Paronychia, panaritium (whitlow or felon)
- Understanding Panaritium (Felon/Whitlow)
- Paronychia (Inflammation of the Nail Fold)
- Types of Panaritium Based on Location and Depth
- Diagnosis of Paronychia and Panaritium
- General Principles of Treatment for Panaritium
- Differential Diagnosis of Finger Infections/Inflammation
- Complications and Prevention
- When to Seek Medical Attention
- References
Understanding Panaritium (Felon/Whitlow)
Definition and Pathogenesis
Panaritium, also commonly known as a felon or whitlow, is an acute purulent (pus-forming) inflammation affecting the tissues of a finger or, less commonly, a toe. This infection typically develops when pyogenic (pus-producing) bacteria, most often *Staphylococcus aureus*, enter the finger tissues through a minor break in the skin, such as an injection site (e.g., from a splinter or needle stick), abrasion, small cut, crack, hangnail, or other forms of microtrauma.
The unique anatomy of the palmar surface of the fingers contributes to the characteristics of these infections. Here, the skin is firmly connected to the underlying palmar aponeurosis and tendon sheaths by strong fibrous septa (tendon bridges). These septa create multiple small, closed fascial compartments or channels. When infection occurs within these confined spaces, the accumulating pus and inflammatory edema lead to a rapid increase in tissue pressure. This increased pressure can compress the small blood vessels (feeding vessels) supplying the area, leading to ischemia (reduced blood flow) and subsequent tissue necrosis (death). This anatomical arrangement facilitates the rapid spread of infection inwards towards deeper structures like tendons, joints, and bones if not treated promptly.
Importance of Early Intervention
If there is a suspicion of an infectious process on the finger consistent with panaritium, a "wait-and-see" approach is unacceptable and dangerous. Delay can lead to rapid progression of infection, tissue necrosis, and involvement of deeper structures, potentially resulting in permanent functional impairment or even loss of the digit. Early surgical intervention, involving incision and drainage of pus along with the obligatory removal of any necrotic tissues, is often necessary to control the infection and prevent severe complications.
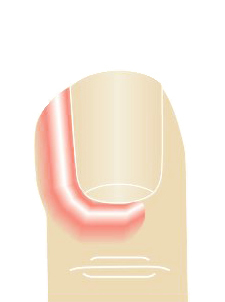
Paronychia (Inflammation of the Nail Fold)
Causes and Symptoms
Paronychia is an inflammation of the periungual fold, which is the soft tissue surrounding the fingernail or toenail (the nail bed or periungual roller). Common causes of paronychia include:
- Superficial trauma during a manicure or pedicure (e.g., from cuticle pushing or trimming).
- Tearing off hangnails (agnails).
- Nail biting.
- Frequent immersion of hands in water or exposure to irritants.
- Ingrown nails.
These can create an entry point for bacteria (commonly *Staphylococcus aureus* or Streptococci) or sometimes fungi (e.g., *Candida albicans* in chronic paronychia). With paronychia, symptoms include redness, swelling, pain, and tenderness in the area of the nail fold. Pus may accumulate under the skin fold and can sometimes be seen or expressed from under the edge of the nail or cuticle.
Treatment of Paronychia
- Initial Stages (Conservative): If there is no frank pus collection, treatment may include:
- Warm soaks in water with Epsom salts or an antiseptic solution (e.g., dilute potassium permanganate baths, chlorhexidine).
- Application of topical antibiotics or antiseptics.
- Keeping the area clean and dry.
- Pus Formation (Suppurative Stage): When pus is present (abscess formation), surgical treatment of paronychia is necessary. This usually involves:
- Incision and drainage of the pus collection, often by gently lifting the nail fold away from the nail plate or making a small incision.
- Systemic antibiotics may be prescribed if there is significant cellulitis or if the patient is immunocompromised.
Paronychia can be complicated by the development of a subungual panaritium (felon under the nail) if the infection spreads beneath the nail plate.
Types of Panaritium Based on Location and Depth
Panaritium is classified based on the anatomical location and depth of the purulent inflammation. Each type has characteristic symptoms and requires specific management.
Subungual Felon (Subungual Panaritium)
Subungual panaritium is a collection of pus located directly beneath the nail plate. It commonly occurs as a result of:
- Suppuration (infection) of subungual hematomas (blood clots under the nail, often from trauma).
- Penetrating foreign bodies under the nail.
- Extension of infection from a paronychia (inflammation of the periungual ridge).
Symptoms include severe, throbbing pain under the nail, a sensation of pressure, and sometimes visible pus accumulation or "swimming" (lifting or discoloration) of the nail plate. Pus may be released from under the free edge or sides of the nail plate.
Treatment of subungual felon is promptly surgical. It necessitates removal of part or all of the nail plate to allow for adequate drainage of the pus and debridement of infected tissue. This may involve trephination (drilling a hole in the nail) for small collections or partial/complete nail avulsion for more extensive infections.
Cutaneous Felon (Skin Panaritium)
Cutaneous panaritium involves a collection of pus located superficially under the epidermis (the outermost layer of skin), often forming a limited blister or vesicle filled with pus. This type more frequently occurs due to minor microtrauma or the entry of small foreign bodies into the skin.
With cutaneous panaritium, an accumulation of pus is determined directly beneath the epidermis. The pain syndrome is typically not as sharp or severe as with deeper forms of panaritium. Treatment involves unroofing or deroofing the blister – removing the overlying epidermis – which usually leads to rapid recovery if the infection is truly superficial. After removing the epidermis, it is crucial to carefully examine the base of the abscess. Sometimes, a small fistulous tract (opening) leading to deeper parts of the finger may be visible at the bottom. This indicates that the cutaneous panaritium might be a manifestation of a deeper "collar-button" or "cufflink" abscess, where the main purulent focus is actually a subcutaneous panaritium that has tracked to the surface.
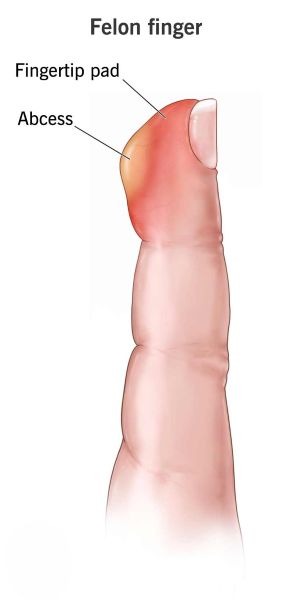
Subcutaneous Panaritium
Subcutaneous panaritium is a common form of purulent inflammation affecting the subcutaneous fatty tissue of the finger, typically on the palmar aspect. Key symptoms include:
- Pronounced, throbbing, or "twitching" pain, which is often constant and severe.
- Localized tenderness, most intense over the site of suppuration, but generally outside the direct projection of the tendons.
- Swelling and redness of the affected part of the finger.
This form often localizes on the distal phalanx (fingertip), creating a felon. The classic description of "the first sleepless night" due to intense pain is often an indication for surgical intervention. Delaying surgery for subcutaneous panaritium risks the spread of inflammation to deeper structures, such as bone (osteomyelitis) or joints (septic arthritis).
Tendon Panaritium (Infectious Tenosynovitis)
Tendon panaritium, or infectious flexor tenosynovitis, is a serious infection involving the synovial sheath that surrounds the flexor tendons of the finger. It often results from the spread of a subcutaneous panaritium inwards or from a direct penetrating injury to the tendon sheath.
Classic signs (Kanavel's signs) include:
- Fusiform (sausage-shaped) swelling of the entire affected finger.
- The finger is held in a slightly flexed (bent) position at rest.
- Intense pain along the course of the affected tendon sheath on palpation.
- Exquisite pain on passive extension (straightening) of the finger. This is often the most sensitive sign.
Delay in surgical treatment for tendon panaritium can lead to tendon necrosis, adhesions, and permanent loss of finger function. Infections of the tendon sheaths of the thumb (I finger) and little finger (V finger) are particularly dangerous because their synovial sheaths often communicate proximally with the radial and ulnar bursae in the palm, respectively. Inflammation can spread along these pathways, leading to a U-shaped phlegmon (horseshoe abscess) of the hand, potentially extending into the forearm (Parona's space). The prognosis for tendon panaritium is often unfavorable without aggressive and timely surgical drainage and debridement.
Articular Panaritium (Septic Arthritis of Finger Joint)
Articular panaritium is a purulent inflammation (suppuration) of the articular capsule and joint space of an interphalangeal or metacarpophalangeal joint of the finger. It is more often a complication arising from a subcutaneous panaritium (due to delayed or incorrectly performed surgery for subcutaneous panaritium) or from direct penetrating trauma into the joint.
Symptoms include:
- Sharp swelling and redness localized around the affected joint.
- Severe pain on palpation of the joint.
- Marked pain with any attempted movement of the joint, and particularly with axial loading (stretching along the axis of the finger) or distraction.
Conservative treatment for articular panaritium (e.g., joint aspiration with antibiotic lavage) may be attempted only in the very earliest stages. With increasing pain and in later stages, surgical treatment (arthrotomy for drainage and debridement) is necessary. The prognosis for articular panaritium is often unfavorable regarding joint function, with risks of ankylosis (joint stiffness) or destruction.
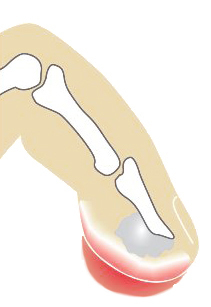
Bone Panaritium (Osteomyelitis of Phalanges)
Bone panaritium, or osteomyelitis of a phalanx, is an infection of the bone of the finger. It most often localizes to the distal (nail) phalanx.
Clinical features include:
- Bulbous or club-like swelling of the affected phalanx, particularly the fingertip.
- Pain on palpation over the involved bone.
- Sometimes, bone crepitus (a grating sensation) may be determined if there is significant bone destruction or sequestrum formation.
- Persistent purulent discharge from a sinus tract if the infection has spread from a chronic subcutaneous or articular panaritium.
Radiographic examination (X-ray) in established bone panaritium will reveal signs of osteomyelitis, such as bone erosion, periosteal reaction, or the presence of a sequestrum (a piece of dead bone). Treatment of bone panaritium is primarily surgical, involving debridement of infected and necrotic bone (sequestrectomy), along with prolonged antibiotic therapy.
Diagnosis of Paronychia and Panaritium
The diagnosis of most forms of paronychia and panaritium is primarily clinical, based on the characteristic history and physical examination findings:
- History: Inquire about recent minor trauma, manicures, hangnails, splinter injuries, or any conditions predisposing to infection (e.g., diabetes, immunocompromise). Note the onset, duration, and nature of pain.
- Physical Examination:
- Inspection for redness, swelling, blisters, pustules, or draining sinus tracts. Note the exact location of maximal tenderness and swelling.
- Palpation to assess for fluctuance (indicating pus collection), induration, tenderness, and crepitus (in bone panaritium).
- Assessment of range of motion of finger joints and pain on passive extension (for suspected tendon sheath infection).
- Careful probing of any draining sinus tracts (with a sterile, blunt probe) can sometimes help determine depth and direction.
- Imaging:
- X-rays: Indicated if bone panaritium (osteomyelitis) or articular panaritium (septic arthritis) is suspected, or to look for radiopaque foreign bodies. X-rays can show bone erosion, sequestra, periosteal reaction, or joint space changes.
- Ultrasound: Can be useful for identifying fluid collections (abscesses) in subcutaneous tissue or tendon sheaths, and can guide aspiration or drainage.
- MRI: May be used in complex cases, suspected deep space infections, or if osteomyelitis is suspected but X-rays are inconclusive.
- Laboratory Tests:
- Gram Stain and Culture: Aspirated pus or tissue samples should be sent for Gram stain, aerobic and anaerobic bacterial cultures, and antibiotic susceptibility testing to guide antibiotic therapy.
- White Blood Cell Count (WBC) and Inflammatory Markers (ESR, CRP): May be elevated, indicating infection and inflammation, especially with more severe or systemic involvement.
General Principles of Treatment for Panaritium
The overarching principles for treating all forms of panaritium are:
- Early Diagnosis and Intervention: Crucial to prevent progression to deeper tissues and irreversible damage.
- Drainage of Pus: Any collection of pus must be adequately drained surgically.
- Debridement of Necrotic Tissue: Removal of all dead or devitalized tissue is essential for infection control and healing.
- Appropriate Antibiotic Therapy: Systemic antibiotics are usually required, initially often empiric (covering common pathogens like *Staphylococcus* and *Streptococcus*) and then tailored based on culture and sensitivity results.
- Immobilization and Elevation: Resting the affected hand/finger and elevating it can help reduce swelling and pain.
- Pain Management.
- Hand Therapy and Rehabilitation: After the acute infection resolves, hand therapy may be needed to restore range of motion, strength, and function, especially after tendon, joint, or bone involvement.
The specific surgical approach and antibiotic regimen will vary depending on the type and severity of the panaritium.
Differential Diagnosis of Finger Infections/Inflammation
Painful, swollen, and red conditions of the finger can arise from various causes:
| Condition | Key Differentiating Features |
|---|---|
| Paronychia/Panaritium (Felon) | History of minor trauma, localized pain, redness, swelling at nail fold (paronychia) or fingertip pulp (felon). Fluctuance and pus if abscess formed. Throbbing pain characteristic. |
| Herpetic Whitlow | Viral infection (HSV-1 or HSV-2) of the fingertip. Presents with grouped vesicles on an erythematous base, intense pain, burning, or tingling. Often recurrent. Tzanck smear positive for multinucleated giant cells. |
| Cellulitis | Spreading inflammation of skin and subcutaneous tissue without a discrete pus collection (initially). Area is red, warm, swollen, tender. Borders often indistinct. |
| Insect Bite or Sting (Inflamed) | History of bite/sting. Localized swelling, intense itching, redness. Central punctum may be visible. Can become secondarily infected. |
| Gout or Pseudogout (Crystal Arthropathy) | Acute onset of severe joint pain, redness, swelling (often affects a single joint, e.g., interphalangeal). Aspiration may show crystals (urate for gout, CPPD for pseudogout). |
| Contact Dermatitis (Irritant or Allergic) | Itching, redness, vesicles, scaling due to exposure to an irritant or allergen. Often follows pattern of exposure. |
| Traumatic Injury (without infection initially) | Bruising, swelling, pain localized to site of injury. Hematoma may form. Less likely to have signs of purulence unless secondarily infected. |
| Glomus Tumor (Subungual) | Rare benign tumor under the nail. Causes severe, paroxysmal pain, often triggered by cold. Localized tenderness, bluish discoloration under nail possible. |
Complications and Prevention
Potential complications of paronychia and panaritium if not treated adequately include:
- Spread of infection to deeper tissues (tendons, joints, bone).
- Tendon necrosis and loss of finger function (in tendon panaritium).
- Joint destruction and ankylosis (in articular panaritium).
- Osteomyelitis leading to bone loss or chronic infection.
- Nail deformities or loss (with paronychia or subungual felon).
- Lymphangitis and lymphadenitis.
- Bacteremia and sepsis (rare but possible with severe infections).
- Chronic pain or stiffness.
- Amputation of the digit (in very severe, neglected cases).
Prevention involves:
- Careful hand and nail hygiene.
- Avoiding biting nails or picking at cuticles/hangnails.
- Using sterile instruments for manicures/pedicures.
- Wearing protective gloves when working with hands to prevent minor injuries.
- Prompt cleaning and antiseptic application to any minor cuts, abrasions, or splinters on fingers.
- Good control of underlying conditions like diabetes that increase infection risk.
When to Seek Medical Attention
Medical attention should be sought promptly if:
- Signs of infection around a nail or on a fingertip develop (redness, swelling, increasing pain, pus).
- The pain is severe, throbbing, or keeps you awake at night.
- There is fever or general malaise associated with a finger infection.
- The finger is held in a flexed position and is extremely painful to straighten (suggests tendon sheath infection).
- Symptoms do not improve with home care (e.g., warm soaks for early paronychia) within 1-2 days, or worsen.
- There is a penetrating injury to the finger.
- The individual has diabetes, is immunocompromised, or has poor circulation.
Early diagnosis and appropriate treatment by a healthcare professional (often a primary care physician, dermatologist, hand surgeon, or emergency physician) are crucial for preventing serious complications from these common but potentially debilitating finger infections.
References
- Clark DC. Common acute hand infections. Am Fam Physician. 2003 Nov 15;68(10):2167-76.
- Ong YS, Levin LS. Hand infections. Plast Reconstr Surg. 2009 Aug;124(2):225e-233e.
- Shafritz AB, Coppage JP. Acute and chronic paronychia. J Am Acad Orthop Surg. 2014 Mar;22(3):165-74.
- Patel DB, Emmanuel NB, Stevanovic MV, et al. Acute Hand Infections. J Am Acad Orthop Surg. 2014 Jul;22(7):435-44.
- Rockwell PG. Acute and chronic paronychia. Am Fam Physician. 2001 Mar 15;63(6):1113-6.
- Neviaser RJ. Infections of the hand. Instr Course Lect. 1983;32:85-94.
- Hausman MR, Lisser SP. Hand infections. Orthop Clin North Am. 1992 Oct;23(4):171-85.
- Abrams RA, Botte MJ. Hand infections: a current concepts review. J Hand Surg Am. 1996 Jan;21(1):8-15.
See also
- Abscess
- Breast diseases (mastopathy, cyst, calcifications, fibroadenoma, intraductal papilloma, cancer)
- Bursitis
- Furuncle (boil)
- Ganglion cyst
- Hidradenitis suppurativa (HS)
- Ingrown toenail
- Lipoma (fatty tumor)
- Lymphostasis
- Paronychia, panaritium (whitlow or felon)
- Sebaceous cyst (epidermoid cyst)
- Tenosynovitis (infectious, stenosing)