Diabetic, alcoholic, toxic and small fiber sensory neuropathy (SFSN)
Understanding Types of Polyneuropathies (Polyneuritis)
Polyneuropathy, historically sometimes referred to as polyneuritis (though "neuritis" implies inflammation which is not always the primary pathology), is a condition characterized by damage or dysfunction of multiple peripheral nerves throughout the body. This typically results in symmetrical symptoms, often starting in the longest nerves (affecting feet and hands first, in a "stocking-glove" distribution). This section will discuss several common types of polyneuropathy.
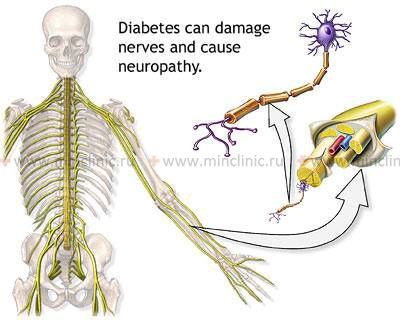
Diabetic Polyneuropathy
Diabetic polyneuropathy is a common and serious complication of diabetes mellitus, representing a type of nerve damage that results from the systemic metabolic derangements and intoxication of the body due to impaired tissue metabolism. While multiple factors contribute, a leading pathogenic factor in the onset of diabetic neuropathy is **microangiopathy** (damage to small blood vessels) concomitant with diabetes. This angiopathy leads to impaired regional blood circulation (ischemia) supplying the nerves (vasa nervorum), contributing to nerve damage. Other contributing factors include direct glucose toxicity, oxidative stress, and inflammation.
Depending on the specific nerves affected and the level of nerve damage in diabetic polyneuropathy, patients experience a variety of symptoms, including sensory disturbances (numbness, tingling/paresthesias, burning sensations, pain), and in more advanced cases, muscle weakness and autonomic dysfunction. The severity and type of symptoms (sensory, motor, autonomic) will vary among patients.
Microvascular and Macrovascular Complications of Diabetes Mellitus
Diabetic neuropathy is one of the major microvascular complications of diabetes. Other complications include:
Microvascular Complications:
Retinopathy |
Neuropathy |
Nephropathy |
|---|---|---|
|
Peripheral Neuropathy:
Autonomic Neuropathy:
|
|
Macrovascular Complications:
Coronary Artery Disease |
Cerebrovascular Disease |
Peripheral Vascular Disease (PVD) |
|---|---|---|
|
|
|
Alcoholic Polyneuropathy
Alcoholic polyneuropathy is a type of nerve damage that occurs in individuals with a history of chronic and excessive alcohol abuse. The exact mechanisms are multifactorial and include:
- Direct Toxic Effects of Alcohol and its Metabolites (e.g., acetaldehyde) on Nerves.
- Nutritional Deficiencies: Chronic alcoholism often leads to malnutrition and deficiencies in essential vitamins, particularly thiamine (Vitamin B1), but also pyridoxine (B6), cobalamin (B12), and folate, all of which are crucial for nerve health. Thiamine deficiency is a major contributor.
- Oxidative Stress and Impaired Axonal Transport.
Alcoholic polyneuropathy typically presents as a symmetrical, distal, sensorimotor neuropathy, predominantly affecting the lower extremities more severely than the upper extremities. Symptoms often include pain, paresthesias, muscle weakness, and gait disturbances. Autonomic dysfunction can also occur.
Toxic Polyneuropathy (Including Chemotherapy-Induced Polyneuropathy)
Toxic polyneuropathies are caused by exposure to various neurotoxic substances. Most manifest as a distal axonal degeneration that develops gradually over time in the patient. The causes are diverse and include:
- Medications:
- Chemotherapeutic Agents: Many anticancer drugs are neurotoxic, including platinum compounds (cisplatin, oxaliplatin), taxanes (paclitaxel, docetaxel), vinca alkaloids (vincristine), bortezomib, and thalidomide. Chemotherapy-induced peripheral neuropathy (CIPN) is a common and dose-limiting side effect.
- Antiretroviral Drugs: Some older nucleoside reverse transcriptase inhibitors (NRTIs) used for HIV treatment (e.g., stavudine, didanosine) can cause neuropathy.
- Antimicrobials: Isoniazid, metronidazole, nitrofurantoin, fluoroquinolones (rarely).
- Cardiovascular Drugs: Amiodarone, hydralazine, perhexiline.
- Other Medications: Colchicine, phenytoin, dapsone, and overuse of pyridoxine (Vitamin B6).
- Heavy Metals: Lead, mercury, arsenic, thallium.
- Industrial Solvents and Chemicals: Organophosphates, acrylamide, carbon disulfide, ethylene oxide, n-hexane.
- Environmental Substances: Certain pesticides.
When assessing a patient's condition, a temporal relationship between exposure to a toxic substance (time of administration and dosage) and the onset of clinical manifestations of neuropathy is usually noted. In general, exposure to small doses of a drug or toxin over a long period tends to be less acutely toxic to nerves than large doses administered over a short period, even if the cumulative dose is similar (though cumulative toxicity is a major factor for many agents like platinum drugs).
The onset of neuropathy may occur during exposure or, in some cases, may continue to progress even after the administration of the toxic substance is discontinued (a phenomenon known as "coasting"). This coasting effect can occur with drugs like platinum-based chemotherapies, benzene-related compounds (though benzene itself is more known for bone marrow toxicity, its metabolites or related industrial chemicals might be implied), certain NRTIs, or excessive pyridoxine.
Clinical analysis of the patient's history includes identifying:
- The relationship between the moment the toxin entered the patient's body and the onset of motor and sensory symptoms of nerve damage.
- Any other concomitant diseases that could independently cause or predispose to toxic neuropathy.
- Symptoms of general systemic intoxication related to the specific toxin.
Nerve biopsy is rarely performed for toxic neuropathies unless the diagnosis is uncertain, but it sometimes reveals characteristic signs for specific types of nerve injury, such as:
- Osmophilic inclusions within Schwann cells during intoxication with amiodarone, perhexiline, and chloroquinoline (a synthetic antimalarial).
- Massive perinodal axonal edema with certain benzene-related neuropathies (or other solvent-induced neuropathies).
Detection of certain toxins in body tissues or fluids can aid diagnosis:
- Heavy metals can be detected in urine (e.g., arsenic, thallium), hair, and nails (e.g., arsenic).
- Laboratory analysis of drug levels in blood plasma can also be useful in establishing the diagnosis of drug-induced toxic neuropathy if therapeutic ranges are exceeded or if a known neurotoxic drug is implicated.
Small Fiber Sensory Neuropathy (SFSN)
Small fiber sensory neuropathy (SFSN), or simply small fiber neuropathy (SFN), is a disorder characterized by selective damage to the small-diameter myelinated (Aδ) and unmyelinated (C) sensory nerve fibers in the skin and autonomic nervous system. These fibers are responsible for transmitting pain and temperature sensations, and for autonomic functions.
Symptoms of SFSN
The symptoms of SFSN are primarily sensory and can be quite distressing:
- Pain: Often described as burning, aching, or sharp, electric shock-like brief painful sensations.
- Paresthesias: Unusual sensations such as pins-and-needles, pricking, tingling, crawling, or buzzing.
- Numbness or Altered Sensation: Reduced sensitivity to pain or temperature.
- Allodynia or Hyperalgesia: Pain provoked by normally non-painful stimuli (allodynia) or an exaggerated pain response (hyperalgesia).
- Autonomic Symptoms (if small autonomic fibers are involved): Abnormal sweating (hyperhidrosis or anhidrosis), dry eyes/mouth, orthostatic intolerance, gastrointestinal dysmotility, or bladder dysfunction.
Since SFSN typically does not involve the large sensory fibers (which convey proprioception/balance information) or motor nerve fibers, patients usually do not experience balance problems or muscle weakness unless there is coexisting large fiber neuropathy.
In most patients, these symptoms start distally in the feet and progress upwards in a length-dependent pattern (affecting the longest nerves first). In advanced cases, it may involve the hands. However, a smaller percentage of patients experience a non-length-dependent SFSN, with symptoms appearing more diffusely over the whole body, including the trunk and sometimes even the face, often with a subacute onset. Most non-length-dependent cases are idiopathic (of unknown cause).
The majority of SFSN cases are length-dependent. This type is often associated with:
- Diabetes mellitus or impaired glucose metabolism (prediabetes). Length-dependent SFSN in these cases may progress to typical diabetic polyneuropathy involving large fibers as well.
- Connective tissue diseases (e.g., Sjogren's syndrome, lupus).
- Certain infections (e.g., HIV).
- Amyloidosis.
- Paraneoplastic syndromes.
- Genetic mutations (e.g., in SCN9A or SCN10A genes).
- However, in a significant percentage of patients (up to 50%), no underlying etiology is found, and these are classified as idiopathic SFSN.
Diagnosis of SFSN
The diagnosis of SFSN is based on a combination of characteristic symptoms, clinical examination findings, and supporting laboratory investigations. Standard electromyography (EMG) and nerve conduction studies (NCS) are typically normal in pure SFSN because these tests primarily evaluate large myelinated nerve fibers.
Key diagnostic tools include:
- Detailed History and Neurological Examination: Focusing on sensory symptoms and signs (pinprick, temperature sensation).
- Quantitative Sensory Testing (QST): Can assess thresholds for temperature and pain perception.
- Skin Biopsy with Epidermal Nerve Fiber Density (ENFD) Measurement: This is considered a gold standard objective test. A small punch biopsy of the skin (usually from the distal leg and sometimes thigh) is taken, and the density of small nerve fibers in the epidermis is quantified. A reduced ENFD confirms the diagnosis.
- Autonomic Function Testing: If autonomic symptoms are present (e.g., QSART - quantitative sudomotor axon reflex test, thermoregulatory sweat test, cardiovascular reflex tests).
- Blood Tests: To screen for underlying causes like diabetes (fasting glucose, HbA1c, glucose tolerance test), vitamin deficiencies, autoimmune markers, etc.
Nerve and muscle biopsies are rarely needed for SFSN diagnosis unless a vasculitic neuropathy or other specific pathology is suspected.
Treatment of SFSN
Treatment of SFSN depends on identifying and managing the underlying etiology, if possible. If it is due to diabetes or a prediabetic state, then optimum glycemic control, exercise, and weight loss to reduce insulin resistance are crucial.
Symptomatic treatment for painful sensory paresthesias and neuropathic pain includes:
- Anti-seizure Medications (Anticonvulsants): Gabapentin, pregabalin, carbamazepine, topiramate.
- Antidepressants: Tricyclic antidepressants (TCAs) like amitriptyline or nortriptyline; serotonin-norepinephrine reuptake inhibitors (SNRIs) like duloxetine or venlafaxine.
- Topical Agents: Capsaicin cream, lidocaine patches.
- Analgesics: Simple analgesics like NSAIDs are often ineffective for neuropathic pain. In some cases, tramadol or, rarely, stronger opioid drugs may be considered for severe, refractory pain under strict medical supervision.
- Intravenous Immunoglobulin (IVIG): May be considered in some cases of autoimmune-mediated or idiopathic SFSN, though evidence is still evolving.
In severe painful conditions, patients may be referred to a specialized pain clinic or multidisciplinary pain management centers for a comprehensive approach involving medication management, physical therapy, psychological support, and interventional pain procedures.
Diagnosis of Diabetic, Alcoholic, and Toxic Polyneuropathies
Clinical Evaluation
Symptoms of damage to any peripheral nerve, as seen in diabetic polyneuropathy and alcoholic polyneuropathy (historically termed polyneuritis), can manifest as a combination of motor, reflex, sensory, and vasomotor-secretory-trophic disorders. The comprehensive examination of the patient traditionally begins with meticulous collection of anamnestic information (medical history) during a detailed neurological examination. This includes onset and progression of symptoms, nature of sensory disturbances (numbness, tingling, pain, burning), motor weakness, balance issues, autonomic symptoms, and a thorough review of medical history (diabetes control, alcohol intake, medication/toxin exposure).
Electrodiagnostic Studies (EMG and ENG)
Classical electrodiagnostic studies, including Electromyography (EMG) and Nerve Conduction Studies (ENG or NCS), are of paramount importance in the comprehensive evaluation of polyneuropathies. These tests are typically most informative from 2 weeks after nerve damage onwards and are crucial for:
- Confirming the presence and characterizing the type of neuropathy: Axonal loss, demyelination, or mixed.
- Assessing the severity and distribution of nerve damage.
- Differentiating degenerative (axonal) from non-degenerative (primarily demyelinating) disorders.
- Prognostication: To a certain extent, the findings can help determine the prognosis for recovery in conditions like diabetic neuropathy and alcoholic polyneuropathy. For instance, the restoration of muscle movements to a functional strength (e.g., 4-5 points on the MRC scale) is typically observed only in those muscles where classical electrodiagnostics reveal reduced electroexcitability or a reaction of partial degeneration (indicating some preserved axons). A reaction of complete degeneration (no electrical response) generally correlates with a poor prognosis for spontaneous motor recovery in the affected muscles.
In very late periods after nerve damage in diabetic or alcoholic polyneuropathy, the finding of complete loss of electroexcitability in paralyzed muscles provides an additional reason to reconsider or refuse nerve surgery aimed at functional restoration, as the target muscles may no longer be viable.
Contrary to some conventional wisdom, small intrinsic muscles (e.g., of the hands or feet) often demonstrate more stability in their ability to respond to electrical stimulation during classical electrodiagnostic testing, even in the presence of significant neuropathy, compared to larger proximal muscles.
The appearance of previously absent motor unit action potentials (MUAPs) on an EMG in diabetic or alcoholic polyneuropathy can sometimes indicate early signs of reinnervation and predict the potential for movement restoration long before the first clinical signs of such recovery become apparent.
Diagnosis of the level and type of nerve damage in diabetic, alcoholic, and toxic polyneuropathy affecting the lower extremities is commonly performed using electroneurography (ENG/NCS) and electromyography (EMG).
Treatment Principles for Polyneuropathies
The treatment for polyneuropathies, including diabetic, alcoholic, and toxic forms, is selected individually for each case, considering the underlying cause, severity, and specific symptoms.
Addressing the Underlying Cause
This is the most critical aspect of management:
- Diabetic Polyneuropathy: Strict glycemic control (optimizing blood sugar levels) is paramount to prevent progression. Management of other cardiovascular risk factors (hypertension, dyslipidemia) is also important.
- Alcoholic Polyneuropathy: Complete abstinence from alcohol is essential. Nutritional supplementation, especially with thiamine (Vitamin B1) and other B vitamins, is crucial.
- Toxic Polyneuropathy: Identification and removal of the offending toxin or discontinuation/dose adjustment of the causative medication is the primary step. Specific chelating agents may be used for certain heavy metal poisonings.
Symptomatic Management
Painful neuropathic symptoms are common and often require specific medications (as detailed for SFSN, including anticonvulsants like gabapentin/pregabalin, antidepressants like TCAs/SNRIs, and topical agents).
Rehabilitative and Supportive Therapies
A comprehensive course of treatment for diabetic and alcoholic polyneuropathy often includes a set of conservative procedures aimed at improving nerve function, reducing symptoms, and enhancing quality of life. The duration of treatment and potential for recovery can be influenced by factors such as the severity of regional arterial circulatory disorders, which are common in these conditions.
Due to impaired regional arterial circulation, the restoration of lost peripheral nerve functions in diabetic and alcoholic polyneuropathy often takes much longer compared to other types of polyneuritis or neuropathies where circulatory disorders are not a primary cause (e.g., some traumatic neuritides).
Rehabilitative measures may include:
- Physical Therapy: To maintain muscle strength, improve balance, and manage pain. Exercises to improve range of motion in affected joints.
- Occupational Therapy: To adapt daily activities and maintain independence.
- Pharmacological Support:
- Vitamins, particularly B-complex vitamins (B1, B6, B12), Vitamin C, and Vitamin E.
- Lipoic acid preparations (e.g., alpha-lipoic acid, available as Espa-Lipon, Berlition) are antioxidants that have shown some benefit in improving symptoms of diabetic neuropathy.
- Homeopathic remedies are sometimes used, though scientific evidence for their efficacy is generally lacking.
- Neuromodulation Techniques:
- Acupuncture: Can be very effective in managing neuropathic pain and improving some sensory symptoms.
- Transcutaneous Electrical Nerve Stimulation (TENS) or other forms of Nerve Stimulation and Muscle Stimulation: May help alleviate pain and, in some cases, improve muscle function or reduce paresthesias. Neurostimulation through physiotherapy can accelerate the elimination of paresthesias and pain, and help restore strength in leg muscles in alcoholic polyneuropathy and diabetic neuropathy of the lower extremities.
- Foot Care: Essential for diabetic neuropathy to prevent ulcers and infections.
In specialized clinics, physical therapy often incorporates neurostimulation of the nerves of the lower extremities. Acupuncture is also frequently used as a component of the stimulatory effect on peripheral nerves in neuropathy of the lower extremities.
The use of acupuncture (reflexology) can be very effective in the comprehensive treatment of Diabetic, Alcoholic, Toxic, and Small Fiber Sensory Neuropathy (SFSN), helping to alleviate pain and improve sensory symptoms.
Neurostimulation as a physiotherapeutic modality can accelerate the elimination of paresthesia and pain, and help restore strength in the leg muscles during the treatment of alcoholic polyneuropathy, diabetic neuropathy, and other neuropathies of the lower extremities.
Differential Diagnosis of Polyneuropathy
Polyneuropathy can have numerous causes. Differentiating between diabetic, alcoholic, toxic, and other forms requires careful evaluation:
| Type of Polyneuropathy | Key Differentiating Features |
|---|---|
| Diabetic Polyneuropathy | History of diabetes mellitus (often long-standing or poorly controlled); predominantly distal, symmetrical, sensory > motor; autonomic features common. Elevated blood glucose/HbA1c. |
| Alcoholic Polyneuropathy | History of chronic, excessive alcohol intake; often associated with nutritional deficiencies (especially thiamine); painful sensory symptoms, distal weakness, gait ataxia. |
| Toxic Polyneuropathy (e.g., CIPN, heavy metals) | History of exposure to specific neurotoxin (medication, industrial agent); pattern depends on toxin (e.g., predominantly sensory, motor, or mixed; axonal or demyelinating). Temporal relationship to exposure. |
| Small Fiber Sensory Neuropathy (SFSN) | Burning pain, paresthesias, altered temperature/pain sensation; normal large fiber NCS/EMG; diagnosis by skin biopsy (ENFD) or QST. Can be idiopathic or secondary to diabetes, autoimmune disease, etc. |
| Guillain-Barré Syndrome (GBS) | Acute/subacute onset, rapidly progressive ascending symmetrical weakness, areflexia, often follows infection. Primarily motor, demyelinating. CSF shows albuminocytologic dissociation. |
| Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) | Chronic or relapsing-remitting progressive symmetrical weakness and sensory loss; demyelinating features on NCS/EMG. Responds to immunotherapy. |
| Nutritional Deficiency Neuropathies (e.g., B12, B6, B1, E deficiency) | Specific pattern depending on vitamin (e.g., B12: sensory ataxia, paresthesias; B6 excess: sensory neuropathy). History of malnutrition, malabsorption, specific dietary restrictions, or excessive supplementation (B6). |
| Hereditary Neuropathies (e.g., Charcot-Marie-Tooth disease) | Slowly progressive, often family history; characteristic foot deformities (pes cavus), distal weakness and atrophy. Genetic testing. |
| Vasculitic Neuropathy | Often painful, asymmetrical multifocal neuropathy (mononeuritis multiplex), may have systemic signs of vasculitis. Nerve biopsy can be diagnostic. |
| Paraneoplastic Neuropathy | Associated with underlying cancer; can be sensory, sensorimotor, or autonomic. Detection of onconeural antibodies. |
Complications and Prognosis
Potential complications of polyneuropathies include:
- Chronic pain and impaired quality of life.
- Increased risk of falls due to sensory loss or weakness.
- Development of foot ulcers, infections, and potential amputations (especially in diabetic neuropathy).
- Muscle atrophy and contractures.
- Autonomic dysfunction leading to cardiovascular, gastrointestinal, or urogenital problems.
- Disability and loss of independence.
The prognosis varies greatly depending on the underlying cause, severity at diagnosis, and response to treatment. Early diagnosis and management of the primary cause can often slow or halt progression and improve symptoms. Some neuropathies (e.g., some toxic or inflammatory types) may be partially or fully reversible if the cause is removed or treated promptly. Others, like advanced diabetic or some hereditary neuropathies, are often progressive.
Prevention Strategies
Prevention focuses on addressing modifiable risk factors:
- Diabetes: Strict glycemic control, regular foot care, management of cardiovascular risk factors.
- Alcohol: Moderation or abstinence from alcohol. Ensuring adequate nutrition, especially B vitamins.
- Toxins: Avoiding exposure to known neurotoxins in the workplace or environment. Careful monitoring and dose adjustments for potentially neurotoxic medications.
- Nutritional Deficiencies: Maintaining a balanced diet and addressing any malabsorption issues.
When to Consult a Neurologist
Consultation with a neurologist is recommended if an individual experiences:
- Persistent numbness, tingling, burning, or pain in the extremities (hands or feet).
- Progressive muscle weakness or difficulty with balance or coordination.
- Symptoms suggestive of autonomic dysfunction (e.g., dizziness on standing, unexplained sweating changes, bladder or bowel problems).
- Known risk factors for neuropathy (e.g., diabetes, heavy alcohol use, chemotherapy) and development of new neurological symptoms.
- Unexplained neurological symptoms.
A neurologist can perform a comprehensive evaluation, including electrodiagnostic studies and other necessary tests, to establish an accurate diagnosis, identify the underlying cause, and develop an appropriate management plan.
References
- Callaghan BC, Kerber KA, Lisabeth LL, et al. Role of neurologists and diagnostic tests in the management of distal symmetric polyneuropathy. JAMA Neurol. 2014;71(9):1143-1149.
- Dyck PJ, Karnes JL, O'Brien PC, et al. The Rochester Diabetic Neuropathy Study: reassessment of tests and criteria for diagnosis and staged severity. Neurology. 1992;42(6):1164-1170.
- American Diabetes Association. Peripheral neuropathy. Diabetes Care. 2023;46(Suppl 1):S151-S169. (Refer to latest ADA guidelines)
- Julian T, Glascow N, Sye S, Zis P. Alcoholic peripheral neuropathy: a systematic review and meta-analysis. J Neurol. 2019;266(11):2907-2919.
- Windebank AJ. Metal neuropathy. In: Dyck PJ, Thomas PK, eds. Peripheral Neuropathy. 4th ed. Philadelphia, PA: Elsevier Saunders; 2005:2351-2362.
- Staff NP, Windebank AJ. Peripheral neuropathy due to vitamin deficiency, toxins, and drugs. Continuum (Minneap Minn). 2014 Oct;20(5 Peripheral Nervous System Disorders):1293-311.
- Lacomis D. Small-fiber neuropathy. Muscle Nerve. 2002 Aug;26(2):173-88.
- Devigili G, Tugnoli V, Penza P, et al. The diagnostic criteria for small fibre neuropathy: from symptoms to new non-invasive diagnostic methods. Brain. 2008 Jul;131(Pt 7):1912-25.
- Peltier A, Goutman SA, Callaghan BC. Painful neuropathies. Muscle Nerve. 2014 Apr;49(4):467-81.
See also
- Anatomy of the nervous system
- Spinal disc herniation
- Pain in the arm and neck (trauma, cervical radiculopathy)
- The eyeball and the visual pathway:
- Anatomy of the eye and physiology of vision
- The visual pathway and its disorders
- Eye structures and visual disturbances that occur when they are affected
- Retina and optic disc, visual impairment when they are affected
- Impaired movement of the eyeballs
- Nystagmus and conditions resembling nystagmus
- Dry Eye Syndrome
- Optic nerve and retina:
- Compression neuropathy of the optic nerve
- Edema of the optic disc (papilledema)
- Ischemic neuropathy of the optic nerve
- Meningioma of the optic nerve sheath
- Optic nerve atrophy
- Optic neuritis in adults
- Optic neuritis in children
- Opto-chiasmal arachnoiditis
- Pseudo-edema of the optic disc (pseudopapilledema)
- Toxic and nutritional optic neuropathy
- Neuropathies and neuralgia:
- Diabetic, alcoholic, toxic and small fiber sensory neuropathy (SFSN)
- Facial nerve neuritis (Bell's palsy, post-traumatic neuropathy)
- Fibular (peroneal) nerve neuropathy
- Median nerve neuropathy
- Neuralgia (intercostal, occipital, facial, glossopharyngeal, trigeminal, metatarsal)
- Post-traumatic neuropathies
- Post-traumatic trigeminal neuropathy
- Post-traumatic sciatic nerve neuropathy
- Radial nerve neuropathy
- Tibial nerve neuropathy
- Trigeminal neuralgia
- Ulnar nerve neuropathy
- Tumors (neoplasms) of the peripheral nerves and autonomic nervous system (neuroma, sarcomatosis, melanoma, neurofibromatosis, Recklinghausen's disease)
- Carpal tunnel syndrome
- Ulnar nerve compression in the cubital canal