Ulnar nerve neuropathy
- Understanding Ulnar Nerve Neuropathy
- Symptoms and Clinical Presentation of Ulnar Nerve Neuropathy
- Diagnosis of Ulnar Nerve Neuropathy
- Treatment of Ulnar Nerve Neuropathy (Ulnar Neuritis)
- Differential Diagnosis of Hand Weakness and Ulnar-Sided Sensory Loss
- Prognosis and Potential Complications
- Prevention Strategies
- When to Consult a Specialist (Neurologist, Hand Surgeon)
- References
Understanding Ulnar Nerve Neuropathy
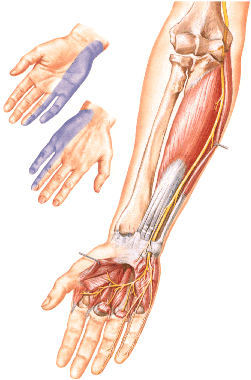
Ulnar nerve neuropathy refers to damage or dysfunction of the ulnar nerve (nervus ulnaris), a major peripheral nerve of the upper limb. This condition can lead to characteristic motor deficits, primarily affecting hand grip and fine finger movements, as well as sensory disturbances in the ulnar aspect of the hand.
Anatomy and Function of the Ulnar Nerve
The ulnar nerve is a mixed nerve, containing both motor and sensory fibers. It originates primarily from the C8 and T1 spinal nerve roots (with occasional minor contributions from Th2). These fibers initially pass through the lower trunk and then predominantly form the medial cord of the brachial plexus, from which the ulnar nerve arises.
The ulnar nerve travels down the medial aspect of the arm, passes posterior to the medial epicondyle of the humerus at the elbow (through the cubital tunnel), then enters the forearm to supply muscles and continues into the hand via Guyon's canal at the wrist.
Key functions innervated by the ulnar nerve include:
- Motor Functions:
- In the forearm: Flexor carpi ulnaris (assists with wrist flexion and ulnar deviation) and the medial half of the flexor digitorum profundus (responsible for flexion of the distal interphalangeal - DIP - joints of the ring and little fingers).
- In the hand: Most of the intrinsic muscles of the hand, including:
- Hypothenar muscles (abductor digiti minimi, flexor digiti minimi brevis, opponens digiti minimi - controlling little finger movements).
- All interosseous muscles (dorsal and palmar - responsible for finger abduction and adduction, and MCP joint flexion with IP joint extension).
- The medial two lumbrical muscles (to the ring and little fingers - similar function to interossei).
- Adductor pollicis muscle (adduction of the thumb).
- Deep head of the flexor pollicis brevis.
- Sensory Functions: The ulnar nerve provides sensation to:
- The ulnar (medial) aspect of the hand, both palm and dorsum.
- The entire little finger (V).
- The ulnar half (medial aspect) of the ring finger (IV).
- Sometimes, it may partially contribute to the sensation of the ulnar side of the middle finger (III).
Thus, the motor function of the ulnar nerve primarily consists of ulnar deviation and palmar flexion of the wrist, flexion of the V, IV, and partly III fingers (especially DIP joints), adduction and abduction of the fingers, and adduction of the thumb. It also contributes to the extension of the middle and terminal phalanges of the fingers via the lumbricals and interossei. Regarding the innervation of finger movements, the function of the ulnar nerve is closely associated with that of the median nerve; however, the ulnar nerve is primarily related to the function of the V and IV fingers, while the median nerve primarily controls the function of the II and III fingers.
Common Causes and Sites of Injury/Compression
Ulnar nerve neuropathy can occur due to various mechanisms, with common sites of injury or entrapment including:
- Elbow (Cubital Tunnel Syndrome): This is the most common site of ulnar nerve entrapment. The nerve passes through a narrow fibro-osseous tunnel (the cubital tunnel) behind the medial epicondyle. Causes include:
- Prolonged or repetitive elbow flexion (e.g., sleeping with elbow bent, phone use).
- Direct trauma or contusion to the medial elbow ("funny bone").
- Chronic external pressure on the elbow (e.g., leaning on armrests).
- Arthritis, bone spurs, or ganglia in the elbow joint.
- Valgus deformity of the elbow.
- Wrist (Guyon's Canal Syndrome): Compression of the ulnar nerve as it passes through Guyon's canal at the wrist. Causes include:
- Repetitive trauma (e.g., using tools, cycling - "handlebar palsy").
- Ganglion cysts or other tumors.
- Fractures of the hamate bone.
- Arthritis.
- Trauma:
- Fractures of the humerus (especially supracondylar or medial epicondyle), ulna, or wrist bones.
- Dislocations of the elbow or wrist joints.
- Lacerations or penetrating injuries to the arm, forearm, or wrist.
- Post-injection injury if a drug is inadvertently injected into or near the nerve.
- Systemic Conditions: Diabetes mellitus, rheumatoid arthritis, hypothyroidism.
- Prolonged Clamping or Pressure: During surgery or prolonged immobility.
- Iatrogenic Injury: During surgical procedures in the vicinity of the nerve.
Damage to the ulnar nerve, whether from surgery, injury (including post-injection issues), direct blows, prolonged clamping, bone fractures, or joint dislocations, is often accompanied by inflammatory changes in it (ulnar nerve neuritis) and manifests as impaired motor and sensory function in the area of its innervation in the hand.
Symptoms and Clinical Presentation of Ulnar Nerve Neuropathy
The clinical manifestations of ulnar nerve neuropathy depend on the level and severity of the nerve lesion.
Impact of Lesion Level (Brachial Plexus vs. Peripheral)
With damage to the **spinal nerves C8-T1(-T2)**, the **lower trunk**, or the **medial cord of the brachial plexus**, the function of the ulnar nerve suffers significantly. This often occurs in combination with damage to the medial cutaneous nerves of the arm and forearm (causing sensory loss in these areas) and can involve partial dysfunction of the median nerve, specifically its lower root/leg (contributing to weakness of finger flexors and thenar muscles). This constellation of symptoms can create a clinical picture similar to or part of **Dejerine-Klumpke paralysis** (lower brachial plexus palsy).
The ulnar nerve gives off its first muscular branches in the forearm. Therefore, damage to the nerve at or above the elbow joint (e.g., in the cubital tunnel) or in the upper part of the forearm will affect both forearm and hand muscles, giving a similar clinical picture for high lesions. Damage to the ulnar nerve in the area of the middle and lower third of the forearm (distal to branches to flexor carpi ulnaris and flexor digitorum profundus) will spare the innervation of these forearm muscles. In such cases, palmar flexion of the wrist (by FCU) and flexion of the terminal phalanges of the V and IV fingers (by FDP) do not suffer as much or at all. However, the degree of "clawing" of the hand (see below) often increases with more distal lesions because the extrinsic finger flexors (FDP) are relatively unopposed by the paralyzed intrinsic hand muscles.
Motor Deficits and "Claw Hand" Deformity
Complete damage to the ulnar nerve leads to:
- Weakening of palmar flexion and ulnar deviation of the wrist (due to paralysis of flexor carpi ulnaris).
- Weakness or lack of flexion of the DIP joints of the IV (ring) and V (little) fingers, and sometimes part of the III (middle) finger (due to paralysis of the ulnar part of flexor digitorum profundus).
- Inability to abduct (spread) and adduct (bring together) the fingers, especially the V and IV fingers (due to paralysis of interosseous muscles).
- Inability to adduct the thumb (paralysis of adductor pollicis).
- Weakness or paralysis of hypothenar muscles (little finger movements).
- Atrophy of the muscles of the hand innervated by the ulnar nerve becomes distinctly noticeable over time. This includes retraction of the interosseous spaces (guttering between metacarpals, especially the first dorsal interosseous space) and a sharp flattening of the hypothenar eminence (the fleshy mound at the base of the little finger).
- As a result of ulnar nerve damage, the hand often takes on the characteristic appearance of a **"claw hand" (main en griffe)** or "ulnar claw." This deformity involves hyperextension at the metacarpophalangeal (MCP) joints and flexion at the interphalangeal (IP) joints of the IV and V fingers (and sometimes III). This occurs because the ulnar-innervated lumbricals and interossei (which flex MCPs and extend IPs) are paralyzed, while the extrinsic extensors (radial nerve) and long flexors (median and ulnar nerves, with FDP to IV/V being ulnar) are relatively unopposed or imbalanced. The clawing is especially pronounced for the V and IV fingers. The fingers may also be somewhat spread apart (abducted), particularly the V finger, due to paralysis of adductor muscles.
Sensory Disturbances
Superficial sensitivity (light touch, pain, temperature) in ulnar neuritis or neuropathy is typically impaired on the skin of:
- The little finger (V).
- The ulnar half of the ring finger (IV).
- The corresponding ulnar surface of the hand, both palmar and dorsal aspects.
The joint-muscular sense (proprioception) is usually primarily affected in the little finger with ulnar nerve lesions.
Pain and Autonomic/Trophic Changes
Pain with damage to the ulnar nerve is not uncommon and usually radiates to the little finger and ulnar side of the hand. Autonomic and trophic changes can also occur:
- Cyanosis (bluish discoloration) or pallor of the skin in the affected area.
- Sweating disorders (anhidrosis or hyperhidrosis).
- A decrease in skin temperature in the ulnar distribution, roughly coinciding with the area of sensory disturbances.
- Skin dryness, nail changes (brittleness, ridging), and thinning of subcutaneous tissue over time.
Specific Clinical Tests
To determine movement disorders that occur when the ulnar nerve is damaged, the following basic tests are commonly used:
- Fist Clasp Test: When the patient attempts to clench their hand into a fist, the V and IV fingers (and sometimes partly the III finger) do not bend (flex at MCP and IP joints) sufficiently or remain partially extended due to weakness of interossei, lumbricals, and FDP to these fingers.
- Weakness of Little Finger Flexion/Abduction: Inability to effectively bend the terminal phalanx of the V finger or to "scratch" with the little finger on a table while the palm is held flat against it (tests flexor digiti minimi and FDP). Inability to abduct the little finger against resistance (tests abductor digiti minimi).
- Impaired Finger Adduction/Abduction: Fingers cannot be brought together tightly or spread apart effectively, especially the V and IV fingers (tests interossei). This can be tested by asking the patient to hold a piece of paper between extended fingers.
- Froment's Sign (Thumb Adduction Test): To test the adductor pollicis muscle. The patient is asked to grasp a strip of paper firmly between the thumb and the radial side of the flexed index finger. In case of ulnar nerve damage and paralysis of the adductor pollicis, adduction of the thumb is impossible or very weak. To compensate and hold the paper, the patient hyperflexes the interphalangeal (IP) joint of the thumb, using the flexor pollicis longus muscle (innervated by the median nerve). This flexion of the thumb IP joint is a positive Froment's sign.
- Wartenberg's Sign: Persistent abduction of the little finger due to unopposed action of the extensor digiti minimi (radial nerve) when the ulnar-innervated adductor muscles (palmar interossei) are weak.
- Card Test: Inability to hold a card firmly between the adducted fingers due to interosseous weakness.
Diagnosis of Ulnar Nerve Neuropathy
Diagnosing ulnar nerve neuropathy involves a combination of clinical assessment to identify the pattern of weakness and sensory loss, and diagnostic testing to localize the exact site of compression (e.g., at the elbow or wrist).
Clinical Neurological Examination
A thorough physical examination is the first step:
- Inspection: The doctor looks for muscle atrophy (wasting) in the hypothenar eminence (palm base near the little finger) and the dorsal interossei (especially the first web space between the thumb and index finger). The presence of a "claw hand" deformity is noted.
- Palpation: The ulnar nerve is palpated at the elbow in the cubital tunnel. Thickening, tenderness, or subluxation (snapping of the nerve over the bone during flexion) may be observed.
- Sensory Testing: Sensation is tested on the little finger and the ulnar half of the ring finger. If sensation is preserved on the dorsal ulnar aspect of the hand (dorsal cutaneous branch territory), the lesion is likely at the wrist (Guyon's canal); if lost, it is likely at or above the elbow.
- Motor Testing: Strength testing of finger abduction (spreading fingers), little finger flexion, and thumb adduction.
- Provocative Tests:
- Tinel's Sign: Light tapping over the nerve at the cubital tunnel (elbow) or Guyon's canal (wrist). Tingling in the little finger indicates a positive test.
- Elbow Flexion Test: The patient holds the elbow fully flexed with the wrist extended for 1-3 minutes. Reproduction of symptoms suggests cubital tunnel syndrome.
Electrodiagnostic Studies (EMG/NCS)
Electromyography (EMG) and Nerve Conduction Studies (NCS) are considered the gold standard for confirming the diagnosis and determining the severity.
- Nerve Conduction Studies (NCS):
- Motor NCS: Measuring the conduction velocity of the ulnar nerve across the elbow is the most useful test for Cubital Tunnel Syndrome. A significant slowing of conduction velocity (or conduction block) in the elbow segment compared to the forearm segment confirms entrapment.
- Sensory NCS: Reduced amplitude or absence of sensory nerve action potentials (SNAP) from the little finger.
- Electromyography (EMG):
- A needle electrode examination of the intrinsic hand muscles (e.g., first dorsal interosseous, abductor digiti minimi) and forearm muscles (flexor carpi ulnaris).
- Finding denervation potentials (fibrillations) in the hand muscles but sparing the forearm muscles suggests a lesion at the wrist or distal forearm.
- Involvement of the flexor carpi ulnaris helps localize the lesion to the elbow or above.
- EMG also helps rule out C8/T1 radiculopathy by testing non-ulnar muscles innervated by the same roots.
Imaging Studies
Imaging is used to identify structural causes of compression.
- Ultrasound (Neuromuscular Ultrasound): High-resolution ultrasound can visualize the ulnar nerve at the elbow. It can detect nerve enlargement (swelling), dislocation of the nerve from the groove during movement, or compression by cysts or ganglia.
- Magnetic Resonance Imaging (MRI): Useful for identifying space-occupying lesions (tumors, ganglion cysts, osteophytes) at the elbow or wrist. It is also essential if a Pancoast tumor (lung apex) or brachial plexus lesion is suspected.
- X-ray: Performed to identify bone abnormalities, such as old fractures, bone spurs, or deformities (e.g., cubitus valgus) that may be stretching or compressing the nerve.
Treatment of Ulnar Nerve Neuropathy (Ulnar Neuritis)
The treatment for ulnar neuritis or neuropathy is selected individually for each specific case, considering the underlying cause, severity of symptoms, duration, and location of the nerve lesion. Treatment typically includes a combination of conservative procedures, and surgical intervention may be indicated in certain circumstances.
General Principles and Conservative Management
- Addressing the Underlying Cause: If a specific cause is identified (e.g., compression at the elbow or wrist, trauma, systemic disease), treating that primary condition is essential.
- Activity Modification and Protection:
- Avoiding activities that exacerbate symptoms (e.g., prolonged elbow flexion, direct pressure on the elbow or ulnar wrist).
- Using elbow pads or wrist splints (especially at night) to maintain the elbow in a position of slight extension or the wrist in a neutral position, thereby reducing pressure on the nerve at common entrapment sites.
- Ergonomic adjustments at work or during daily activities.
- Pain Management: NSAIDs for inflammatory pain; neuropathic pain medications (gabapentin, pregabalin, TCAs, SNRIs) for nerve-related pain.
Pharmacological Treatment
- Corticosteroids: A short course of oral corticosteroids or local corticosteroid injections near the site of entrapment (e.g., into the cubital tunnel or Guyon's canal, performed carefully to avoid direct nerve injection) may be considered to reduce inflammation and swelling.
- Vitamins: B-complex vitamins (group "B"), Vitamin C ("C"), and Vitamin E ("E") are often prescribed as supportive therapy for nerve health, though strong evidence for their efficacy in promoting significant nerve regeneration in all types of neuropathy is varied.
- Homeopathic Remedies: Some patients explore these options, but their effectiveness for nerve conditions is not scientifically established.
Rehabilitative Therapies
Physical and occupational therapy are important for managing symptoms and improving function.
- Physical Therapy: Exercises to maintain range of motion in the elbow, wrist, and fingers; nerve gliding exercises for the ulnar nerve; strengthening exercises for weakened muscles as recovery occurs. Modalities like heat/cold therapy or ultrasound. The elimination of paresthesia and pain, and the restoration of strength in the muscles during the treatment of ulnar neuropathy can be accelerated with physiotherapy.
- Occupational Therapy: To adapt daily activities, provide assistive devices (e.g., modified grips for tools), and teach joint protection techniques.
- Acupuncture: Can be very effective for pain relief and potentially improving sensory or motor symptoms in some patients with ulnar neuropathy.
- Nerve Stimulation and Muscle Stimulation:
- Transcutaneous Electrical Nerve Stimulation (TENS) for pain control.
- Neuromuscular Electrical Stimulation (NMES) to help maintain muscle mass and prevent disuse atrophy in denervated ulnar-innervated muscles while awaiting reinnervation.
Surgical Intervention
Surgical treatment for ulnar nerve neuropathy is considered if:
- Conservative management fails to provide relief after an adequate trial (typically 3-6 months).
- Symptoms are severe or progressively worsening.
- There is evidence of significant muscle weakness, atrophy, or persistent motor deficits.
- Electrodiagnostic studies show significant axonal loss or a persistent conduction block at an identifiable entrapment site.
- A specific compressive lesion (e.g., tumor, ganglion cyst, bone spur) is identified.
- Acute nerve transection or severe trauma has occurred.
Common surgical procedures include:
- Cubital Tunnel Release: Decompression of the ulnar nerve at the elbow by incising the fascial roof of the cubital tunnel (Osborne's ligament).
- Ulnar Nerve Transposition: Moving the ulnar nerve from its position behind the medial epicondyle to a new location anterior to it (subcutaneous, intramuscular, or submuscular transposition) to relieve tension and pressure. This is often done in conjunction with cubital tunnel release. Medial epicondylectomy (partial removal of the medial epicondyle) is another option.
- Guyon's Canal Release: Decompression of the ulnar nerve at the wrist.
- Neurolysis: Surgical freeing of the nerve trunk from scar tissue or adhesions.
- Nerve Repair (Neurorrhaphy) or Grafting: For traumatic nerve transections or severe segmental damage.
- Excision of compressive tumors or cysts.
- Tendon transfers or other reconstructive procedures for permanent "claw hand" deformity if nerve recovery is not expected.
Differential Diagnosis of Hand Weakness and Ulnar-Sided Sensory Loss
Symptoms of ulnar neuropathy need to be distinguished from other conditions affecting the hand and arm:
| Condition | Key Differentiating Features |
|---|---|
| Ulnar Nerve Neuropathy (Cubital Tunnel or Guyon's Canal) | Numbness/tingling in 4th (ulnar half) & 5th fingers, weakness of ulnar-innervated intrinsic hand muscles (hypothenar, interossei, adductor pollicis), +/- weakness of FCU/FDP to IV-V. Positive Tinel's at elbow/wrist. EMG/NCS localizes to ulnar nerve. |
| C8/T1 Radiculopathy | Neck pain, radiating arm pain/paresthesias in C8/T1 dermatome (medial forearm, ulnar hand). Weakness in C8/T1 myotomes (may include ulnar intrinsics, but also other muscles like finger flexors, triceps). Reflex changes (e.g., triceps if C7 also involved). Neck MRI diagnostic. |
| Lower Brachial Plexopathy (e.g., Thoracic Outlet Syndrome - neurogenic) | Pain, paresthesias, weakness often in C8/T1 distribution, but may involve other parts of plexus. Horner's syndrome possible with T1 involvement. Symptoms often worsen with arm elevation or specific maneuvers. EMG/NCS shows plexopathy. |
| Median Nerve Neuropathy (e.g., Carpal Tunnel Syndrome) | Numbness/tingling in thumb, index, middle, radial half of ring finger. Thenar weakness/atrophy. Does not typically cause ulnar-sided symptoms unless coexisting. |
| Peripheral Polyneuropathy | Usually symmetrical, distal "stocking-glove" sensory loss and weakness. Multiple nerves affected, not just ulnar. |
| Motor Neuron Disease (e.g., ALS) | Progressive weakness, may start in hand (e.g., split hand syndrome), but often associated with fasciculations, muscle atrophy, hyperreflexia (or mixed UMN/LMN signs). Sensory exam usually normal. |
| Syringomyelia (Cervical) | Can cause dissociated sensory loss (loss of pain/temperature, preserved touch/proprioception) in a cape-like distribution, weakness/atrophy in hands. MRI of spinal cord. |
Prognosis and Potential Complications
The prognosis for ulnar nerve neuropathy depends on the cause, severity, duration of compression/injury, and the timeliness of treatment.
- Mild, early compressive neuropathies often respond well to conservative measures.
- More severe or long-standing compression with axonal loss may result in incomplete recovery even with surgical decompression.
- Traumatic nerve transections have a more guarded prognosis.
Potential complications include:
- Persistent weakness and muscle atrophy (especially intrinsic hand muscles), leading to "claw hand" deformity and impaired hand function (difficulty with grip, fine motor tasks).
- Chronic pain or paresthesias.
- Permanent sensory loss in the ulnar distribution.
- Joint contractures.
Prevention Strategies
Preventive measures focus on avoiding prolonged or repetitive pressure on the ulnar nerve, especially at the elbow:
- Avoid leaning on elbows for extended periods.
- Use padding for elbows if repetitive pressure is unavoidable (e.g., certain occupations).
- Avoid prolonged or extreme elbow flexion.
- Ergonomic adjustments for workstations.
- Careful positioning during surgery or prolonged immobilization.
- Prompt management of elbow trauma or arthritis.
When to Consult a Specialist (Neurologist, Hand Surgeon)
Consultation with a neurologist, hand surgeon, or physician specializing in peripheral nerve disorders is recommended if:
- Numbness, tingling, or pain in the little finger, ring finger, or ulnar side of the hand is persistent or worsening.
- There is noticeable weakness in hand grip or fine finger movements (e.g., difficulty buttoning, clumsiness).
- Muscle wasting (atrophy) is observed in the hand (e.g., between fingers, at the base of the little finger).
- Symptoms follow an injury to the elbow or wrist.
- Conservative home measures do not provide relief.
Early diagnosis and appropriate intervention can improve outcomes and prevent long-term disability from ulnar nerve neuropathy.
References
- Stewart JD. Focal Peripheral Neuropathies. 3rd ed. Lippincott Williams & Wilkins; 2000. Chapter 10: Ulnar Neuropathy.
- Preston DC, Shapiro BE. Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic Correlations. 3rd ed. Elsevier Saunders; 2013. Chapter 16: Ulnar Neuropathy at the Elbow.
- American Academy of Orthopaedic Surgeons (AAOS). Ulnar Nerve Entrapment at the Elbow (Cubital Tunnel Syndrome). OrthoInfo. Rosemont, IL: AAOS.
- Caliandro P, La Torre G, Padua R, Giannini F, Padua L. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev. 2016 Nov 15;11(11):CD006839.
- Dyck PJ, Thomas PK. Peripheral Neuropathy. 4th ed. Elsevier Saunders; 2005. (Comprehensive reference).
- Campbell WW. DeJong's The Neurologic Examination. 8th ed. Lippincott Williams & Wilkins; 2019.
- Boone S, Gelberman RH, Calfee RP. The Management of Cubital Tunnel Syndrome. J Hand Surg Am. 2015 Sep;40(9):1897-904.
- Elhassan B, Steinmann SP. Entrapment neuropathy of the ulnar nerve. J Am Acad Orthop Surg. 2007 Nov;15(11):672-81.
See also
- Anatomy of the nervous system
- Spinal disc herniation
- Pain in the arm and neck (trauma, cervical radiculopathy)
- The eyeball and the visual pathway:
- Anatomy of the eye and physiology of vision
- The visual pathway and its disorders
- Eye structures and visual disturbances that occur when they are affected
- Retina and optic disc, visual impairment when they are affected
- Impaired movement of the eyeballs
- Nystagmus and conditions resembling nystagmus
- Dry Eye Syndrome
- Optic nerve and retina:
- Compression neuropathy of the optic nerve
- Edema of the optic disc (papilledema)
- Ischemic neuropathy of the optic nerve
- Meningioma of the optic nerve sheath
- Optic nerve atrophy
- Optic neuritis in adults
- Optic neuritis in children
- Opto-chiasmal arachnoiditis
- Pseudo-edema of the optic disc (pseudopapilledema)
- Toxic and nutritional optic neuropathy
- Neuropathies and neuralgia:
- Diabetic, alcoholic, toxic and small fiber sensory neuropathy (SFSN)
- Facial nerve neuritis (Bell's palsy, post-traumatic neuropathy)
- Fibular (peroneal) nerve neuropathy
- Median nerve neuropathy
- Neuralgia (intercostal, occipital, facial, glossopharyngeal, trigeminal, metatarsal)
- Post-traumatic neuropathies
- Post-traumatic trigeminal neuropathy
- Post-traumatic sciatic nerve neuropathy
- Radial nerve neuropathy
- Tibial nerve neuropathy
- Trigeminal neuralgia
- Ulnar nerve neuropathy
- Tumors (neoplasms) of the peripheral nerves and autonomic nervous system (neuroma, sarcomatosis, melanoma, neurofibromatosis, Recklinghausen's disease)
- Carpal tunnel syndrome
- Ulnar nerve compression in the cubital canal