Treatment of transient ischemic attack (TIA) in common carotid artery basin
Anticoagulation therapy
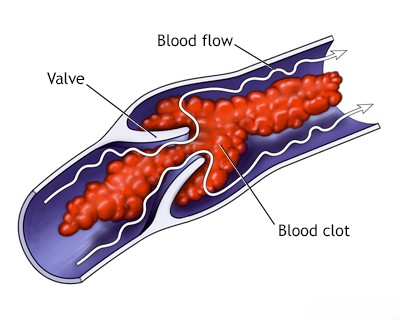
In patients experiencing Transient Ischemic Attacks (TIAs) suspected to be caused by severe stenosis or near-occlusion of the Internal Carotid Artery (ICA) or Middle Cerebral Artery (MCA), the optimal acute medical management strategy is crucial but can be complex [1]. While immediate initiation of antiplatelet therapy is standard practice [2], the role of acute anticoagulation with heparin has been debated [1]. Historically, heparin was sometimes used empirically in high-risk situations, such as crescendo TIAs (multiple frequent TIAs) or suspected ongoing thrombus formation/propagation, with the goal of preventing imminent stroke while awaiting definitive diagnosis or intervention [1]. However, robust evidence demonstrating the superiority of acute heparin over antiplatelet therapy in this setting is lacking [1, 2]. Furthermore, anticoagulation carries an inherent risk of bleeding, including hemorrhagic conversion of any potential small infarcts [1]. Therefore, the decision to use acute heparin for TIAs related to large artery stenosis is generally made on a case-by-case basis by specialists, weighing the perceived risk of imminent stroke against the risks of anticoagulation, and it is not considered routine initial therapy [1, 2].
The role of long-term oral anticoagulation (like warfarin) for secondary stroke prevention after Transient Ischemic Attacks (TIAs) related specifically to atherosclerotic stenosis of the carotid or middle cerebral arteries (i.e., non-cardioembolic causes) is highly controversial and generally *not* the standard of care compared to antiplatelet therapy [1, 2]. Evaluating the effectiveness of anticoagulation for this indication based on older studies is challenging due to limitations including [1]:
- Lack of adequate randomization comparing anticoagulants directly against modern antiplatelet regimens.
- Often small numbers of patients in specific subgroups.
- Inconsistent diagnostic criteria and methods for determining TIA etiology across studies.
Interpretation of some older studies may also be confounded by the inclusion of patients whose symptoms were not truly ischemic or were potentially due to causes other than large artery atherosclerosis [1].
Current guidelines strongly favor antiplatelet agents for long-term secondary prevention in patients with TIAs or ischemic strokes attributed to large artery atherosclerosis [2]. While historically anticoagulation was sometimes considered for patients deemed unsuitable for surgical or endovascular revascularization (e.g., due to inaccessible lesions like high carotid siphon stenosis or MCA stenosis), antiplatelet therapy is now the mainstay in such cases, unless a compelling separate indication for anticoagulation exists (e.g., concurrent atrial fibrillation) [1, 2].
For severe symptomatic intracranial stenosis (such as significant MCA stenosis), major clinical trials (like SAMMPRIS [3]) have demonstrated that intensive medical management, including dual antiplatelet therapy (aspirin and clopidogrel) for an initial period (e.g., 90 days) followed by long-term single antiplatelet therapy, combined with aggressive risk factor control (especially blood pressure and lipids), is superior to endovascular stenting and is the recommended approach [3]. Long-term anticoagulation is generally not recommended for this indication due to lack of proven benefit over antiplatelets and increased bleeding risk [1, 3].
Therapeutic anticoagulation carries significant bleeding risks [1]. Absolute contraindications are situations where the bleeding risk clearly outweighs potential benefits, and generally include [1]:
- Active, clinically significant bleeding.
- Severe uncontrolled hypertension.
- Recent major trauma or surgery (especially intracranial or spinal).
- High risk of intracranial hemorrhage (e.g., recent large infarct with hemorrhagic conversion risk, known cerebral amyloid angiopathy).
- Severe thrombocytopenia or known coagulopathy.
- Severe liver disease with impaired coagulation.
Relative contraindications require careful individual risk-benefit assessment and include factors like [1]:
- Advanced age.
- Moderate or difficult-to-control hypertension.
- History of significant gastrointestinal or other bleeding.
- High fall risk.
- Chronic kidney disease.
- Concurrent use of other medications affecting bleeding risk (e.g., NSAIDs).
Short-term anticoagulation with heparin may occasionally be considered in the acute setting for specific high-risk scenarios, such as crescendo TIAs presumed secondary to critical carotid stenosis, potentially as a bridge while awaiting urgent revascularization (e.g., endarterectomy or stenting) [1]. However, this is not routine practice, requires careful patient selection, and must balance the perceived thrombotic risk against the immediate bleeding risk [1, 2].
Platelet antiaggregation therapy
Antiplatelet therapy is the cornerstone of medical management for preventing recurrent ischemic events after a Transient Ischemic Attack (TIA) or minor ischemic stroke attributed to non-cardioembolic causes (such as large artery atherosclerosis or small vessel disease) [1, 2]. While the efficacy of any secondary prevention strategy is subject to ongoing research and refinement, the fundamental benefit of antiplatelet agents is well-established, unlike the more controversial role of anticoagulants for these specific indications [1, 2]. Acetylsalicylic acid (aspirin) is the most extensively studied antiplatelet agent for this purpose [2]. Numerous randomized controlled trials have evaluated aspirin monotherapy as well as aspirin in combination with other antiplatelet agents (such as clopidogrel or dipyridamole) [2, 4]. These studies have consistently demonstrated that antiplatelet therapy, including aspirin alone, significantly reduces the risk of recurrent TIA, stroke, and other vascular events in patients presenting with ischemic cerebrovascular symptoms [2, 4]. Current guidelines often recommend initiating dual antiplatelet therapy (DAPT, typically aspirin plus clopidogrel) for a short duration (e.g., 21-90 days) in patients with high-risk TIA or minor ischemic stroke, followed by long-term single antiplatelet therapy, to further optimize early risk reduction [2, 5].
While early studies comparing aspirin to placebo after Transient Ischemic Attack (TIA) or minor stroke sometimes involved patients where the exact cause wasn't definitively determined via angiography, the overall benefit of antiplatelet therapy, particularly aspirin, in reducing recurrent non-cardioembolic ischemic events is well-established [2]. Some analyses suggested aspirin might provide more benefit in patients with confirmed atherosclerotic lesions in the carotid arteries compared to those without such lesions (where a cardioembolic source might be more likely), but antiplatelet therapy remains indicated for secondary prevention in both scenarios unless anticoagulation is required (e.g., for atrial fibrillation) [1, 2]. Comparing the risk reduction from aspirin alone (medical management) to that achieved with carotid endarterectomy (CEA) requires careful context: CEA provides a substantial risk reduction compared to medical therapy *alone* specifically in patients with *severe symptomatic* carotid stenosis (typically 70-99%, or sometimes 50-69% depending on specific factors) [6, 7].
Aspirin (or other antiplatelet agents like clopidogrel) is considered fundamental medical therapy for patients with TIA or stroke related to atherosclerosis, not merely an adjunct or alternative [2]. It is used across the spectrum of disease severity, including cases with mild stenosis, severe stenosis unsuitable for or awaiting intervention (e.g., inaccessible lesions like high carotid siphon or MCA stenosis), or following revascularization procedures [2].
Aspirin exerts its primary antiplatelet effect by irreversibly inhibiting the cyclooxygenase-1 (COX-1) enzyme within platelets [8]. This action prevents the synthesis of thromboxane A2 (TXA2), a potent promoter of platelet aggregation and vasoconstriction [8]. Aspirin also inhibits COX enzymes in endothelial cells, reducing the production of prostacyclin (PGI2), which normally inhibits platelet aggregation and causes vasodilation [8]. This latter effect is potentially undesirable, but the clinical benefit of aspirin suggests the inhibition of platelet TXA2 predominates, especially at lower doses [8].
Because the inhibition of platelet COX-1 is achieved effectively even at low doses, and higher doses may increase bleeding risk and potentially inhibit prostacyclin more significantly, standard dosages for secondary stroke prevention are typically low (e.g., 75-100 mg daily, or 81-325 mg daily depending on regional guidelines and specific clinical situations) [2, 8].
Dipyridamole is another antiplatelet agent whose mechanism involves inhibiting phosphodiesterase (increasing platelet cAMP) and potentially adenosine uptake, ultimately reducing platelet aggregation [8]. While evidence for dipyridamole monotherapy is limited, the combination of extended-release dipyridamole with aspirin has been shown in trials to be effective for secondary stroke prevention and is an established treatment option, although its use relative to other agents like clopidogrel has varied over time [2, 4].
Clopidogrel is a widely used antiplatelet agent that irreversibly inhibits the P2Y12 adenosine diphosphate (ADP) receptor on platelets, preventing ADP-mediated platelet activation and aggregation [8]. It is often used as an alternative to aspirin for patients who cannot tolerate aspirin, or in combination with aspirin (Dual Antiplatelet Therapy - DAPT) for a limited period after certain high-risk TIAs or minor strokes [2, 5]. Sulfinpyrazone has antiplatelet effects but is not a standard therapy for TIA/stroke prevention. Clofibrate is a lipid-lowering agent, and while NSAIDs like ibuprofen have some antiplatelet effect, they are not used for secondary stroke prevention and may interfere with aspirin's efficacy or increase bleeding risk [8].
Surgical therapy
Carotid endarterectomy
Carotid Endarterectomy (CEA) is a well-established surgical procedure for treating significant atherosclerotic stenosis of the internal carotid artery, particularly when it has caused symptoms like a Transient Ischemic Attack (TIA) or minor stroke [1, 9]. First performed in the 1950s, the operation involves surgically removing the plaque buildup from the artery to restore normal blood flow and, most importantly, to prevent future strokes [9]. Like any major surgery, CEA carries inherent risks, including perioperative stroke, death, cranial nerve injury, and myocardial infarction [9]. However, in experienced centers performing the procedure on appropriately selected patients, the risk of major complications like perioperative stroke or death is generally low (often cited as needing to be <6% for symptomatic patients and <3% for asymptomatic patients, though actual outcomes vary) [2, 9]. Crucially, landmark randomized controlled trials (such as NASCET [6] and ECST [7]) definitively demonstrated decades ago that for patients with severe (typically 70-99%) symptomatic carotid stenosis, CEA provides a substantial long-term benefit in reducing the risk of stroke compared to medical therapy alone [6, 7]. Benefit may also exist for carefully selected patients with moderate (50-69%) symptomatic stenosis [6]. Therefore, despite the procedural risks, CEA is considered a vital and effective treatment for stroke prevention in appropriately selected individuals, as the long-term benefits clearly outweigh the surgical risks in this high-risk population [2, 6, 7].
Patients undergoing Carotid Endarterectomy (CEA) face an increased risk of perioperative stroke if they have certain anatomical or physiological factors that compromise cerebral collateral circulation [1, 9]. These factors include severe stenosis or occlusion of the contralateral carotid artery or inadequate collateral pathways through the Circle of Willis [1]. Intraoperative neuromonitoring, such as continuous Electroencephalography (EEG) monitoring or somatosensory evoked potentials (SSEPs), is often used during the procedure [9]. Monitoring aims to detect signs of cerebral ischemia that may occur when the carotid artery is temporarily clamped [9]. If significant changes suggestive of ischemia are detected, the surgeon may elect to place a temporary shunt to maintain blood flow to the brain during the plaque removal [9].
Patients requiring CEA often have significant comorbidities, reflecting the systemic nature of atherosclerosis [9]. Arterial hypertension, coronary artery disease (CAD), and peripheral vascular disease are common [9]. Certain conditions significantly increase the risk of surgery and may represent relative or absolute contraindications [9]. These include unstable angina, recent myocardial infarction (typically within the past few months), and severe congestive heart failure or severely reduced ejection fraction [9]. While significant hypertension should ideally be controlled before elective surgery, excessive lowering of blood pressure in patients with critical carotid stenosis must be avoided, as hypotension can precipitate thrombosis at the stenotic site or cause cerebral hypoperfusion, potentially leading to ischemic stroke [1].
Restenosis, or re-narrowing of the treated segment of the carotid artery, can occur after Carotid Endarterectomy (CEA), although significant, flow-limiting restenosis is relatively uncommon [9]. Early restenosis (typically within the first 1-2 years) is often attributed primarily to neointimal hyperplasia (an excessive healing response involving smooth muscle cell proliferation and matrix deposition) [9]. Later restenosis (occurring after 2 years) is more commonly due to progressive atherosclerosis within the treated segment or adjacent areas [9]. While clinically significant restenosis may cause recurrent symptoms, repeat surgical intervention (redo CEA) is technically more challenging due to scar tissue formation from the initial operation, potentially increasing procedural risks [9]. Endovascular treatment with angioplasty and stenting is often considered an alternative for managing significant restenosis [9, 10].
Managing tandem lesions, where significant stenosis exists at both the carotid bifurcation (origin of the internal carotid artery) and more distally in the intracranial segment (e.g., the carotid siphon), presents a complex challenge [1]. Treatment decisions are highly individualized and depend on factors like the severity and location of each stenosis, the patient's symptoms, overall vascular health, and procedural risks [1]. Simple diameter measurements alone are insufficient for decision-making. Options may include CEA for the bifurcation lesion combined with intensive medical management for the siphon lesion, endovascular treatment (stenting) of one or both lesions (though intracranial stenting carries specific risks and indications [3]), or intensive medical management alone with antiplatelet agents and aggressive risk factor control [1, 2]. There is no universal consensus on the optimal approach for all tandem lesions, and management often involves multidisciplinary discussion [1].
Endovascular therapy (stenting and balloon angioplasty)
Endovascular treatment, specifically Carotid Artery Stenting (CAS) often combined with balloon angioplasty, is an established minimally invasive option for treating carotid artery stenosis, used as an alternative to Carotid Endarterectomy (CEA) in selected patients [2, 10]. It is performed by appropriately trained specialists (including interventional radiologists, neurologists, cardiologists, and vascular surgeons). CAS involves deploying a stent across the stenotic lesion to widen the artery lumen and maintain patency, thereby improving blood flow to the brain [10]. This technique can be applied to stenosis located at:
- The carotid bifurcation (where the common carotid divides into internal and external carotid arteries).
- The cervical segments of the internal carotid artery (below the skull base).
- Selected lesions in the intracranial segments of the internal carotid artery (though indications and risks differ significantly for intracranial stenting compared to extracranial CAS) [3].
Example of an atherectomy device sometimes used in endovascular treatment of peripheral or other artery diseases (related to managing atherosclerotic vascular disease). Note: Atherectomy is distinct from standard carotid stenting.
Carotid Artery Stenting (CAS) is often considered for patients who are deemed high-risk for Carotid Endarterectomy (CEA) due to specific anatomical factors (e.g., previous radical neck surgery or radiation, restenosis after prior CEA, contralateral laryngeal nerve palsy, lesion location high in the neck or below the clavicle) or significant medical comorbidities (e.g., severe cardiac or pulmonary disease) [2, 10]. During CAS, an Embolic Protection Device (EPD) is typically used to capture potential debris (emboli) dislodged during the procedure, reducing the risk of stroke [10]. Major randomized trials (like CREST [11]) have compared CAS (with EPD) and CEA [10, 11]. Key findings generally indicate that while both procedures are effective in long-term stroke prevention for appropriate candidates, there are differences in periprocedural risks: CAS tends to have a slightly higher risk of minor periprocedural stroke, whereas CEA tends to have a slightly higher risk of periprocedural myocardial infarction [11]. The overall composite risk of major events (stroke, MI, death) in the periprocedural period and long-term outcomes are often comparable between the two procedures when performed by experienced operators on suitable patients [11]. Patient age and specific risk factors influence the relative risks, and the choice between CAS and CEA requires careful individualized assessment and discussion [2, 10, 11].
Extracranial-to-intracranial bypass surgery
Extracranial-to-Intracranial (EC-IC) bypass surgery, typically involving anastomosis (connection) of a scalp artery like the Superficial Temporal Artery (STA) to a cortical branch of the Middle Cerebral Artery (MCA), was developed as a method to augment blood flow to brain regions distal to a severe stenosis or occlusion [1, 12]. Historically, this procedure was proposed for patients with symptomatic atherosclerotic disease, such as Internal Carotid Artery (ICA) occlusion or severe MCA stenosis, who continued to experience Transient Ischemic Attacks (TIAs) or minor strokes despite medical management [1]. However, a major international randomized controlled trial, the EC/IC Bypass Study published in 1985 [13], compared STA-MCA bypass surgery plus medical therapy against medical therapy alone for patients with symptomatic ICA or MCA atherosclerotic disease. The trial famously found no benefit from the surgery; patients randomized to surgery did not have a lower risk of subsequent stroke or death compared to those receiving medical therapy alone (which included antiplatelet agents available at the time) [13]. As a result of this landmark study, EC-IC bypass is generally *not* considered an effective treatment for preventing stroke related to typical intracranial or extracranial atherosclerotic occlusive disease [1, 12]. While the procedure may still have specific niche applications in neurosurgery (e.g., for Moyamoya disease, complex aneurysms requiring vessel sacrifice, certain skull base tumors), it is not standard treatment for the atherosclerotic indications originally studied in the 1985 trial [12].
The immediate management strategy following an ischemic stroke in the Internal Carotid Artery (ICA) territory depends heavily on the initial stroke severity and the time from onset [1]. In cases of large, devastating strokes presenting with severe deficits like dense hemiplegia, global aphasia, or profound neglect/anosognosia (indicating extensive infarction, often involving much of the Middle Cerebral Artery territory), the acute focus shifts from preventing immediate recurrence in that territory towards supportive care [1]. Priorities include stabilizing the patient, managing blood pressure carefully (often allowing permissive hypertension initially unless thrombolysis or thrombectomy is performed), preventing and treating complications like cerebral edema, aspiration pneumonia, and deep vein thrombosis [1, 14].
The role of acute anticoagulation (e.g., with heparin) immediately following an ischemic stroke remains controversial and is generally *not* recommended for most stroke types, particularly large ones, due to the increased risk of hemorrhagic transformation [1, 14]. While historically debated for "stroke-in-evolution" or fluctuating deficits, current practice typically favors early initiation of antiplatelet therapy [2, 14]. Intravenous thrombolysis (like alteplase) or endovascular thrombectomy are the primary hyperacute treatments aimed at reperfusion if the patient presents within the appropriate time window and meets eligibility criteria [14, 15].
Initiating anticoagulation shortly after a minor stroke or TIA in the setting of newly diagnosed severe ICA stenosis or occlusion is also generally not standard practice unless there is a clear concurrent indication (like atrial fibrillation) [1, 2]. While the theoretical goal might be to prevent thrombus propagation or early recurrence, the risk of hemorrhagic conversion of even small infarcts exists [1]. Antiplatelet therapy is the mainstay in these situations [2].
For patients who have suffered a minor stroke or TIA attributed to a severe (typically 70-99%, or sometimes 50-69% based on specific criteria), symptomatic stenosis of the ipsilateral ICA, Carotid Endarterectomy (CEA) is a well-established secondary prevention strategy [2, 6, 7]. Landmark trials (like NASCET [6] and ECST [7]) demonstrated that CEA significantly reduces the long-term risk of stroke compared to medical therapy alone in appropriately selected patients [6, 7]. The acceptable perioperative risk (stroke or death) for CEA in symptomatic patients is generally considered to be <6% in experienced centers [2]. The presence of severe contralateral carotid stenosis or occlusion can increase the perioperative risk, requiring careful assessment and planning [1, 9]. Medical management alone for severe symptomatic stenosis carries a significant risk of recurrent stroke [6, 7].
Hemorrhagic transformation of the recent infarct is a potential complication after CEA, though relatively uncommon if surgery is timed appropriately and postoperative hypertension is avoided [1, 9]. There is ongoing debate regarding the optimal timing of CEA after an acute stroke [2, 9]. While delaying surgery for several weeks (e.g., 2-6 weeks) allows for infarct stabilization and reduces bleeding risk, prolonged delay increases the risk of recurrent stroke before intervention [2]. Earlier intervention (within days to 2 weeks) may be considered, especially for patients with TIAs or very minor strokes who have stabilized, balancing the risks of surgery against the high early risk of recurrence [2].
Emergency CEA or carotid stenting for acute ICA occlusion causing major stroke is performed in highly specialized centers but is not routine; endovascular thrombectomy targeting the intracranial occlusion is the more common hyperacute intervention for large vessel occlusion stroke [14, 15]. Outcomes of any intervention in the setting of established large infarcts are often poor [1].
For patients with symptomatic ICA occlusion (rather than stenosis) causing mild to moderate stroke, long-term management typically involves antiplatelet therapy and aggressive risk factor control [1, 2]. Long-term anticoagulation is generally reserved for patients with a concurrent indication like atrial fibrillation; its routine use solely for ICA occlusion is not supported by strong evidence [1, 2]. Surgical options for ICA occlusion are limited; ECA endarterectomy is rarely indicated for stroke prevention, and EC-IC bypass is not effective for atherosclerotic disease (as discussed previously) [1, 13]. Investigating the likely mechanism (e.g., distal embolism from the stump vs. hemodynamic compromise) may influence management nuances, but antiplatelet therapy remains central [1, 2].
Managing symptomatic intracranial stenosis (e.g., carotid siphon or MCA trunk stenosis) also requires a specific approach [1, 3]. Based on trials like SAMMPRIS [3], aggressive medical management is superior to stenting for most patients with significant symptomatic intracranial stenosis [3]. This medical management includes dual antiplatelet therapy (DAPT - typically aspirin and clopidogrel) for an initial period (e.g., 90 days), followed by single antiplatelet therapy long-term, along with intensive control of blood pressure and cholesterol [3]. Long-term anticoagulation (warfarin) is generally *not* recommended for intracranial atherosclerotic stenosis due to increased bleeding risk and lack of proven benefit over antiplatelets [1, 3].
Reducing blood viscosity (hemodilution) is not a standard acute or chronic stroke treatment; while theoretically appealing, trials have not shown consistent benefit and it carries potential risks [1]. Similarly, agents like the opiate antagonist naloxone have been investigated in acute stroke but have not proven effective and are not used in standard practice [1]. The concept of the ischemic penumbra (tissue at risk around the core infarct) is central to hyperacute reperfusion therapies (thrombolysis, thrombectomy), aiming to salvage this tissue before irreversible infarction occurs [1, 14].
Ischemic events primarily affecting the Anterior Cerebral Artery (ACA) territory are less common than those in the MCA or posterior circulation territories [1]. Management typically follows general principles for ischemic stroke, including antiplatelet therapy and risk factor control, unless a specific high-risk source (like cardioembolism) dictates anticoagulation [1, 2]. Surgical options specifically targeting ACA stenosis are generally not available or indicated [1].
References
- Ropper AH, Samuels MA, Klein JP, Prasad S. Adams and Victor's Principles of Neurology. 11th ed. McGraw Hill; 2019. Chapter 34: Cerebrovascular Diseases.
- Kernan WN, Ovbiagele B, Black HR, et al; American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014 Jul;45(7):2160-236. (Or more recent updates).
- Chimowitz MI, Lynn MJ, Derdeyn CP, et al; SAMMPRIS Trial Investigators. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011 Sep 15;365(11):993-1003.
- Diener HC, Bogousslavsky J, Brass LM, et al; European Stroke Prevention Study 2. Aspirin and extended-release dipyridamole for prevention of ischemic stroke. N Engl J Med. 2006 Jun 8;354(23):2493-4; author reply 2494-5. (Example trial comparing antiplatelets).
- Johnston SC, Easton JD, Farrant M, et al; CHANCE Investigators. Clopidogrel and Aspirin in Acute Ischemic Stroke and High-Risk TIA. N Engl J Med. 2013 Jul 4;369(1):11-9. (Example DAPT trial).
- North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991 Aug 15;325(7):445-53.
- European Carotid Surgery Trialists' Collaborative Group. MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70-99%) or with mild (0-29%) carotid stenosis. Lancet. 1991 May 25;337(8752):1235-43.
- Patrono C, García Rodríguez LA, Landolfi R, Baigent C. Low-dose aspirin for the prevention of atherothrombosis. N Engl J Med. 2005 Dec 1;353(22):2373-83. (Review on aspirin mechanism/dosing).
- Greenberg MS. Handbook of Neurosurgery. 9th ed. Thieme; 2019. Chapter 41: Carotid Endarterectomy.
- Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease. Stroke. 2011 Aug;42(8):e464-540. (Covers CEA and CAS indications).
- Brott TG, Howard G, Roubin GS, et al; CREST Investigators. Long-Term Results of Stenting versus Endarterectomy for Carotid-Artery Stenosis. N Engl J Med. 2016 Mar 17;374(11):1021-31.
- Greenberg MS. Handbook of Neurosurgery. 9th ed. Thieme; 2019. Chapter 42: Extracranial-Intracranial Bypass.
- The EC/IC Bypass Study Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med. 1985 Nov 7;313(19):1191-200.
- Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-e418.
- Goyal M, Menon BK, van Zwam WH, et al; HERMES collaborators. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016 Apr 23;387(10029):1723-31.
See also
- Ischemic stroke, cerebral ischemia
- Vertebrobasilar insufficiency (VBI) with vertigo symptom
- Somatoform autonomic dysfunction
- Dizziness, stuffiness in ear and tinnitus
- Ischemic brain disease:
- Atherosclerotic thrombosis
- Atherothrombotic occlusion of internal carotid artery
- Asymptomatic carotid bifurcation stenosis with noise
- Atherothrombotic occlusion of vertebrobasilar and posterior cerebral arteries
- Atherothrombotic occlusion of posterior cerebral artery
- Atherothrombotic occlusion of vertebral and posterior inferior cerebellar arteries (PICA)
- Atherothrombotic occlusion of basilar artery
- Small-vessel stroke (lacunar infarction)
- Other causes of ischemic stroke (cerebral infarction)
- Cerebral embolism
- Spontaneous intracranial (subarachnoid) and intracerebral hemorrhage:
- Arteriovenous malformations of the brain
- Hypertensive intracerebral hemorrhage
- Cerebral arteries inflammatory diseases (cerebral arteritis)
- Giant intracranial aneurysms
- Other causes of intracerebral hemorrhage
- Lobar intracerebral hemorrhage
- Saccular aneurysm and subarachnoid hemorrhage
- Mycotic intracranial aneurysms
- Repeated cerebral artery aneurysm rupture
- Communicating hydrocephalus after intracerebral hemorrhage with ruptured aneurysm
- Cerebral vasospasm
- Cerebrovascular diseases - ischemic stroke, transient ischemic attack (TIA):
- Transient ischemic attack (TIA)
- Sigmoid sinus suppurative thrombophlebitis with thrombosis