Upper Back Pain: Causes, Diagnosis, and Treatment
Introduction to Upper Back Pain
Upper back pain, also known as thoracic pain or interscapular pain, refers to discomfort experienced in the region of the thoracic spine, between the neck and the lower back. While less common than lower back or neck pain, it can significantly impact daily activities and quality of life. The thoracic spine is designed for stability, providing protection for vital organs and less mobility than the cervical or lumbar regions. Understanding the potential causes is crucial for effective diagnosis and treatment.
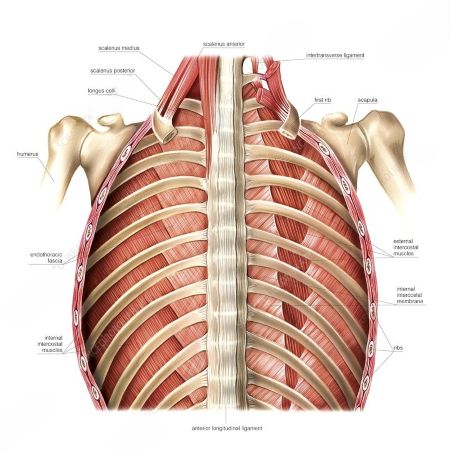
Anatomy of the Upper Back
The upper back is composed of 12 thoracic vertebrae (T1-T12), which connect to the ribs, forming the rib cage. This structure provides significant stability and protection. Key components include:
- Vertebrae: 12 bones forming the thoracic spine.
- Intervertebral Discs: Cushions between vertebrae that absorb shock. See more about Herniated and bulging intervertebral disc.
- Muscles: A complex network of muscles supports the spine and facilitates movement, including erector spinae, rhomboids, trapezius, and latissimus dorsi.
- Ligaments: Connect bones and provide stability.
- Nerves: Spinal nerves branch out from the spinal cord, innervating muscles and skin in the upper body.
Common Causes of Upper Back Pain
Musculoskeletal Issues
- Muscle Strain or Sprain: Often due to poor posture, heavy lifting, repetitive movements, or sudden injury. This is a very common cause of low back pain (spinal pain) that can also affect the upper back.
- Myofascial Pain Syndrome: Chronic pain in muscle tissue and fascia, often with trigger points.
- Poor Posture: Prolonged slouching or incorrect body mechanics can put excessive stress on the upper back muscles and ligaments, leading to poor posture related pain.
Spinal Conditions
- Disc Problems: While less common in the thoracic spine due to its rigidity, herniated and bulging intervertebral discs can occur and compress nerves.
- Osteocondritis of the spine: Degeneration of the intervertebral discs and vertebral bodies.
- Spinal spondylosis: Degenerative changes in the vertebrae, including bone spurs.
- Spondyloarthrosis (facet joint osteoarthritis): Arthritis of the facet joints, leading to pain and stiffness.
- Compression Fracture of the Spine: Can result from trauma or osteoporosis of the spine.
- Scoliosis or Kyphosis: Abnormal spinal curvatures that can place undue stress on certain areas.
- Spondylitis (osteomyelitic, tuberculous): Inflammation of the vertebrae, often due to infection.
- Spinal Stenosis: Narrowing of the spinal canal, which can compress the spinal cord or nerves. See more about Spinal stenosis.
- Ankylosing Spondylitis (Bechterew's Disease): A chronic inflammatory disease primarily affecting the spine.
Other Causes
- Nerve Compression: Resulting from disc issues, bone spurs, or other structural problems. This can manifest as pain in the thoracic spine, intercostal neuralgia.
- Organ-Referred Pain: Pain from conditions affecting the heart, lungs, gallbladder, or esophagus can sometimes be felt in the upper back.
- Shingles: A viral infection that can cause severe nerve pain.
- Tumors: Both benign and malignant tumors can occur in the spine, spinal cord, or surrounding tissues. See Hemangiomas of the spinal cord and epidural space of the spinal canal or Non-compression oncological myelopathies.
- Spinal bacterial (purulent) epiduritis: Infection within the epidural space.
In intercostal neuralgia resulting from herpes zoster (shingles), a characteristic rash of painful blisters (vesicles) appears on the skin overlying the affected intercostal nerve(s).
Associated Symptoms
Upper back pain can manifest with various symptoms, including:
- Aching, sharp, or burning pain.
- Stiffness and reduced range of motion.
- Muscle spasms or tenderness.
- Pain that worsens with movement or prolonged sitting.
- Numbness, tingling, or weakness in the arms or legs (suggestive of nerve involvement).
- Difficulty breathing (in severe cases or with lung involvement).
Diagnosis
Diagnosis typically involves a thorough medical history, physical examination, and imaging studies if necessary. A doctor will assess posture, range of motion, muscle strength, and neurological function.
- X-rays: Can reveal bone abnormalities, fractures, or significant spinal curvature.
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues, including discs, ligaments, and the spinal cord, helpful for identifying herniated discs, inflammation, or tumors.
- CT (Computed Tomography) Scan: Offers detailed bone imaging, useful for fractures or complex bony anatomy.
- Electromyography (EMG) and Nerve Conduction Studies (NCS): Can assess nerve function and identify nerve compression.
CT and MRI of the thoracic spine is a valuable imaging technique for diagnosing various causes of pain in this region, including degenerative changes, yellow ligament ossification, fractures, or other pathologies contributing to thoracic pain or intercostal neuralgia.
Differential Diagnosis Table
Differentiating the cause of upper back pain is critical for effective treatment. This table outlines common conditions and their distinguishing features:
| Condition | Key Symptoms | Contributing Factors | Diagnostic Clues |
|---|---|---|---|
| Muscle Strain/Spasm | Localized aching, tenderness, stiffness; often acute onset. | Poor posture, heavy lifting, repetitive movements, stress. | Pain reproduced with palpation and specific movements; absence of neurological deficits. |
| Herniated Disc | Sharp, radiating pain; numbness, tingling, weakness in arms/legs. | Trauma, degenerative changes. | Neurological deficits on exam; confirmed by MRI. |
| Osteochondrosis / Spondylosis | Chronic, dull ache; stiffness, worse in mornings or after inactivity. | Aging, degenerative changes. | X-ray or MRI showing disc degeneration, osteophytes. |
| Compression Fracture | Sudden, severe pain, often after minor trauma in older adults. | Osteoporosis, trauma, metastatic cancer. | X-ray or CT scan showing vertebral collapse. |
| Scoliosis/Kyphosis | Asymmetrical shoulders/hips, visible spinal curvature, chronic pain. | Congenital, idiopathic, degenerative. | Physical exam revealing curvature; confirmed by X-ray. |
| Spondylitis | Severe localized pain, fever, chills, malaise. | Bacterial infection (e.g., tuberculosis, staph). | Elevated inflammatory markers (ESR, CRP), positive blood cultures, MRI showing vertebral infection. |
| Referred Pain (e.g., cardiac, pulmonary) | Chest pain, shortness of breath, palpitations (cardiac); cough, fever (pulmonary). | Heart disease, lung conditions, gastrointestinal issues. | Absence of spinal tenderness; positive findings on cardiac or pulmonary workup. |
Treatment Approaches
Treatment for upper back pain depends on the underlying cause and severity. Options range from conservative measures to surgical intervention.
- Conservative Management:
- Rest and Activity Modification: Avoiding activities that exacerbate pain.
- Physical Therapy: Strengthening exercises, stretching, posture correction, manual therapy. This is crucial for conditions like scoliosis and general back pain.
- Medications: Over-the-counter pain relievers (NSAIDs), muscle relaxants, or prescription pain medications.
- Heat and Cold Therapy: Applying heat can relax muscles, while cold can reduce inflammation.
- Massage Therapy: Can help relieve muscle tension and spasms.
- Acupuncture: May help manage chronic pain.
- Injections:
- Epidural Steroid Injections: Can reduce inflammation and pain if nerve compression is present.
- Facet Joint Injections: For pain originating from the facet joints (spondyloarthrosis).
- Surgical Intervention:
- Rarely needed for upper back pain. Considered for severe cases involving spinal cord compression, instability, or unrelenting pain that doesn't respond to conservative treatments, such as significant herniated discs or spinal stenosis.
Exercise for shoulder and neck muscles.
Prevention
Preventing upper back pain often involves adopting healthy lifestyle habits:
- Maintain good posture, especially when sitting or lifting.
- Engage in regular exercise that strengthens core and back muscles.
- Use proper lifting techniques.
- Maintain a healthy weight.
- Take breaks and stretch regularly if you have a sedentary job.
- Ensure your workstation is ergonomically sound.
References
- Haldeman, S., Dagenais, S., & Sari, N. (2009). The prevalence of low back pain in the United States and internationally: Estimates from the National Health and Nutrition Examination Survey (NHANES) III (1988–1994). *Spine Journal, 9*(7), 543-552.
- Bogduk, N. (2005). Clinical anatomy of the lumbar spine and sacrum (4th ed.). Edinburgh: Churchill Livingstone.
- American Academy of Orthopaedic Surgeons. (2018). *Orthoinfo: Thoracic Back Pain*. Retrieved from [https://orthoinfo.aaos.org/en/diseases--conditions/thoracic-back-pain/](https://orthoinfo.aaos.org/en/diseases--conditions/thoracic-back-pain/)
- National Institute of Neurological Disorders and Stroke. (2020). *Back Pain Fact Sheet*. Retrieved from https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Back-Pain-Fact-Sheet
- Koes, B. W., van Tulder, M. W., Ostelo, R., Burton, A. K., & Waddell, G. (2007). Clinical guidelines for the management of low back pain in primary care: an international perspective. *Spine, 32*(25), 2901-2916.
- Chou, R., Qaseem, A., Snow, V., Casey, D., Cross, T. Jr, Shekelle, P., ... & Owens, D. K. (2007). Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. *Annals of Internal Medicine, 147*(7), 478-491.
See also
- Anatomy of the spine
- Ankylosing spondylitis (Bechterew's disease)
- Back pain by the region of the spine:
- Back pain during pregnancy
- Coccygodynia (tailbone pain)
- Compression fracture of the spine
- Dislocation and subluxation of the vertebrae
- Herniated and bulging intervertebral disc
- Lumbago (low back pain) and sciatica
- Osteoarthritis of the sacroiliac joint
- Osteocondritis of the spine
- Osteoporosis of the spine
- Guidelines for Caregiving for Individuals with Paraplegia and Tetraplegia
- Sacrodinia (pain in the sacrum)
- Sacroiliitis (inflammation of the sacroiliac joint)
- Scheuermann-Mau disease (juvenile osteochondrosis)
- Scoliosis, poor posture
- Spinal bacterial (purulent) epiduritis
- Spinal cord diseases:
- Spinal spondylosis
- Spinal stenosis
- Spine abnormalities
- Spondylitis (osteomyelitic, tuberculous)
- Spondyloarthrosis (facet joint osteoarthritis)
- Spondylolisthesis (displacement and instability of the spine)
- Symptom of pain in the neck, head, and arm
- Pain in the thoracic spine, intercostal neuralgia
- Vertebral hemangiomas (spinal angiomas)
- Whiplash neck injury, cervico-cranial syndrome