Lipoma (fatty tumor)
Understanding Lipomas (Fatty Tumors)
Definition and Origin
A lipoma, often referred to as a fatty tumor or colloquially as a "wen" (though "wen" can also refer to other cyst types), is a common benign (non-cancerous) tumor composed of mature adipose tissue cells (fat cells). These tumors typically develop within the subcutaneous adipose tissue layer, which is the layer of fat located just beneath the skin. Lipomas can occur almost anywhere on the body where fat cells are present, including the face, abdomen, back, neck, shoulders, arms, and thighs.
While the exact initial cause of a single lipoma often involves the atypical proliferation of fat cells, some theories suggest they might arise from pre-existing "atypical" fat cells laid down embryologically (from birth), which later begin to grow. However, most lipomas develop sporadically in adulthood.
Causes and Pathogenesis of Lipomas
The precise cause of most solitary lipomas is unknown. However, for lipomas and the condition of multiple lipomas (lipomatosis), several factors and theories are considered:
- Genetic Predisposition: Familial cases of multiple lipomatosis with an autosomal dominant inheritance pattern are described, suggesting a genetic component in some individuals. Certain genetic syndromes, like Gardner syndrome or Madelung's disease (multiple symmetric lipomatosis), are associated with lipoma formation.
- Metabolic Factors: A systemic impairment of metabolic processes in adipose tissue is thought to play a role in the development of lipomas and lipomatosis. The occurrence of subcutaneous lipomas might be associated with a localized defect in the lipolysis process (the breakdown of fatty deposits under the skin) or abnormal fat cell proliferation.
- Trauma: Some evidence suggests that minor trauma or injury to an area might trigger the formation of a lipoma ("post-traumatic lipoma"), possibly by causing adipose tissue herniation or inflammation that stimulates fat cell growth.
Lipomatosis and Associated Conditions
Associated Medical Conditions: The role of diseases affecting the liver or pancreas, as well as hypofunction of the thyroid gland or pituitary gland, are debated as potential contributing factors to lipoma and lipomatosis development. Often, lipomas and lipomatosis can develop due to or against the background of conditions such as:
- Alcoholism
- Diabetes mellitus
- Obesity
- Dyslipidemia (abnormal lipid levels)
- Rarely, they may be associated with malignant tumors of the upper respiratory tract, though this is not a direct causal link for typical subcutaneous lipomas.
Lipomas are generally encapsulated tumors, meaning they are surrounded by a thin fibrous capsule that separates them from the surrounding healthy tissue.
Clinical Presentation and Diagnosis of Lipomas
Common Locations and Characteristics
Lipomas are typically located wherever adipose tissue is present, most commonly in the subcutaneous layer. Favorite sites for subcutaneous lipomas (wens) include:
- Back
- Neck (especially posterior neck)
- Shoulders
- Upper and lower extremities (arms and thighs)
- Scalp (though less common than pilar cysts here)
- Face
- Abdomen
On physical examination, a typical subcutaneous lipoma presents as:
- A soft, doughy, or rubbery-feeling nodule or "knot" under the skin.
- Usually well-defined, though some may have less distinct boundaries.
- Painless in most cases. Pain may occur if the lipoma compresses a nearby nerve or if it undergoes infarction or inflammation (rare).
- Mobile under the skin, not typically fixed or welded to underlying tissues or the overlying skin itself.
- The skin over the lipoma is usually unchanged in color and texture.
- Size can vary from very small (pea-sized) to quite large (several centimeters or more). They tend to grow slowly over months or years.
Differentiating Lipomas from Atheromas (Epidermoid Cysts)
In appearance, subcutaneous atheromas (more accurately, epidermoid or pilar cysts) and lipomas can be very similar. However, a doctor can often distinguish them based on subtle indirect signs and palpation:
- Location: Lipomas are generally located in areas with abundant subcutaneous fatty tissue. Atheromas (epidermoid/pilar cysts) are more common in areas with a high concentration of sebaceous glands or hair follicles (e.g., scalp, face, back, chest).
- Central Punctum: Upon close examination, an epidermoid cyst often has a visible central punctum (a tiny dark spot representing the blocked opening of the hair follicle). Lipomas do not have a punctum.
- Consistency and Attachment: Both formations can feel soft. However, an atheroma (epidermoid/pilar cyst) is often part of the skin, being tethered to it, especially at the punctum. A lipoma is a deeper, subcutaneous formation that typically does not adhere to the surface of the skin and often feels more "slippery" or lobulated under palpation.
While clinical examination is often sufficient for diagnosis of typical superficial lipomas, imaging studies like ultrasound or MRI may be used for larger, deeper, or atypical lesions to confirm the fatty nature and rule out other types of soft tissue tumors. Biopsy is rarely needed unless malignancy (liposarcoma, which is rare) is suspected.
Treatment of Lipomas
Indications for Treatment
Treatment for subcutaneous lipomas is generally elective, as they are benign. The only definitive treatment is surgical excision. Indications for removal include:
- Cosmetic concerns: If the lipoma is unsightly or bothersome to the patient.
- Pain or Discomfort: If the lipoma is tender, painful, or presses on adjacent nerves.
- Functional Impairment: If the lipoma's size or location interferes with movement or daily activities.
- Rapid Growth or Change in Characteristics: To rule out rare malignant transformation (liposarcoma) or other pathology.
- Diagnostic Uncertainty: If the diagnosis is not entirely clear based on clinical examination alone.
Surgical Excision of Lipomas
If the subcutaneous lipomas are very large, the operation is best performed in a hospital or surgical center setting, though it can still be an outpatient procedure. If the lipoma under the skin is small and uncomplicated, the removal operation is commonly performed on an outpatient basis in a clinic or doctor's office. The operation to remove a subcutaneous lipoma is typically performed under local anesthesia.
Stages of Lipoma Removal Surgery
The typical surgical procedure for lipoma removal involves the following steps:
- Anesthesia: The area is cleansed with an antiseptic solution, and local anesthetic (e.g., lidocaine with epinephrine) is injected around and beneath the lipoma to numb the area.
- Incision: A skin incision is made directly over the lipoma. The length of the incision is usually minimized but must be adequate to allow for complete removal. Incisions are often planned along natural skin lines or creases to optimize the cosmetic outcome.
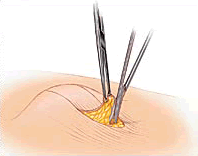
- Dissection and Removal: The surgeon carefully dissects the lipoma from the surrounding subcutaneous tissue. Lipomas are usually well-encapsulated and can often be "shelled out" or removed by gentle blunt dissection and traction. Sometimes, the fatty accumulation is simply removed. It is important to remove the entire lipoma to prevent recurrence.
- Hemostasis: Any small bleeding vessels are controlled (e.g., with electrocautery or pressure).
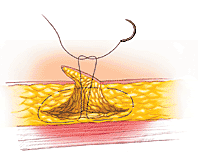
- Wound Closure: The skin wound is then sutured. This may involve one or two layers of sutures:
- Deep Sutures (if needed): Absorbable sutures may be used to close the deeper subcutaneous dead space if the lipoma was large.
- Skin Sutures: The skin edges are approximated with non-absorbable or absorbable sutures.
- Dressing: A sterile dressing is applied.
Skin healing after lipoma removal surgery typically occurs within 7-10 days. At the end of this period, non-absorbable skin sutures are removed by a healthcare professional. Absorbable sutures will dissolve on their own.
Alternative Treatments (Limited Use)
- Steroid Injections: Injections of corticosteroids directly into a lipoma can sometimes cause it to shrink, but they usually do not eliminate it completely. This may be an option for small lipomas where surgery is undesirable or for symptomatic relief.
- Liposuction: For larger lipomas, liposuction can be used to remove the fatty tissue through a small incision. However, it may be more difficult to ensure complete removal of the entire lipoma and its capsule with this method, potentially leading to a higher recurrence rate compared to formal excision.
These alternative treatments are generally less definitive than surgical excision.
Differential Diagnosis of Subcutaneous Lumps
While lipomas are common, other subcutaneous lumps must be considered in the differential diagnosis:
| Condition | Key Differentiating Features |
|---|---|
| Lipoma | Soft, doughy, mobile, painless subcutaneous fatty tumor. Not attached to skin. No punctum. Slow growing. |
| Epidermoid Cyst (Sebaceous Cyst) | Firm or fluctuant, often with a central punctum, filled with keratin. Tethered to skin. Can become inflamed. |
| Pilar Cyst (Trichilemmal Cyst) | Smooth, firm, mobile, most common on scalp. No punctum. Thicker wall. Filled with keratin. |
| Angiolipoma | Similar to lipoma but often tender or painful due to vascular component. Histologically different. |
| Neurofibroma | Soft, fleshy, often compressible ("buttonhole sign"). May be associated with neurofibromatosis. |
| Abscess | Painful, erythematous, warm, fluctuant collection of pus. Signs of acute inflammation. |
| Hematoma (Organized) | Collection of blood, often after trauma. May become firm over time. Skin may be bruised. |
| Dermatofibroma | Firm, often slightly raised or depressed papule/nodule. "Dimple sign" (retracts with lateral pressure). |
| Liposarcoma (Malignant) | Rare. Often larger (>5 cm), rapidly growing, may be firm, fixed to deeper tissues, or painful. Requires imaging and biopsy for diagnosis. |
| Metastatic Nodule | Firm, rapidly growing nodule in a patient with a known history of cancer. |
Potential Complications and Recurrence
Lipomas are benign and generally do not cause serious medical problems. Potential issues are usually related to their size, location, or cosmetic appearance:
- Pain or Discomfort: If a lipoma compresses a nearby nerve or is in an area prone to pressure.
- Cosmetic Concerns.
- Functional Limitation: Very large lipomas can sometimes interfere with movement.
- Recurrence: Recurrence after surgical excision is uncommon if the entire lipoma, including its capsule, is removed. Incomplete removal can lead to regrowth. Liposuction has a higher recurrence rate.
- Complications of Removal: Standard surgical risks like bleeding, infection, scar formation, or temporary numbness around the incision site.
- Malignant Transformation: Extremely rare for a benign lipoma to transform into a liposarcoma. Most liposarcomas arise de novo. However, any rapidly growing or unusually firm "lipoma" should be evaluated carefully.
When to Seek Medical Attention
Medical advice from a dermatologist, general practitioner, or surgeon should be sought if a subcutaneous lump:
- Is rapidly growing or changing in appearance.
- Becomes painful, tender, red, or warm.
- Is hard or fixed to underlying tissues.
- Is very large (>5 cm).
- Causes functional problems or cosmetic distress.
- The diagnosis is uncertain.
While most lipomas are harmless, a proper diagnosis is important to rule out other, more serious conditions.
References
- Salam GA. Lipoma excision. Am Fam Physician. 2002 Mar 1;65(5):901-4.
- Weiss SW, Goldblum JR. Enzinger and Weiss's Soft Tissue Tumors. 6th ed. Mosby Elsevier; 2013. (Chapter on Benign Lipomatous Tumors).
- Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016. (Chapter on Benign Skin Tumors).
- Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F, eds. WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. IARC Press; 2013.
- Aust MC, Spies M, Kall S, Gohritz A, Boorboor P, Koller M, Vogt PM. Lipomas after soft tissue trauma: are they real? Analysis of 31 cases. Br J Dermatol. 2007 Jul;157(1):92-9.
- Nigam Y, Knight J. Anatomy and physiology of the skin. Nurs Times. 2007 Nov 20-26;103(47):26-7. (General skin context).
- Kolb L, Yarrarapu SNS, Kasi A. Lipoma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
See also
- Abscess
- Breast diseases (mastopathy, cyst, calcifications, fibroadenoma, intraductal papilloma, cancer)
- Bursitis
- Furuncle (boil)
- Ganglion cyst
- Hidradenitis suppurativa (HS)
- Ingrown toenail
- Lipoma (fatty tumor)
- Lymphostasis
- Paronychia, panaritium (whitlow or felon)
- Sebaceous cyst (epidermoid cyst)
- Tenosynovitis (infectious, stenosing)