Optic nerve and retina
- Anatomy and Physiology of the Optic Nerve and Retina
- Common Diseases and Pathologies of the Optic Nerve and Retina
- Diagnosis of Optic Nerve and Retinal Diseases
- Treatment Approaches for Optic Nerve and Retinal Diseases
- Differential Diagnosis of Vision Loss and Funduscopic Abnormalities
- Prognosis and Potential Complications
- When to Consult a Specialist (Ophthalmologist, Neurologist, Neuro-ophthalmologist)
- References
Anatomy and Physiology of the Optic Nerve and Retina
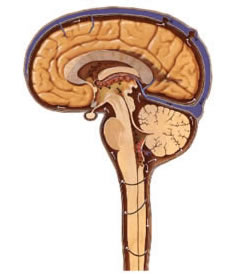
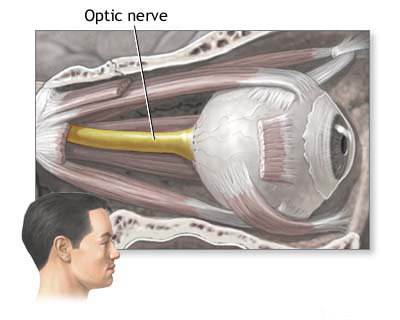
The optic nerve (cranial nerve II) and the retina are fundamental components of the visual system, responsible for capturing light and transmitting visual information to the brain. Ophthalmoscopic examination of a patient's eye provides a unique, non-invasive window to directly visualize parts of the central nervous system (the optic nerve head and retina) and its vasculature, allowing for the identification of changes associated with various local and systemic pathologies.
Formation and Pathway of the Optic Nerve
The optic nerve is essentially an extension of the brain and is formed by the convergence of axons from the retinal ganglion cells (neurons of the retina). This convergence occurs at the optic disc (also known as the optic nerve head), which is the anatomical blind spot of the eye as it lacks photoreceptors.
From the optic disc, the optic nerve fibers pass posteriorly out of the eyeball. The pathway includes:
- Intraocular portion: The optic disc.
- Intraorbital portion: The nerve travels within the orbit, behind the eye (retrobulbar segment), surrounded by meningeal sheaths (dura, arachnoid, pia mater) continuous with those of the brain.
- Intracanalicular portion: Passes through the optic canal in the sphenoid bone.
- Intracranial portion: Enters the cranial cavity (middle cranial fossa) and joins with the optic nerve from the contralateral eye to form the optic chiasm, located superior to the sella turcica (which houses the pituitary gland).
At the optic chiasm, fibers from the nasal (medial) half of each retina decussate (cross over) to the opposite side, while fibers from the temporal (lateral) half of each retina remain uncrossed. Posterior to the chiasm, these reorganized bundles of nerve fibers continue as the optic tracts. Each optic tract carries fibers from the contralateral visual field of both eyes and projects primarily to the lateral geniculate nucleus (LGN) of the thalamus, from where visual information is relayed to the primary visual cortex in the occipital lobe.
Vascular Supply and Clinical Implications
The optic nerve and retina receive their blood supply primarily from branches of the ophthalmic artery, which is itself a branch of the internal carotid artery. The central retinal artery, a branch of the ophthalmic artery, enters the optic nerve and spreads over the inner surface of the retina to supply its inner layers. The optic nerve head is supplied by branches from the short posterior ciliary arteries and the circle of Zinn-Haller.
Vascular compromise can have severe consequences for vision. For example, in approximately 25% of cases of clinically manifested occlusion (blockage) of the internal carotid artery, patients may experience amaurosis fugax – transient, episodic monocular (one eye) blindness or visual disturbance. This can be a warning sign, as there is a high probability of permanent blindness or stroke if the underlying vascular disease is not addressed. Patients describing such an episode might report a feeling of a "shadow" or "curtain" descending, ascending, or crossing their field of view, or a loss of peripheral parts of the visual field. They may also complain of blurred vision or transient dimming of vision in the affected eye, or the absence of the upper or lower half of the visual field. Most often, these symptoms of amaurosis fugax persist for only a few minutes. Less commonly, but more catastrophically, a stroke involving the internal carotid artery can lead to simultaneous occlusion of the ophthalmic artery or the central retinal artery, resulting in sudden, profound, and often permanent vision loss in one eye.
Common Diseases and Pathologies of the Optic Nerve and Retina
Diseases affecting the optic nerve and retina can arise from various etiological factors, including inflammatory, ischemic, compressive, toxic, hereditary, and degenerative processes. They differ in their primary site of localization and the type of pathological process involved. Based on these factors, a targeted plan for neurological and ophthalmological examination and subsequent treatment is formulated for patients.
Key conditions include:
Optic Disc Edema (Papilledema)
Optic disc edema refers to swelling of the optic nerve head. Papilledema specifically denotes optic disc edema caused by an increase in intracranial pressure (ICP). During ophthalmoscopy, papilledema is characterized by:
- Hyperemia (redness) and elevation of the optic disc.
- Prominence of the optic disc into the vitreous body.
- Blurring or obscuration of the disc margins.
- Dilated and tortuous retinal veins.
- Peripapillary hemorrhages (flame-shaped or punctate) on or around the disc surface.
- Cotton wool spots (retinal nerve fiber layer infarcts) may be present.
- Absence of a spontaneous venous pulsation (though this can be absent in some normal individuals).
A characteristic feature of early papilledema is the long-term preservation of visual acuity, although patients may report transient visual obscurations (momentary dimming or loss of vision, especially with changes in posture). The blind spot may be enlarged on visual field testing. However, as the edema progresses and becomes chronic, it can lead to secondary optic atrophy ("atrophy after stagnation" or post-papilledema optic atrophy), which is accompanied by a gradual and often irreversible decrease in visual acuity and the potential development of blindness. Stagnant changes in the fundus (papilledema) are observed in various conditions accompanied by an increase in intracranial pressure, such as brain tumors, hydrocephalus, meningitis, encephalitis, idiopathic intracranial hypertension (pseudotumor cerebri), or severe systemic hypertension.
Cases of optic disc edema where there are also direct signs of damage to the optic nerve or tract by the underlying pathological process (e.g., a tumor directly compressing the nerve) are sometimes referred to as complicated edema of the optic nerve head or compressive optic neuropathy with disc edema.
Optic Neuritis
Optic neuritis refers to an inflammatory process affecting the optic nerve. When the inflammation involves the optic nerve head (intraocular portion), it is called papillitis. Ophthalmoscopic findings in papillitis include hyperemia of the optic disc, blurring (washout) of its borders, dilation of retinal arteries and veins, peripapillary hemorrhages, and sometimes foci of necrosis or exudates on the surface of the disc (nipple) and in the surrounding retina. A key characteristic of optic neuritis is an early and often profound impairment of visual functions (decreased visual acuity, color vision defects, visual field loss - typically a central or cecocentral scotoma) that occurs simultaneously with or even precedes the development of ophthalmoscopic changes.
Optic neuritis is frequently associated with acute inflammatory diseases of the central nervous system, such as multiple sclerosis (MS - a very common cause, especially in young adults), meningitis, encephalitis, encephalomyelitis, and neurosyphilis. It can also be caused by other infections, autoimmune disorders, or be idiopathic.
Retrobulbar Optic Neuritis
Retrobulbar optic neuritis is an inflammation of the optic nerve occurring behind the eyeball (retrobulbar segment), without direct involvement or visible swelling of the optic nerve head initially. Consequently, changes in the fundus in patients during the acute phase are often uncharacteristic or minimal; there might only be mild hyperemia and slight blurring of the optic disc boundaries, or the disc may appear entirely normal. Pain with eye movements is a common symptom.
Retrobulbar optic neuritis is often unilateral. Clinically significant neurological signs include:
- Rapid and often severe vision loss.
- Visual field disturbances, typically a central or cecocentral scotoma (blind spot in the center of vision).
- Impaired color vision (dyschromatopsia), especially for red.
- Pain with eye movements.
- Afferent pupillary defect (Marcus Gunn pupil) on the affected side.
Retrobulbar optic neuritis is a common presenting symptom of multiple sclerosis. It can also occur with opticomyelitis (neuromyelitis optica spectrum disorder - NMOSD), Leber's hereditary optic neuropathy (though this is a genetic, not inflammatory, condition with a similar presentation initially), and opticochiasmal arachnoiditis. Phenomena of retrobulbar neuritis are also possible in other acute and chronic inflammatory diseases of the brain (encephalitis, meningitis, neurosyphilis) or due to sinus disease.
Optic Neuropathy
Optic neuropathy is a general term for damage or disease of the optic nerve from any cause. Besides inflammatory optic neuritis, other common types include:
- Ischemic Optic Neuropathy (ION): Due to impaired blood supply to the optic nerve head.
- Anterior ION (AION): Involves the optic disc. Can be arteritic (e.g., due to giant cell arteritis - GCA) or non-arteritic (NAION - more common, associated with vascular risk factors like diabetes, hypertension). Presents with sudden, painless vision loss.
- Posterior ION (PION): Affects the retrobulbar optic nerve; fundus initially normal. Rare, can occur after major surgery with hypotension/anemia, or with GCA.
- Compressive Optic Neuropathy: Caused by tumors (e.g., meningioma, pituitary adenoma, glioma), aneurysms, or thyroid eye disease compressing the optic nerve. Gradual vision loss.
- Traumatic Optic Neuropathy: Direct or indirect injury to the optic nerve from head trauma.
- Toxic/Nutritional Optic Neuropathy: Due to exposure to toxins (e.g., methanol, ethambutol, lead) or nutritional deficiencies (e.g., B-vitamins, folate).
- Hereditary Optic Neuropathies: E.g., Leber's hereditary optic neuropathy, dominant optic atrophy.
Clinically, optic nerve neuropathy (non-inflammatory) can manifest in patients with neurological deficits in the form of visual field loss (various patterns depending on site of lesion), decreased visual acuity, and sometimes subjective visual phenomena like color flashes (photopsias).
Optic Disc Atrophy
Optic atrophy is the end-stage result of damage to optic nerve axons, leading to their degeneration. During ophthalmoscopy, it reveals pallor of the optic disc, often with thinning of the retinal nerve fiber layer and vasoconstriction (narrowing of retinal blood vessels). Visual acuity is typically reduced, and visual field defects are present.
- Primary (Simple) Optic Atrophy: The optic disc appears pale with sharply defined margins. This develops in conditions where the damage is to the optic nerve or its pathways without preceding disc swelling (e.g., due to compression by a tumor, scar tissue, neuroma, gumma; trauma; hereditary optic neuropathies; toxic/nutritional causes; some forms of glaucoma). It can occur with syphilitic damage to the nervous system.
- Secondary Optic Atrophy: The optic disc appears pale with blurred or ill-defined margins, often with gliosis (scarring). This develops as a consequence of processes that initially caused optic disc edema (papilledema) or inflammation (papillitis/optic neuritis).
The Foerster-Kennedy syndrome is a specific clinical entity characterized by the combination of optic nerve atrophy in one eye (due to direct compression by a tumor) and papilledema (stagnant disc) in the other eye (due to increased intracranial pressure from the same tumor). This is classically observed with tumors on the basal surface of the frontal lobe of the brain, such as an olfactory groove meningioma or frontal lobe glioma. Gummas or tuberculomas in this location can also cause it. The optic atrophy occurs on the side of the tumor due to direct compression.
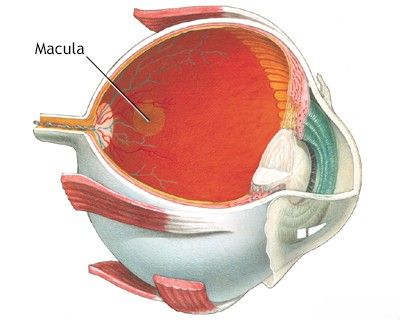
Macular Changes
The macula is the central part of the retina responsible for sharp, detailed central vision. Changes in the macula can significantly impact vision.
- Tay-Sachs Disease (Infantile Amaurotic Familial Idiocy): A rare, fatal genetic metabolic disorder. In the childhood form, funduscopic examination reveals a characteristic grayish opacity in the macular area with a "cherry-red spot" in its central part (the foveola appearing red due to contrast with the surrounding pale, lipid-laden retina).
- Juvenile Amaurotic Idiocy (e.g., Batten Disease): In these forms, patients may develop pigmentary degeneration of the retina in the central (macular) regions, along with optic atrophy and neurological decline.
- Age-Related Macular Degeneration (AMD): A common cause of vision loss in older adults.
- Diabetic Macular Edema: Swelling of the macula due to diabetic retinopathy.
- Macular Holes, Epiretinal Membranes.
Retinal Vascular Changes
Retinal vascular changes involve alterations in the appearance, course, and caliber of the retinal blood vessels (arteries and veins). These are most often observed in systemic conditions like:
- Hypertension (Hypertensive Retinopathy): Systemic high blood pressure leads to characteristic changes in the retinal vasculature. Several stages are distinguished:
- Stage of Initial Changes (Grade 1-2): Arterial narrowing (generalized or focal), increased arteriolar light reflex ("copper wiring" or "silver wiring" with more severe sclerosis), corkscrew tortuosity of venules (especially in the paramacular region - Gist's symptom), and transient arterial spasms are noted. Arteriovenous (AV) nicking or crossing changes (Gunn's sign, Salus' sign) where thickened arteries compress underlying veins.
- Stage of Organic Changes (Retinal Angiosclerosis): More pronounced vascular sclerosis, narrowing of vessel caliber with compaction of their walls.
- Severe Hypertensive Retinopathy (Grade 3-4 / Malignant Hypertension): In severe forms of hypertensive encephalopathy or malignant hypertension, retinopathy develops. This includes the above vascular phenomena plus signs of blood-retinal barrier breakdown: retinal hemorrhages (flame-shaped, dot-blot), cotton wool spots (nerve fiber layer infarcts), hard exudates (lipid deposits), and edema of the optic disc (papilledema). These changes constitute hypertensive neuroretinopathy.
- Cerebral Vascular Sclerosis (Atherosclerosis): Can affect retinal vessels similarly to hypertension.
- Diabetic Retinopathy: Microaneurysms, hemorrhages, exudates, neovascularization.
- Retinal Vein or Artery Occlusions.
Diagnosis of Optic Nerve and Retinal Diseases
Diagnosing diseases of the optic nerve and retina requires a comprehensive ophthalmological and often neurological evaluation:
- Detailed Medical and Ocular History.
- Visual Acuity Testing.
- Color Vision Testing.
- Visual Field Testing (Perimetry).
- Pupil Examination: Assessing size, shape, reactivity to light (direct and consensual), and checking for a relative afferent pupillary defect (RAPD or Marcus Gunn pupil).
- Slit-Lamp Biomicroscopy: To examine anterior segment structures and, with appropriate lenses, the posterior segment.
- Ophthalmoscopy (Funduscopy): Direct visualization of the optic disc, retina, macula, and retinal blood vessels. This is crucial for identifying papilledema, optic neuritis, atrophy, macular changes, and vascular abnormalities.
- Optical Coherence Tomography (OCT): Provides high-resolution cross-sectional images of the retina and optic nerve head, allowing for quantification of retinal nerve fiber layer thickness, macular thickness, and detection of subtle edema or atrophy.
- Fluorescein Angiography (FA) or Indocyanine Green Angiography (ICGA): To evaluate retinal and choroidal circulation, detect neovascularization, leakage, or ischemia.
- Neuroimaging (MRI or CT Scan): Of the brain and orbits, especially if compressive lesions, demyelinating disease, or increased intracranial pressure are suspected.
- Electrophysiological Tests:
- Visual Evoked Potentials (VEP): Measure electrical activity in the visual cortex in response to visual stimuli, helpful in assessing optic nerve function, especially in retrobulbar neuritis or demyelinating disease.
- Electroretinography (ERG): Measures electrical responses of retinal cells (photoreceptors, bipolar cells), useful for diagnosing various retinal dystrophies and dysfunctions.
- Systemic Evaluation: Blood tests for inflammatory markers, autoimmune diseases, infections, diabetes, hypertension, vitamin deficiencies, or genetic testing, as indicated by clinical suspicion.
Treatment Approaches for Optic Nerve and Retinal Diseases
Neurological and ophthalmological treatment for diseases of the optic nerve and retina is highly individualized by the physician for each specific case, based on the underlying etiology and severity.
General Principles
Treatment aims to:
- Address the underlying cause of the disease.
- Reduce inflammation.
- Preserve or improve vision.
- Prevent further damage and complications.
- Manage associated symptoms.
Treatment can include a complex of conservative procedures, medical therapies, and sometimes surgical intervention.
Specific Interventions
- Optic Neuritis: High-dose intravenous corticosteroids followed by an oral taper are often used for acute demyelinating optic neuritis (e.g., associated with MS) to speed up visual recovery, though they may not affect long-term visual outcome. Treatment of the underlying condition (e.g., MS disease-modifying therapies) is crucial.
- Papilledema: Management focuses on lowering intracranial pressure (e.g., treating the underlying brain tumor, hydrocephalus, or idiopathic intracranial hypertension with weight loss, diuretics like acetazolamide, CSF shunting, or optic nerve sheath fenestration).
- Ischemic Optic Neuropathy: For arteritic AION (GCA), urgent high-dose systemic corticosteroids are critical to prevent further vision loss in the affected and fellow eye. For NAION, there is no proven effective acute treatment, but management of vascular risk factors is important.
- Compressive Optic Neuropathy: Surgical decompression by removing the compressive lesion (e.g., tumor neurolysis to free the nerve trunk from a scar or tumor like meningioma) is often required. Radiation therapy may be an adjunct.
- Optic Atrophy: There is no direct treatment to reverse established optic atrophy. Management focuses on treating any underlying active disease to prevent further progression and on visual rehabilitation.
- Retinal Vascular Occlusions: Treatments may include ocular massage, anterior chamber paracentesis, anti-VEGF injections, laser photocoagulation, or management of systemic vascular risk factors, depending on the type and severity.
- Diabetic Retinopathy/Macular Edema: Strict glycemic and blood pressure control, laser photocoagulation, anti-VEGF injections, intravitreal steroids.
- Age-Related Macular Degeneration: Anti-VEGF injections for wet AMD, AREDS vitamin supplements for specific stages of dry AMD.
- Supportive Therapies (often adjunctive or for specific indications):
- Acupuncture: Some patients explore acupuncture, and it is considered very effective by some practitioners for treating optic neuritis or other nerve conditions, though robust scientific evidence for widespread efficacy in all optic nerve diseases is varied.
- Stimulation of the Optic Nerve and Oculomotor Muscles: Various forms of electrical or magnetic stimulation are being investigated, but are not standard practice.
- Vitamins: B-group vitamins ("B"), Vitamin C ("C"), and Vitamin E ("E") are often prescribed as general neurotrophic or antioxidant support.
- Antiviral Drugs: If a viral infection is a confirmed cause of optic neuritis (e.g., CMV retinitis in immunocompromised patients).
- Hormones (Corticosteroids): As mentioned, for inflammatory conditions.
- Homeopathic Remedies: Explored by some, but lack scientific validation.
The use of acupuncture is considered by some to be very effective as an adjunctive or complementary therapy in treating conditions like optic neuritis, aiming to reduce inflammation and promote recovery.
The duration of neurological and ophthalmological treatment and its frequency for diseases of the optic nerves and retina are dictated by the functional state of the optic nerve itself, the condition of the retina, and the degree to which lost light sensitivity or visual acuity is restored or stabilized.
Differential Diagnosis of Vision Loss and Funduscopic Abnormalities
The causes of vision loss and abnormal funduscopic findings are extensive. A systematic approach is crucial.
| Funduscopic Finding | Common Causes / Conditions | Key Differentiating Features / Associated Symptoms |
|---|---|---|
| Optic Disc Edema (Papilledema if due to ICP) | Increased intracranial pressure (tumor, hydrocephalus, IIH), Hypertensive crisis, Optic neuritis (papillitis), AION, Central retinal vein occlusion (CRVO), Compressive optic neuropathy. | Headache, nausea/vomiting, transient visual obscurations (with ICP). Vision loss (often sudden in AION/CRVO/neuritis). Pain with eye movement (neuritis). RAPD (if unilateral or asymmetric). |
| Optic Disc Pallor (Optic Atrophy) | Previous optic neuritis or papilledema, Glaucoma, Chronic compressive lesions, Ischemic optic neuropathy (late), Hereditary optic neuropathies, Toxic/Nutritional optic neuropathy. | Gradual or previous sudden vision loss, visual field defects, impaired color vision. History of preceding event or condition. |
| Retinal Hemorrhages | Diabetic retinopathy, Hypertensive retinopathy, Retinal vein occlusion, Anemia, Leukemia, Trauma, Age-related macular degeneration (wet), High altitude retinopathy. | Pattern of hemorrhage (flame, dot-blot, pre-retinal), associated vascular changes, exudates, neovascularization. Systemic disease history. |
| Cotton Wool Spots | Hypertension, Diabetes, HIV retinopathy, SLE, Severe anemia, CRVO. | Fluffy white retinal lesions (nerve fiber layer infarcts). Often associated with other signs of vascular disease. |
| Macular Changes (Edema, Exudates, Drusen, Hemorrhage) | Age-related macular degeneration, Diabetic macular edema, Cystoid macular edema (post-op, uveitis), Central serous chorioretinopathy, Macular hole, Epiretinal membrane. | Central vision loss, metamorphopsia (distortion), scotoma. OCT is key for diagnosis. |
| Cherry-Red Spot (Macula) | Central retinal artery occlusion (CRAO), Tay-Sachs disease, Niemann-Pick disease, Other lysosomal storage diseases. | Sudden profound vision loss (CRAO). Neurological regression in infants (storage diseases). |
| Retinal Vascular Attenuation/Sclerosis | Hypertension, Arteriosclerosis, Retinitis pigmentosa (late stage). | Narrowed arterioles, increased light reflex ("copper/silver wiring"), AV nicking. Peripheral field loss, night blindness (in RP). |
Prognosis and Potential Complications
The prognosis for diseases of the optic nerve and retina varies widely depending on the specific condition, its severity, the timeliness of diagnosis and treatment, and the patient's overall health.
- Some conditions, like mild optic neuritis in MS, may have good visual recovery.
- Others, like advanced glaucoma, severe ischemic optic neuropathy, or untreated retinal detachments, can lead to permanent and severe vision loss.
- Chronic conditions like diabetic retinopathy or AMD require lifelong management to preserve vision.
Potential complications include irreversible vision loss, blindness, visual field defects, impaired color vision, and secondary ocular issues (e.g., neovascular glaucoma from retinal ischemia).
When to Consult a Specialist (Ophthalmologist, Neurologist, Neuro-ophthalmologist)
Urgent or routine consultation with an appropriate specialist is necessary for any significant or unexplained visual symptoms or funduscopic abnormalities. This typically involves:
- Ophthalmologist: For primary evaluation of most eye and vision problems, diagnosis and management of retinal diseases, glaucoma, cataracts, etc.
- Neuro-ophthalmologist: A specialist at the interface of neurology and ophthalmology, crucial for complex optic nerve disorders, unexplained vision loss, visual field defects, papilledema, and disorders of eye movements.
- Neurologist: If visual symptoms are part of a broader neurological condition (e.g., MS, stroke, brain tumor, increased intracranial pressure).
- Retina Specialist (Vitreoretinal Surgeon): For specific retinal conditions like retinal detachment, diabetic retinopathy, macular degeneration.
Prompt evaluation is key, especially for sudden vision loss, new visual field defects, or signs of increased intracranial pressure.
References
- Miller NR, Newman NJ, Biousse V, Kerrison JB. Walsh and Hoyt's Clinical Neuro-Ophthalmology. 6th ed. Lippincott Williams & Wilkins; 2005. (Comprehensive reference).
- American Academy of Ophthalmology. Basic and Clinical Science Course (BCSC), Section 5: Neuro-Ophthalmology. San Francisco, CA: American Academy of Ophthalmology. (Published annually).
- American Academy of Ophthalmology. Basic and Clinical Science Course (BCSC), Section 12: Retina and Vitreous. San Francisco, CA: American Academy of Ophthalmology. (Published annually).
- Yanoff M, Duker JS. Ophthalmology. 5th ed. Elsevier; 2019.
- Optic Neuritis Study Group. The clinical profile of optic neuritis. Experience of the Optic Neuritis Treatment Trial. Arch Ophthalmol. 1991 Dec;109(12):1673-8.
- Hayreh SS. Ischemic optic neuropathies. Springer; 2011.
- Wong TY, Mitchell P. Hypertensive retinopathy. N Engl J Med. 2004 Nov 25;351(22):2310-7.
- Foroozan R, Buono LM, Savino PJ, Sergott RC. Acute demyelinating optic neuritis. Curr Opin Ophthalmol. 2002 Dec;13(6):375-80.
See also
- Anatomy of the nervous system
- Spinal disc herniation
- Pain in the arm and neck (trauma, cervical radiculopathy)
- The eyeball and the visual pathway:
- Anatomy of the eye and physiology of vision
- The visual pathway and its disorders
- Eye structures and visual disturbances that occur when they are affected
- Retina and optic disc, visual impairment when they are affected
- Impaired movement of the eyeballs
- Nystagmus and conditions resembling nystagmus
- Dry Eye Syndrome
- Optic nerve and retina:
- Meningioma of the optic nerve sheath
- Opto-chiasmal arachnoiditis
- Optic nerve atrophy
- optic neuritis у взрослых
- optic neuritis у детей
- Ишемическая optic nerve neuropathy
- Компрессионная optic nerve neuropathy
- edema of the optic disc
- Псевдоedema of the optic disc
- optic nerve neuropathy токсическая, пищевая
- Neuropathies and neuralgia:
- Diabetic, alcoholic, toxic and small fiber sensory neuropathy (SFSN)
- Facial nerve neuritis (Bell's palsy, post-traumatic neuropathy)
- Fibular (peroneal) nerve neuropathy
- Median nerve neuropathy
- Neuralgia (intercostal, occipital, facial, glossopharyngeal, trigeminal, metatarsal)
- Post-traumatic neuropathies
- Post-traumatic trigeminal neuropathy
- Post-traumatic sciatic nerve neuropathy
- Radial nerve neuropathy
- Tibial nerve neuropathy
- Ulnar nerve neuropathy
- Tumors (neoplasms) of the peripheral nerves and autonomic nervous system (neuroma, sarcomatosis, melanoma, neurofibromatosis, Recklinghausen's disease)
- Carpal tunnel syndrome
- Ulnar nerve compression in the cubital canal