Post-traumatic neuropathies
- Understanding Post-Traumatic Neuropathies
- Diagnosis of Traumatic Neuropathy (Traumatic Neuritis)
- Treatment of Traumatic Neuropathy
- Specific Examples of Post-Traumatic Neuropathies
- Differential Diagnosis of Symptoms Following Trauma
- Prognosis and Potential Complications
- When to Consult a Specialist (Neurologist, Neurosurgeon)
- References
Understanding Post-Traumatic Neuropathies
Post-traumatic neuropathies are disorders of peripheral nerves (or nerve roots, though "neuropathy" typically refers to peripheral nerves) that occur as a direct consequence of mechanical trauma or injury to the nerve. This trauma can lead to a range of structural and functional nerve damage, resulting in motor, sensory, and sometimes autonomic disturbances in the area innervated by the affected nerve(s).
Definition and Common Causes of Nerve Trauma
Mechanical trauma to a nerve can occur through various mechanisms, including:
- Surgical Procedures: Iatrogenic nerve injury during operations near nerve pathways.
- Direct Injuries:
- Impacts, contusions, or blows directly to a nerve or the area where it runs superficially.
- Lacerations or penetrating wounds that sever or damage nerve tissue.
- Post-injection neuritis/neuropathy: Nerve injury resulting from improper intramuscular or perineural injection of drugs, where the needle directly traumatizes the nerve or the injected substance causes chemical irritation/damage.
- Compression or Entrapment:
- Prolonged clamping or pressure on a nerve (e.g., during surgery, from tight casts or bandages, or due to sustained awkward postures - "Saturday night palsy" is an example affecting the radial nerve).
- Nerve entrapment by scar tissue, hematoma, or callus formation following fractures.
- Fractures and Joint Dislocations: Bone fractures (e.g., humerus, fibula, tibia) or joint dislocations can stretch, compress, or directly sever adjacent nerves due to their anatomical proximity.
- Stretch/Traction Injuries: Sudden forceful stretching of a limb or nerve plexus (e.g., brachial plexus injuries during birth or accidents).
Traumatic neuritis (inflammation of the nerve due to trauma) is a common finding in these injuries.
Traumatic neuropathy of the ulnar nerve can occur in conjunction with a fracture of the ulna, particularly near the elbow where the nerve is vulnerable.
Mechanisms and Types of Nerve Injury (e.g., Neuropraxia)
Peripheral nerve injuries are classified by severity (Sunderland or Seddon classifications). **Neuropraxia** is the mildest form, representing a temporary blockage of nerve conduction without axonal damage (e.g., from transient compression). Nerve impulse transmission is disrupted, usually for an average of 6-8 weeks, after which full recovery is typical. More severe injuries involve axonal damage (axonotmesis) or complete nerve transection (neurotmesis), with correspondingly poorer prognoses for spontaneous recovery.
General Symptoms Based on Nerve Damage Level
Post-traumatic neuropathies, depending on the specific nerve(s) involved, the anatomical level of the injury, and the type/severity of nerve damage, will manifest in a variety of symptoms:
- Motor Disorders: Weakness (paresis) or complete loss of voluntary movement (paralysis) in a particular muscle or group of muscles innervated by the damaged nerve.
- Sensory Changes: These can include:
- Negative Symptoms: Numbness (hypoesthesia or anesthesia), decreased sensation to touch, pain, or temperature.
- Positive Symptoms: Paresthesias (abnormal spontaneous sensations like tingling, "pins and needles," or "chills"), dysesthesias (unpleasant abnormal sensations, which can be spontaneous or evoked), hyperalgesia (increased sensitivity to painful stimuli), or allodynia (perception of pain from normally non-painful stimuli). Perversion of sensation refers to distorted sensory perception.
- Autonomic Disturbances: Changes in sweating, skin color, or temperature in the affected area if autonomic fibers within the nerve are damaged.
- Trophic Changes: Long-term consequences of denervation, such as muscle atrophy, skin thinning, nail changes, and poor wound healing.
Post-traumatic neuropathies causing persistent pain symptoms (neuralgia), hypesthesia (decreased sensation), or muscle paresis (decreased strength) often require time and patience but can respond well to appropriate treatment, especially if addressed early.
It's important to note that injuries to large nerves like the sciatic nerve are rarely complete (total transection). More often, a particular portion or fascicular group within the nerve (e.g., peroneal division of the sciatic nerve) suffers more extensive damage than other parts.
Diagnosis of Traumatic Neuropathy (Traumatic Neuritis)
A thorough diagnostic evaluation is essential to confirm traumatic neuropathy, determine the location and severity of nerve damage, and rule out other conditions. Symptoms of damage to any peripheral nerve in traumatic neuritis typically consist of a combination of motor, reflex, sensory, and sometimes vasomotor-secretory-trophic disorders.
Clinical Evaluation and Neurological Examination
Examination of a patient with suspected traumatic neuritis traditionally begins with the meticulous collection of anamnestic information (detailed medical history), including:
- Mechanism, timing, and circumstances of the trauma.
- Onset and progression of symptoms (pain, weakness, sensory changes).
- Previous injuries or neurological conditions.
A comprehensive neurological examination will assess:
- Motor function: Muscle strength grading in all relevant muscle groups, observation for atrophy or fasciculations.
- Sensory function: Testing for light touch, pinprick, temperature, vibration, and proprioception in the suspected nerve distribution.
- Reflexes: Deep tendon reflexes (e.g., biceps, triceps, brachioradialis, patellar, Achilles).
- Tinel's sign: Tapping along the course of the nerve may elicit paresthesias distally if the nerve is irritated or regenerating.
- Inspection for wounds, scars, deformities, or signs of autonomic dysfunction.
Electrodiagnostic Studies (ENG/NCS and EMG)
Classical electrodiagnostic testing (ENG/NCS and EMG) plays a crucial role in the comprehensive study of a patient with traumatic neuritis, typically performed from 2 weeks onwards after the injury. These tests help to:
- Objectively confirm and quantify nerve damage.
- Differentiate between degenerative (axonal loss) and non-degenerative (demyelinating/conduction block) disorders.
- Localize the site of injury along the nerve or within a plexus.
- Assess the severity of the injury.
- Provide prognostic information: Closed damage to nerve trunks, particularly complex structures like the brachial plexus, if accompanied by significant axonal degeneration on EMG/NCS, always carries a doubtful prognosis regarding the completeness and quality of restoration of lost movements, especially in the distal parts of the limb.
Restoration of movements to a functional strength (e.g., 4–5 points on the MRC scale) after traumatic neuritis is generally observed only in those muscles where classical electrodiagnostics reveal reduced electroexcitability or a reaction of partial nerve degeneration (indicating some viable axons). If a reaction of complete degeneration of the nerve is found, spontaneous restoration of movement in the affected muscles is typically not observed.
In very late periods after nerve damage in traumatic neuritis (months to years), the identification of complete loss of electrical excitability of the paralyzed muscles (no response on EMG/NCS) provides an additional strong reason in favor of declining or reconsidering surgical intervention on the nerves, as the target muscles may be irreversibly atrophied and fibrosed. It has been observed that, sometimes earlier than in other areas, the electrical excitability of the muscles on the dorsum of the forearm (e.g., wrist extensors) can disappear. Contrary to some conventional wisdom, the small intrinsic muscles of the hand often turn out to be more resilient in terms of their ability to respond to electrical stimulation by current, even after significant proximal nerve injury.
Electromyography (EMG) is a very promising research and diagnostic method for closed injuries, such as those affecting the brachial plexus, as it allows for the recording and monitoring of the dynamics of changes in the neuromuscular apparatus during the recovery process in traumatic neuritis. The appearance of previously absent motor unit action potentials (MUAPs) on a follow-up EMG can indicate reinnervation and make it possible to expect the restoration of movement long before the first clinical signs of such recovery are evident.
Imaging Studies
- X-rays: To identify associated bone fractures or dislocations.
- CT Scan: For more detailed assessment of bony injuries or complex fractures.
- MRI: To visualize the injured nerve directly (in some cases), detect hematomas, soft tissue injuries, or signs of muscle denervation. MR neurography is a specialized MRI technique for imaging peripheral nerves.
- Ultrasound (High-Resolution): Can visualize nerves, identify sites of compression, discontinuity, or neuromas, and guide injections.
Treatment of Traumatic Neuropathy
Treatment for traumatic neuropathy is tailored individually to each case, considering the specific nerve injured, the mechanism and severity of trauma, the time since injury, and the patient's overall condition. The primary aim is to optimize nerve recovery and restore function.
General Principles and Conservative Management
Many closed traumatic neuropathies, especially milder forms like neuropraxia or mild axonotmesis, may recover spontaneously with conservative care.
- Observation: For closed injuries with no evidence of nerve transection, an initial period of observation (weeks to months) with regular clinical and electrophysiological monitoring is often appropriate to allow for spontaneous recovery.
- Immobilization/Splinting: To protect the injured nerve and limb, prevent further injury, support paretic muscles, and prevent contractures (e.g., wrist drop splint for radial neuropathy, AFO for foot drop).
- Pain Management: Analgesics, NSAIDs, or neuropathic pain medications (gabapentin, pregabalin, TCAs) as needed.
- Physical Therapy: Crucial for maintaining range of motion in affected joints, preventing contractures, and later, for muscle strengthening and re-education as reinnervation occurs.
- Occupational Therapy: To adapt daily activities and provide assistive devices.
Pharmacological Treatment
- Corticosteroids: A short course may be considered in some acute traumatic neuropathies to reduce inflammation and edema around the nerve, but their efficacy is not universally established for all types of traumatic nerve injury.
- Vitamins: B-complex vitamins (group "B"), Vitamin C ("C"), and Vitamin E ("E") are often prescribed as supportive therapy for nerve health and regeneration.
- Homeopathic Remedies: Some patients explore these options, though scientific evidence for their efficacy in promoting nerve recovery is generally limited.
Rehabilitative Therapies
- Acupuncture: Can be very effective in managing pain associated with traumatic neuropathy and is explored by some for promoting nerve recovery.
- Nerve Stimulation and Muscle Stimulation:
- Transcutaneous Electrical Nerve Stimulation (TENS) for pain relief.
- Neuromuscular Electrical Stimulation (NMES) to maintain muscle viability and prevent severe atrophy in denervated muscles while awaiting reinnervation. Neurostimulation through physiotherapy can help eliminate paresthesias and pain, and support muscle strength restoration in traumatic neuropathy.
Surgical Intervention
Surgical treatment is indicated in specific scenarios:
- Open Wounds with Nerve Laceration: Early exploration and direct nerve repair (neurorrhaphy) or grafting is usually recommended.
- Known Nerve Entrapment or Compression: By bone fragments, hematoma, scar tissue, or foreign bodies that require surgical release (neurolysis of the nerve trunk, etc.).
- Failure of Spontaneous Recovery: If, after an adequate period of observation for a closed injury (typically 3-6 months), there is no clinical or electrophysiological evidence of nerve regeneration, surgical exploration may be considered to assess the nerve and perform neurolysis, nerve grafting, or nerve transfers.
- Progressive Neurological Deficit Despite Conservative Care.
The decision for surgery, the timing, and the specific procedure (e.g., neurolysis, nerve suturing/grafting) are complex and depend on many factors, best determined by a surgeon experienced in peripheral nerve injuries.
Specific Examples of Post-Traumatic Neuropathies
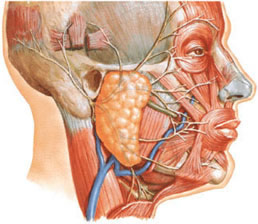
As highlighted in the images and text, specific nerves are prone to traumatic injury due to their anatomical course:
- Radial Nerve Neuropathy: Commonly associated with humerus fractures ("Damage to the radial nerve at the site of the fracture of the humerus").
- Ulnar Nerve Neuropathy: Can occur with ulna fractures or elbow trauma ("Traumatic neuropathy of the ulnar nerve with a fracture of the ulna").
- Fibular (Peroneal) Nerve Neuropathy: Vulnerable with fibula fractures, especially at the fibular head ("Traumatic fibular (peroneal) nerve neuropathy with fibular fracture").
- Tibial Nerve Neuropathy: Can result from tibia fractures or knee/ankle trauma ("Traumatic neuropathy of the tibial nerve with a fracture of the tibia").
- Sciatic Nerve Neuropathy: Can be caused by hip dislocations, pelvic fractures, or deep gluteal injuries/injections ("Post-traumatic sciatic nerve neuropathy, when compressed by a scar, causes a 'lumbago' pain throughout the leg").
- Trigeminal Nerve Neuropathy: Can occur from facial trauma or iatrogenically during dental procedures like conduction anesthesia ("Traumatization of the trigeminal nerve... leads to traumatic neuropathy"). This can involve branches like the infraorbital nerve ("Neuropraxia of the infraorbital nerve... as a result of its damage with blunt trauma").
- Facial Nerve Neuropathy: Vulnerable at its exit from the skull or within the temporal bone due to fractures or compression ("At the point of its exit from the cranial cavity, the facial nerve is most often subject to traumatic compression...").
Differential Diagnosis of Symptoms Following Trauma
When neurological symptoms appear after trauma, it's important to differentiate direct nerve injury from other potential causes:
| Condition | Key Differentiating Features |
|---|---|
| Post-Traumatic Peripheral Neuropathy | Symptoms (weakness, sensory loss, pain) localized to the distribution of a specific peripheral nerve. Clear history of trauma to the nerve's course. EMG/NCS confirms peripheral nerve lesion. |
| Radiculopathy (Nerve Root Injury) | Often due to traumatic disc herniation or vertebral fracture. Pain, weakness, and sensory loss in a dermatomal/myotomal pattern. Neck or back pain common. Reflex changes specific to root level. Spinal imaging (MRI/CT) diagnostic. |
| Plexopathy (Brachial or Lumbosacral Plexus Injury) | Trauma (stretch, compression, penetrating) to the plexus. More widespread neurological deficits involving multiple nerve distributions in a limb. EMG/NCS helps localize to the plexus. |
| Spinal Cord Injury | Bilateral deficits below the level of injury, upper motor neuron signs (spasticity, hyperreflexia, Babinski) often present. Bowel/bladder dysfunction common. Spinal imaging crucial. |
| Compartment Syndrome | Often after crush injury or fracture. Severe pain out of proportion to injury, tenseness of muscle compartment, pain with passive stretch, paresthesias, pulselessness (late sign). Requires urgent fasciotomy. Nerve damage can be secondary. |
| Musculoskeletal Injury (Tendon/Ligament Rupture, Muscle Contusion) | Localized pain, swelling, bruising, instability. Weakness due to pain or structural damage rather than primary nerve lesion. No primary sensory loss unless a nerve is also injured. |
| Vascular Injury with Ischemia | Trauma can damage blood vessels leading to limb ischemia. Symptoms: pain, pallor, pulselessness, paresthesias, paralysis (the "5 Ps"). Neurological deficits are secondary to ischemia. |
| Complex Regional Pain Syndrome (CRPS) | Can develop after trauma. Severe pain (often burning, out of proportion to initial injury), swelling, skin color/temperature changes, abnormal sweating, trophic changes, motor dysfunction. Diagnosis often clinical. |
Prognosis and Potential Complications
The prognosis for post-traumatic neuropathies is highly variable and depends on:
- Type and Severity of Nerve Injury (Sunderland/Seddon classification):
- Neuropraxia (conduction block without axonal damage): Excellent prognosis, full recovery usually within weeks to 3 months.
- Axonotmesis (axonal damage, endoneurial sheath intact): Good potential for recovery through axonal regeneration (approx. 1 mm/day), but can be slow and incomplete.
- Neurotmesis (complete nerve transection or severe disruption): Poor prognosis without surgical repair; recovery often incomplete even with surgery.
- Mechanism of Injury: Sharp transections repaired early tend to do better than crush or severe stretch injuries.
- Location of Injury: More proximal injuries have a longer distance for axons to regenerate.
- Timeliness and Appropriateness of Treatment.
- Patient Factors: Age, overall health, comorbidities (e.g., diabetes).
Potential complications include:
- Persistent motor weakness or paralysis.
- Chronic neuropathic pain or dysesthesias.
- Permanent sensory loss.
- Muscle atrophy.
- Joint contractures and deformities.
- Development of traumatic neuromas (painful stump neuromas).
- Complex Regional Pain Syndrome (CRPS).
- Functional disability and impaired quality of life.
Prevention Strategies
While many traumatic events are accidental, some preventive measures include:
- Adherence to safety regulations in workplaces and during recreational activities.
- Use of appropriate protective gear during sports or hazardous tasks.
- Careful surgical technique to minimize iatrogenic nerve injury during operations.
- Proper landmarking and technique for intramuscular injections to avoid direct nerve trauma.
- Awareness of vulnerable nerve positions during prolonged immobilization or anesthesia.
When to Consult a Specialist (Neurologist, Neurosurgeon)
Following any significant trauma associated with new neurological symptoms, prompt medical evaluation is essential. Consultation with a neurologist, neurosurgeon specializing in peripheral nerve surgery, or a physiatrist is recommended if:
- There is clear motor weakness (paresis/paralysis) or significant sensory loss in the distribution of a nerve after trauma.
- An open wound suggests possible nerve laceration.
- Symptoms do not improve or worsen after an initial observation period for closed injuries.
- Severe or persistent pain (neuralgia) develops.
- Electrodiagnostic studies indicate severe axonal loss or complete denervation with no signs of early recovery.
- A compressive lesion (e.g., hematoma, bone fragment) is identified on imaging.
Early and accurate diagnosis, coupled with timely and appropriate intervention (conservative or surgical), is crucial for maximizing the potential for nerve recovery and functional outcome after traumatic neuropathies.
References
- Seddon HJ. Three types of nerve injury. Brain. 1943;66(4):237-288. (Classical classification of nerve injuries).
- Sunderland S. A classification of peripheral nerve injuries producing loss of function. Brain. 1951;74(4):491-516. (Detailed classification).
- Campbell WW. Evaluation and management of peripheral nerve injury. Clin Neurophysiol. 2008 Sep;119(9):1951-65.
- Kline DG, Hudson AR. Nerve Injuries: Operative Results for Major Nerve Injuries, Entrapments, and Tumors. 2nd ed. WB Saunders; 2008.
- Robinson LR. Traumatic injury to peripheral nerves. Muscle Nerve. 2000 Jun;23(6):863-73.
- Kim DH, Kline DG. Management and results of extensive traumatic longitudinal nerve injuries including the brachial plexus and lumbosacral plexus. Neurosurgery. 2004 Jul;55(1):136-46; discussion 146-7.
- Stewart JD. Focal Peripheral Neuropathies. 3rd ed. Lippincott Williams & Wilkins; 2000. (Chapters on specific nerve injuries).
- Preston DC, Shapiro BE. Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic Correlations. 3rd ed. Elsevier Saunders; 2013. (Relevant chapters on electrodiagnosis of traumatic neuropathies).
See also
- Anatomy of the nervous system
- Spinal disc herniation
- Pain in the arm and neck (trauma, cervical radiculopathy)
- The eyeball and the visual pathway:
- Anatomy of the eye and physiology of vision
- The visual pathway and its disorders
- Eye structures and visual disturbances that occur when they are affected
- Retina and optic disc, visual impairment when they are affected
- Impaired movement of the eyeballs
- Nystagmus and conditions resembling nystagmus
- Dry Eye Syndrome
- Optic nerve and retina:
- Compression neuropathy of the optic nerve
- Edema of the optic disc (papilledema)
- Ischemic neuropathy of the optic nerve
- Meningioma of the optic nerve sheath
- Optic nerve atrophy
- Optic neuritis in adults
- Optic neuritis in children
- Opto-chiasmal arachnoiditis
- Pseudo-edema of the optic disc (pseudopapilledema)
- Toxic and nutritional optic neuropathy
- Neuropathies and neuralgia:
- Diabetic, alcoholic, toxic and small fiber sensory neuropathy (SFSN)
- Facial nerve neuritis (Bell's palsy, post-traumatic neuropathy)
- Fibular (peroneal) nerve neuropathy
- Median nerve neuropathy
- Neuralgia (intercostal, occipital, facial, glossopharyngeal, trigeminal, metatarsal)
- Post-traumatic neuropathies
- Post-traumatic trigeminal neuropathy
- Post-traumatic sciatic nerve neuropathy
- Radial nerve neuropathy
- Tibial nerve neuropathy
- Trigeminal neuralgia
- Ulnar nerve neuropathy
- Tumors (neoplasms) of the peripheral nerves and autonomic nervous system (neuroma, sarcomatosis, melanoma, neurofibromatosis, Recklinghausen's disease)
- Carpal tunnel syndrome
- Ulnar nerve compression in the cubital canal