:
- Pain Management: Lightning pains can be very difficult to treat. Medications like carbamazepine, gabapentin, pregabalin, or tricyclic antidepressants may provide some relief.
- Management of Ataxia: Physical therapy, balance exercises, and assistive devices (e.g., cane, walker) to improve gait and prevent falls.
- Bladder Dysfunction: Urological management, which may include intermittent catheterization or medications.
- Supportive Care: Management of trophic ulcers, Charcot joints, and other complications.
- Follow-up: Regular clinical follow-up and repeat CSF examinations (e.g., at 6-month intervals) are necessary to monitor treatment response (normalization of CSF cell count and protein, decline in CSF-VDRL titers if initially positive). Retreatment may be needed if CSF abnormalities do not improve.
Treatment is typically managed by infectious disease specialists and neurologists.
Differential Diagnosis of Ataxia and Sensory Neuropathy
The symptoms of tabes dorsalis, particularly sensory ataxia and peripheral sensory loss, can mimic other neurological conditions:
| Condition | Key Differentiating Features from Tabes Dorsalis |
|---|---|
| Vitamin B12 Deficiency (Subacute Combined Degeneration) | Posterior column dysfunction (loss of proprioception/vibration), peripheral neuropathy, possible corticospinal tract signs (spasticity, hyperreflexia initially, Babinski). Low serum B12, elevated methylmalonic acid/homocysteine. No Argyll Robertson pupils. Syphilis serology negative. |
| Friedreich's Ataxia | Hereditary ataxia, onset usually in childhood/adolescence. Dysarthria, nystagmus, loss of reflexes, pes cavus, scoliosis, cardiomyopathy. Genetic testing confirms. |
| Diabetic Neuropathy | Peripheral sensory loss (often "glove and stocking"), autonomic neuropathy. History of diabetes mellitus. Reflexes may be diminished. No Argyll Robertson pupils. |
| Spinal Cord Tumors or Syringomyelia (affecting posterior columns) | May cause sensory level, motor weakness, reflex changes. MRI of spine is diagnostic. Syringomyelia often causes dissociated sensory loss (pain/temp lost, touch preserved). |
| Alcoholic Neuropathy / Cerebellar Degeneration | History of chronic alcohol abuse. Peripheral neuropathy, cerebellar ataxia. |
| Multiple Sclerosis (Spinal Cord Lesions) | Can cause sensory ataxia if posterior columns affected. Relapsing-remitting course, optic neuritis, other CNS lesions on MRI. CSF oligoclonal bands. |
| Paraneoplastic Sensory Neuronopathy | Rapid onset sensory loss and ataxia associated with an underlying cancer. Anti-Hu antibodies often present. |
Prognosis and Complications
Without treatment, tabes dorsalis is a progressive disease leading to severe disability, including incapacitating ataxia, blindness (from optic atrophy), Charcot joints, and chronic debilitating pain. Penicillin treatment can arrest the progression of the disease, but established neurological damage is often permanent. Symptomatic improvement may occur in some aspects, but complete recovery of lost function is rare.
Long-term complications relate to the irreversible neurological deficits: chronic pain, risk of falls and injuries due to ataxia and sensory loss, neurogenic bladder requiring catheterization, and complications of trophic ulcers and Charcot joints.
Prevention and When to Seek Medical Attention
Prevention of tabes dorsalis and other forms of neurosyphilis relies on:
- Primary prevention of syphilis through safe sexual practices.
- Early diagnosis and adequate treatment of primary and secondary syphilis with appropriate penicillin regimens.
- Screening for syphilis in at-risk populations and during pregnancy.
Individuals should seek medical attention if they experience:
- Unexplained shooting or stabbing pains, especially in the legs.
- Progressive difficulty with balance or walking, particularly in the dark.
- Numbness, tingling, or loss of sensation in the limbs.
- Changes in vision or pupillary abnormalities.
- Symptoms of bladder dysfunction.
- A history of untreated or inadequately treated syphilis and development of neurological symptoms.
Early recognition and treatment of syphilis at any stage are crucial to prevent the devastating long-term consequences of neurosyphilis.
References
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187. (Standard guidelines for syphilis treatment).
- Ghanem KG, Ram S, Rice PA. The Modern Epidemic of Syphilis. N Engl J Med. 2020 Feb 27;382(9):845-854. (Overview of syphilis).
- Marra CM. Neurosyphilis. Continuum (Minneap Minn). 2015 Dec;21(6 Neuroinfectious Disease):1714-28.
- Timmermans M, Carr J. Neurosyphilis in the modern era. J Neurol Neurosurg Psychiatry. 2004 Dec;75(12):1727-30.
- Singh AE, Romanowski B. Syphilis: review with emphasis on clinical, epidemiologic, and some biologic aspects. Clin Microbiol Rev. 1999 Apr;12(2):187-209.
- Ropper AH, Samuels MA, Klein JP, Prasad S. Adams and Victor's Principles of Neurology. 11th ed. McGraw-Hill Education; 2019. (Chapter on Syphilis of the Nervous System).
- Golden MR, Marra CM, Holmes KK. Update on Syphilis: Resurgence of an Old Problem. JAMA. 2003 Sep 10;290(10):1510-4.
See also
- Anatomy of the spine
- Ankylosing spondylitis (Bechterew's disease)
- Back pain by the region of the spine:
- Back pain during pregnancy
- Coccygodynia (tailbone pain)
- Compression fracture of the spine
- Dislocation and subluxation of the vertebrae
- Herniated and bulging intervertebral disc
- Lumbago (low back pain) and sciatica
- Osteoarthritis of the sacroiliac joint
- Osteocondritis of the spine
- Osteoporosis of the spine
- Guidelines for Caregiving for Individuals with Paraplegia and Tetraplegia
- Sacrodinia (pain in the sacrum)
- Sacroiliitis (inflammation of the sacroiliac joint)
- Scheuermann-Mau disease (juvenile osteochondrosis)
- Scoliosis, poor posture
- Spinal bacterial (purulent) epiduritis
- Spinal cord diseases:
- Spinal spondylosis
- Spinal stenosis
- Spine abnormalities
- Spondylitis (osteomyelitic, tuberculous)
- Spondyloarthrosis (facet joint osteoarthritis)
- Spondylolisthesis (displacement and instability of the spine)
- Symptom of pain in the neck, head, and arm
- Pain in the thoracic spine, intercostal neuralgia
- Vertebral hemangiomas (spinal angiomas)
- Whiplash neck injury, cervico-cranial syndrome